- NHS West London Clinical Commissioning Group
advertisement
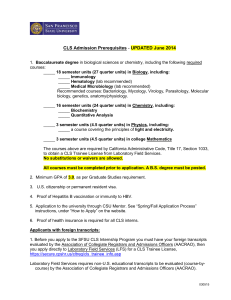
Governing Body report Paper: 5.5 Date 6 May 2014 Title of paper Commissioning Learning Sets report Presenter Dr Rachael Garner, WLCCG Author Jude Channon, Locality Manager Responsible Director Simon Hope, Deputy Managing Director Clinical Lead Dr Rachael Garner, Vice Chair Confidential No The Governing body is asked to: Note the contents of the report. Summary of purpose and scope of report This report provides an overview of the key points of discussion at the CLS meetings in March 2014 and April 2014. The main agenda items were as follows: • • March: CLSs in 2014/15; evaluation CLS plus buddying scheme; process for raising issues at Chelwest &Imperial; paeds and Paediatric A&E audit April: Practice spotlight; CLS Plan 14/15; LES/out of hospital transition; whole systems integrated care; patient experience; PCMHS; supporting workforce transformation. Soft Intelligence March NE CLS: GP raised an issue regarding a long delay in accessing the MSK service and problems with the transfer of patients from the old MSK service to new service. SE CLS: A high volume of DNAs to C&W's ultrasound service noted. It was suggested that this was due to the booking system SW CLS: Lack of follow up of results after endoscopies by secondary care Actions: MSK – The provider has liaised with the practice to investigate the patient case DNA’s to C&W’s ultrasound – The Trust has responded by indicating that a dedicated radiology referral email has been established - caw-tr.radiologyreferrals@nhs.net, the reception area has been altered so more calls can be handled and there are now extra evening and weekend appointments. Endoscopy results - PID examples sent to Trust for investigation. Chelwest has responded by indicating that they are aware of some process and staffing issues with the virtual clinic in Gastroenterology that is tasked with reviewing and informing GPs of the test results. This matter has now been rectified so the service should have improved since the Page 1 of 9 Governing Body report Paper: 5.5 beginning of the year. April NC CLS – There is an issue with CLCH’s Single Point of Access – staff finding it hard to get through over the phone. There also appear to be a large amount of duplicate imaging results being sent from St Mary’s to Practices and long waits for call back from the ‘Itchy Sneezy Wheezy ‘service. NW CLS – Confirm what proportion of patients who attend community dermatology are referred on to secondary care. SE CLS – Investigate why the service from the Memory Clinic seems to be not meeting some patient’s needs. There are also reported long waits with this service. SW CLS – Blood tests sent to Chelwest have gone missing. NE CLS – MSK would not accept a referral by fax when choose and book was down. The service does not seem to refer patients on when needed but instead sends them back to their GP to refer. A patient with chronic renal disease was rejected on the basis that not much could be done for the patient. GP unsure of where to go next. Actions: Single point of access - Locality Manager has asked practice for details on the case and will raise this with CLCH Community dermatology -18/1776 attendances have been onward referred (1%). Monitored monthly by referral destination and indication by the CCG and the Community Dermatology service provided by Chelsea &Westminster. Memory clinic - Locality Manager to raise concerns with the CCG's commissioner of the Memory Clinic and review ways in which the service can be improved. Chelwest blood tests - The practice has been asked to send details of the cases to the Locality Manager in order to follow up with the Provider. MSK Service – The service to be contacted for a response to issues raised above. Renal service – To be escalated to GP queries Results of the Paediatric A&E Audit in March • • • • • CLS groups were each given data showing Paediatric A&E Attendances per CLS by Practice Period: full year forecast outturn for 2013-14 using M6 (Sep) YTD data/6*12 Data Source: SUS Accident and Emergency Capitation List Size as at 01-07-2013 A&E Criteria: A&E Departments only, patients aged <19yrs Practices were then asked to answer a series of questions in small groups relating to how they would reduce paediatric A&E attendances. Practices were also asked to submit two plans per Practice of actions they would be taking to reduce these attendances as well as allocate tasks to specific individuals and create timelines for their plans. COLLATED RESULTS OF PAEDIATRIC A&E AUDIT MARCH 14 Page 2 of 9 Governing Body report Paper: 5.5 How many A&E attendances were in surgery hours and out of hours? Frequent attenders: in hours Out of hours Single attendance: in hours Out of hours NC 81 NW 72 NE 130 SE 100 SW 73 40% 136 147 184 127 78 60% 34 34 27 39 28 47% 27 56 56 59 34 53% For frequent attenders, were the clinical reasons for the A&E attendance quite different or was there a trend in presenting complaints? NC Yes, there 16 was a trend No, there 54 was not a trend 70 NW 32 44 76 NE Not completed Not completed SE 72 SW 25 51% 18 24 49% 0 90 49 285 For frequent attenders: by looking at the medical record on your clinical system how many GP practice attendances has the child had in 2013 (Jan - Dec)? 1-3 NC 21 NW 35 NE 23 SE 32 SW 14 4-6 7-9 10+ 16 18 17 25 17 13 26 15 18 15 17 12 9 6 7 35% 26% 21% 19% 356 For frequent attenders, what do you think the reason is for the parent taking the child to A&E instead of the GP practice? Convenience /ease of access GP practice was not open NC 5 NW 34 NE Not completed SE 2 SW 8 23% 20 15 7 8 6 26% Page 3 of 9 Governing Body report Paper: 5.5 Anxiety that GP practice would not be able to look after the child 18 41 18 18 13 51% 43 90 25 28 27 213 For the single attendance cohort, what were the typical presenting complaints? Illness Injury NC 46 NW 54 NE 49 SE 38 SW 40 57% 24 70 46 100 40 89 38 76 22 62 43% 397 For the single attendance cohort, what were the typical treatments and outcomes? Discharged following investigatio n& treatment Discharged after treatment Discharged without investigatio ns or treatment Admitted NC 8 NW 32 NE 5 SE 19 SW 3 22% 34 3 13 20 15 28% 11 22 17 15 12 26% 6 59 9 66 8 43 34 88 15 45 24% 301 For the single attendance cohort, if the GP practice could have assessed the child, what would have been the most appropriate clinical pathway? Seen by GP Referred to Paed team Advised to go to A&E NC 34 NW 52 NE 50 SE 32 SW 25 54% 4 2 9 28 10 15% 16 36 21 30 26 31% 355 Page 4 of 9 Governing Body report Paper: 5.5 For the single attendance cohort, were there any barriers to accessing the surgery for this child? Yes NC 4 NW 24 No 56 66 NE Not completed 51 60 100 51 Maybe SE 0 SW 3 9% 85 43 88% 7 92 3 49 3% 342 In summary, 1522 attendances at paediatric A&E were audited across the CCG. 60% of frequent attenders attended out of hours and 53% single attenders attended out of hours. For 51% of frequent attenders, there was a trend in the clinical reason for A&E attendance. For frequent attenders, the majority (35%) had attended their GP practice 13 times in 2013. However, approximately a quarter had attended between 4-6 times and a fifth had attended between 7 and 9 times and over 10 times! For frequent attendances, the majority (51%) were thought to have attended A&E because of anxiety that the GP practice would not be able to look after the child. For the single attendance cohort, 57% attended because of illness and 43% because of injury. For single attenders, 26% were discharged without investigation or treatment which may imply that attendance was unwarranted. However, the remaining 74% received an investigation or treatment or were admitted. For the single attendance cohort , if the GP practice could have assessed the child ,54% would have been assessed in GP, 15% referred to the Paediatric on call team and 31% advised to go to A&E. For the single attendance cohort, there were not thought to have been barriers to accessing GP in 88% of cases. A leaflet for parents is being designed, along with an Oyster card holder, which has a simple chart showing parents where they should go in different eventualities. Paediatric learning hubs are now up and running at Barlby Road, Harrow Road, New Elgin Clinic and Portland Road surgeries, with other practices attending at one of these locations. It was agreed to send out the information from these sessions to all practices, whether or not they attend, in order that learning can shared. All practices agreed to follow up inappropriate attendances with a letter, enclosing information about where they can access services. The Childrens team at the CCG is designing a template letter and awaiting patient feedback for disseminating to Practices. Other plans for reducing attendances were to educate parents during 6 week check; to provide same day access for children discuss management of paediatric cases at MDT meetings; go into schools in order to educate parents write to frequent attenders Practice Spotlight CLSs were informed of a new addition to the agenda called the Practice Spotlight. This is a 5 minute slot where Practices took turns at each CLS meeting to present something to the larger group about the work they were doing. Practices in each CLS could choose to either volunteer themselves for future dates or be allocated. The North Central CLS presented a Practice Spotlight on the structure of the new NHS via a video while a South East Practice Spotlight Page 5 of 9 Governing Body report Paper: 5.5 focussed on an experience of System 1 migration. The Practice spotlight for the North East was Foodbank. Chelwest and Imperial Process The CLSs were informed of the process for raising issues with Chelwest and Imperial relating to their services. The process described who to contact, at what level and how to keep the CCG informed of the correspondence. The CCG will keep a log of all cases to monitor the Trusts responses. Prescribing: • National forecasting model has been revised. • NHSBSA confirmed an error in November calculations • Figures unadjusted for change in APUs and expensive drug spend. • Overall still a small underspend forecasted at year end. Data shown is for Apr –Dec. CLS Plan Progress The monthly data was viewed by all CLSs. It was felt that the target for Non Elective ASC conditions was too high. It was made clear that the data did not include the 17% adjustments to RSS agreed by the Operational Group and that would have an impact on the end of year data. CLSs were also pleased that the targets would now move to rate per 1000, particularly in relation to the RSS target. Across the CLSs there was also an interest expressed in understanding how targets were set and what factors were included in the calculation of ‘weighted population’. CLS Meetings in 2014/15 The proposed 14/15 CLS plan was presented to each CLS. It is now a LIS (Local Improved Scheme) rather than a LES. Element 1 – Locality based working. There are both core and optional elements to this part of the LIS. The core element is worth a total of 3.5K to Practices and is payable if Practices have weekly in-house meetings on referrals and non-elective admissions; conduct 3 audits per year; provide 4 patient experience quarterly admissions and the CLS champions complete a template every 6 months outlining progress. Practices can also opt to earn an additional £1k by agreeing to have 4 buddy meetings per year and follow up actions from these meetings. Element 2 - Community pathways. The targets for these pathways will increase in the 14/15 CLS plan. The targets are as follows: • • • 65% of referrals to go to community dermatology 70% of referrals to go to community diabetes and community respiratory (when new services available) 90% of referrals to community MSK In addition to achieving these, element 2 also requires Practices to audit 5 referrals per year to the rapid response service and ensure appropriate use of the primary care metal health service. Full details of these are still to be confirmed. There is £150k available across all pathways for this element. Element 3 – Referral targets and non-elective admissions. There has been a change to how referral and non-elective admissions targets are set. The CCG are now using rate per 1000 to set targets. There is £150k available across the whole CCG area for the referral targets element and £300k available across the whole CCG for achieving the nonelective admissions target. Payment will be 20% CLS achievement and 80% Practice achievement. This is a significant change from the 13/14 CLS plan. Practice list sizes used to calculate the “per 1000” value will be refreshed every quarter and will use weighted list sizes not raw list sizes. Element 4 – Prescribing. There are two parts to this element. Part A (the process part) attracts a payment of £2.6k Page 6 of 9 Governing Body report Paper: 5.5 per Practice. To be eligible for this the Practice must agree an improvement and QIPP action plan with the prescribing link pharmacist by September 2014. Part B (the outcomes part) measures achievement against the prescribing quality markers and budget savings. Payment is 20% to the CLS and 80% to the Practice. ` To note: • NHSE have approved the CLS Plan • Main elements are similar to 2013/14 with some amendments • Hot topic replaced by a practice item on commissioning (practice spotlight) • CLS Plan LIS also includes Prescribing Standardisation Scheme • Co-facilitators encouraged • Shifting of CCG messages to WLCCG weekly member bulletin There was a general feeling that the frequency of meetings was too high in relation to the remuneration offered. Furthermore, CLS groups were uneasy about the steep rise in targets set for community MSK in particular. Many suggested that there were problems with the access and quality of the MSK service and this would impact on them being able to reach their targets. Others expressed an interest in being able to understand exactly how the targets are set as they felt that simply comparing them to neighbouring CCG’s was not the best way to do this. LES/Out of Hospital (OOH) services transition The process to enable re-commissioning of services by July was explained together with the timelines and the decision making groups involved. Practices would be guaranteed of their 13/14 LES income for 14/15 with the following proviso’s: • Services where notice to decommission has been given are not included in the Guarantee • This is a practice income guarantee • Practices should actively participate in the development of networks • Before new services are commissioned, practices can claim more than the ES Guaranteed Income, however, they will need to evidence the additional activity to validate claims At the point when the new OOH services are commissioned there is the opportunity to earn additional income. Where services are decommissioned or no longer provided by a practice, income is still guaranteed during 2014/2015 i.e. March 31st 2015 WLCCG Whole Systems Integrated Care Early Adopters update This process enhances the already existing PPF case management work and builds on PPF progress to date. The proposed model of care is: • • • Putting Patients First (PPF) initiative – proactive multidisciplinary case management of complex frail elderly people over 75. Emergency Admissions - older fit patients who after a hospital admission receive a new acute diagnosis such as an MI, CVA or cancer will be pro-actively case managed by an appropriate member of the MDT Urgent and Emergency Care Pathway – ensuring appropriate response for patients when they are in a crisis. Improve communication between LAS and Practices by use of System1 IT care plans to enable decisions to be made about need for admission. The focus over the next 6/8 weeks is: • Establish a WS Steering Group to ensure representation from all providers and a clear transparent decision making process. Page 7 of 9 Governing Body report Paper: 5.5 • • • • 1 GP from North and 1 GP from South Steering Group Objective; to agree an Outline Business Plan (OBP) with all Providers by May 19th and a Full Business Plan (FBP) by Oct 2014. This will include agreeing a model of care, which is co designed with service users and the development of a capitated funding model 4 workshops will be organised between now and end of May – dates to follow asap Across the CLSs there was a need expressed to understand exactly how networks would work and to generally learn a bit more about them. In the North West, there was an interest expressed in exploring how they could work together as a network and the group would ask that the CCG consider funding this dedicated time away from the Practice. In the North Central CLS questions were raised as to whether this work overlapped with the over 75 DES and the expectations for caring for Over 75’s set out in the New GP Contract. Practices questioned whether they could sign up for both the LES and the whole systems work. Patient Experience For quarter 4, 37 out of 54 practices submitted their quarterly responses and 345 individual patient responses were received, although there was variation between practices and CLSs. Overall, most patients were positive about the services they received. Just under half of the patients provided negative or OK feedback. The majority of the negative responses related to administration of appointments or attitude of staff across a range of providers. The results will be presented to the Quality, Patient Safety and Risk Committee (QPSR). There were two issues raised about maternity aftercare that raised concern namely no midwife arranged for patients when discharged. CLS Plus Buddying Scheme 16 buddy meetings have now taken place between 35 practices. 38 Practices are part of the CLS Plus scheme (92%). 1 buddy group (3 Practices) has failed to supply a meeting date despite numerous requests. Actions from the meetings are being followed-up by the locality team. Feedback from members has on the whole been very positive about the scheme and it is intended that the scheme will be continued into 2014/15 as part of the CLS Plan. Concern was raised that no-one had yet signed up to the scheme for 14/15 and that quarter 1 buddy visits may not be able to happen as a result. Primary Care Mental Health Service The PCMHS needs increased referrals from Practices. Investment in the PCMHS has led to a decrease in waiting times to 15 days across all surgeries for all treatments. The PCMHS will be changing the way it reaches out to harder to engage groups including Older Adults and BME communities. SMI (SSOC) LES Sign up SMI (shifting settings) LES aims to : • • • • Support practices to manage the transfer of patients from CNWL with safer discharge processes Provide enhanced support for stable SMI patients historically held in CMHTs Continue the commitment to shared care prescribing CCG Quality premium : Step down target Whole systems – SMI proposal Practices were asked to indicate their interest in learning more about the pilot or in being involved in developing the SMI proposal. Page 8 of 9 Governing Body report Paper: 5.5 Shaping a healthier future Practices were encouraged to discuss their workforce issues and suggest ideas for areas of investment of HENWL monies. Practice nursing was seen as an area needing more resources in terms of training and recruitment as well as customer service training and HR. It was made clear that mandatory training was not included in what would be commissioned as this was the responsibility of the employer (the Practice) to provide. Practices and CLSs were encouraged to send their ideas to the workforce and transformation team. Quality & Safety/ Patient Engagement/ Impact on patient services: N/A Financial and resource implications N/A Equality / Human Rights / Privacy impact analysis N/A Risk N/A Supporting documents N/A Governance and reporting (list committees, groups, or other bodies that have discussed the paper) Committee name Date discussed Outcome N/A Page 9 of 9