Buprenorphine in the Treatment of Opioid Addiction
advertisement
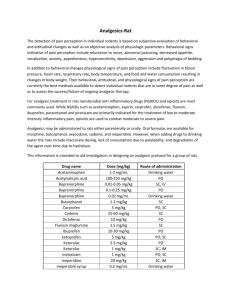
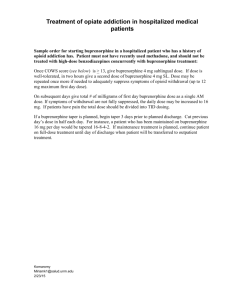
CAT Project – Addiction treatment with buprenorphine Evidence Based Practice Critically Appraised Topic Buprenorphine in the treatment of opioid addiction Carrie DeFoe, RN, BSN, FNP-S University of Mary DeFoe 1 CAT Project – Addiction treatment with buprenorphine DeFoe 2 Evidenced Based Practice Critically Appraised Topic: Buprenorphine in the treatment of opioid dependence. Date: March 6, 2014 Clinical Scenario A 31-year-old male presents to the clinic for help with his opioid addiction and has heard of the drug Subutex. He says that he wants to get off the painkillers because is engaged with a baby on the way and he “finally” has a good job. The patient tells you that he has tried “stopping cold turkey but the withdrawals were too bad.” He also reports trying counseling in the past without success. Clinical Question In patients with opioid addiction, does pharmacologic subutex (buprehnorphine) therapy versus methadone or placebo ameliorate opioid withdrawal symptoms and prevent relapse? Articles Gowing, L. (2009). Buprenorphine for the management of opioid withdrawal. Cochrane Database Of Systematic Reviews, (3), doi:10.1002/14651858.CD002025.pub4 Mattick, R. (2014). Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Of Systematic Reviews, (2), doi:10.1002/14651858.CD002207.pub4 Summary and Appraisal of Key Evidence Study 1 Gowing (2009) states that opioid dependence is a major health issue in our society, especially in the 15 to 34 year age group, mostly due to its high mortality rate, transmission of HIV and Hepatitis C, health care costs, crime costs, and law enforcement costs. The article states that detoxification alone is not an effective treatment option for opioid dependence. This Cochrane review used randomized and quasi-randomized controlled clinical trials involving participants who were primarily opioid dependent and who underwent managed withdrawal. The review focused on experimental interventions using buprenorphine compared to tapering doses of other medications such as methadone, alpha2-adrenergic agonists, placebo, or various buprenorphine doses. Trials were retrieved from electronic database searches including: The Cochrane Central Register of Controlled Trials, MEDLINE, EMBASE, and PsycINFO. The review utilized twenty-two studies involving 1736 participants. A total of 956 participants were treated with buprenorphine. The comparisons considered in this study were diverse, comparing buprenorphine to methadone, clonidine, lofexidine, and various rates of buprenorphine dose reduction. Meta-analysis was possible for only two comparisons: buprenorphine versus methadone and buprenorphine versus clonidine. The risk of assessment bias for objective outcomes was considered low for all studies. The risk assessment bias for subjective outcomes included intensity of withdrawal, occurrence and severity of adverse effects. Duration and completion of therapy were identified as potential biases but none of the studies were found to have a high risk of bias as a result of missing data. CAT Project – Addiction treatment with buprenorphine DeFoe 3 The study concluded that both buprenorphine and methadone medications have similar capacities to ameliorate withdrawal symptoms. Neither medication was found to have severe adverse effects when used for the management of opioid withdrawal. In regards to completion of treatment, buprenorphine was found to have higher completion rates than methadone but more research is needed. When compared to clonidine, buprenorphine was associated with greater retention and completion of treatment. Also, low dose buprenorphine was found to be more effective than clonidine at ameliorating withdrawal symptoms. Clinical evidence was not graded in this review. Strengths and weakness can be evaluated. A majority of the studies included in this review were performed during inpatient stays, limiting useful data for outpatient treatment of opioid addiction. Dosages of buprenorphine taper were varied among studies and participants. The studies included were evaluating the effectiveness in patients withdrawing from heroin but not other opiates. Study 2 In a Cochrane Database of Systematic Reviews, Mattick (2014) evaluated buprenorphine treatment versus placebo and as an alternative to methadone in the management of opioid dependence. Selection criteria included randomized control trials of buprenorphine maintenance treatment versus placebo or methadone in opioid dependent persons. The review included 31 trials involving 5430 participants. Participants in the studies were addicted to either heroin or other opiates. Electronic searches were conducted using CENTRAL, The Cochrane Library, and EMBASE. The interventions in the studies ranged from two to fifty-two weeks. A large number of the studies used fix doses of medication creating some limitations because common clinical practice involves flexible dosing. Three of the studies used a very low dose Buprenorphine, 1 mg, as the placebo. The review felt this was a conservative dose and unlikely to bias the results. All studies involved were judged to be low risk of bias. This review concluded that buprenorphine is an effective maintenance therapy when compared to placebo. Methadone maintenance therapy at flexible doses, when compared to buprenorphine, was found to be more effective in retaining participants in treatment (high quality, grade 4 evidence). The review supported buprenorphine in substitution maintenance and found it to be relatively safe. There was moderate evidence (grade 3) showing no difference between buprenorphine and methadone when participants’ urine drug screens tested positive for cocaine, morphine, and benzodiazepine. Also, the numbers of self reported heroin use during the studies showed no difference between the two medications (grade 3). Results Both Cochrane reviews compared buprenorphine to methadone in the management of opioid withdrawal, specifically in heroin withdrawal. Buprenorphine was consistently found to be as effective as methadone in ameliorating withdrawal symptoms. Mattick (2014) found methadone to have higher completion of treatment rate. Gowing (2009) found Buprenorphine to relieve withdrawal symptoms faster and have a higher rate of treatment completion. Adverse effects with the two drugs are minimal in both studies. Gowing (2009) compared buprenorphine to Clonidine and buprenorphine to be more effective. Mattick (2014) compared buprenorphine to placebo and concluded that buprenorphine was more effective. CAT Project – Addiction treatment with buprenorphine DeFoe 4 Clinical Bottom Line Both methadone and buprenorphine are effective treatments for opioid withdrawal and addiction management. It is up to clinical judgment to determine which medication is best suited for an individual patient. Both medications are opioids themselves and carry a high risk for abuse. Implications for Practice Based on the above studies, I would recommend either buprenorphine or methadone for the treatment of opioid withdrawal and management. Buprenorphine-licensed physicians are the only providers who can prescribe and manage buprenorphine treatment. Referral to a pain management provider is vital to success of opioid withdrawal. Both of these medications must be monitored closely with frequent follow up and urine drug screening. CAT Project – Addiction treatment with buprenorphine DeFoe References Gowing, L. (2009). Buprenorphine for the management of opioid withdrawal. Cochrane Database Of Systematic Reviews, (3), doi:10.1002/14651858.CD002025.pub4 Mattick, R. (2014). Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Of Systematic Reviews, (2), doi:10.1002/14651858.CD002207.pub4 5