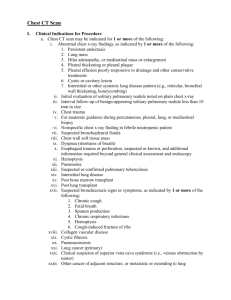
Chest CT Scan - Health Care LA

HCLA Clinical Practice Protocols Chest CT Scan Rev. Date 2015-10-30
Chest CT Scan
I.
Clinical Indications for Procedure a.
Chest CT scan may be indicated for 1 or more of the following: i.
Abnormal chest x-ray findings, as indicated by 1 or more of the following:
1.
Persistent atelectasis
2.
Lung mass
3.
Hilar adenopathy, or mediastinal mass or enlargement
4.
Pleural thickening or pleural plaque
5.
Pleural effusion poorly responsive to drainage and other conservative treatments
6.
Cystic or cavitary lesion
7.
Interstitial or other systemic lung disease pattern (e.g., reticular, bronchial wall thickening, honeycombing) ii.
Initial evaluation of solitary pulmonary nodule noted on plain chest x-ray iii.
Interval follow-up of benign-appearing solitary pulmonary nodule less than 10 mm in size iv.
Chest trauma v.
For anatomic guidance during percutaneous, pleural, lung, or mediastinal biopsy vi.
Nonspecific chest x-ray finding in febrile neutropenic patient vii.
Suspected bronchopleural fistula viii.
Chest wall soft tissue mass ix.
Dyspnea (shortness of breath) x.
Esophageal trauma or perforation, suspected or known, and additional information required beyond general clinical assessment and endoscopy xi.
Hemoptysis xii.
Pneumonia xiii.
Suspected or confirmed pulmonary tuberculosis xiv.
Interstitial lung disease xv.
Post bone marrow transplant xvi.
Post lung transplant xvii.
Suspected bronchiectasis signs or symptoms, as indicated by 1 or more of the following:
1.
Chronic cough
2.
Fetid breath
3.
Sputum production
4.
Chronic respiratory infections
5.
Hemoptysis
6.
Cough-induced fracture of ribs xviii.
Collagen vascular disease xix.
Cystic fibrosis xx.
Pneumoconiosis xxi.
Lung cancer (primary)
1
HCLA Clinical Practice Protocols Chest CT Scan Rev. Date 2015-10-30 xxii.
Clinical suspicion of superior vena cava syndrome (i.e., venous obstruction by tumor) xxiii.
Other cancer of adjacent structure, or metastatic or extending to lung xxiv.
Estimation of postoperative pulmonary function reserve, prior to anticipated resection, and nuclear medicine perfusion scanning indeterminate xxv.
Preoperative planning for patient with primary hyperparathyroidism, and sestamibi nuclear scan positive for mediastinal location of adenoma
II.
Inappropriate Use
For lung cancer screening, a systematic review and consensus guidelines have concluded that the role and benefits of screening for high-risk patients with low-dose CT scan remains uncertain. The Early Lung Cancer Action Project, a nonrandomized study, screened 31,567 asymptomatic patients age 40 years or older with risk factors, such as cigarette smoking, exposure to secondhand smoke, or occupational exposure (asbestos, beryllium, uranium, or radon), with low-dose CT scan; it detected lung cancer in 1.3% on baseline CT screening, and in 0.3% on annual screening. The study authors estimated the
10-year survival rates for the 412 patients who were diagnosed with stage I lung cancer and concluded that screening led to increased survival for patients diagnosed with early disease. However, other large studies of CT screening of asymptomatic patients with ascertainment of actual deaths due to lung cancer have concluded that, although screening may increase the diagnosis and treatment of lung cancer, it may not reduce mortality from lung cancer. These discordant conclusions are attributed to possible leadtime bias (disease is detected earlier, but death is not delayed), and length bias (CT screening may identify indolent slowly progressive disease that may not otherwise have been diagnosed). The goal of the US National Lung Screening Trial was to determine whether screenings with low-dose helical CT reduced mortality from lung cancer relative to screening with chest x-ray. Trial participants included more than 53,000 current and former smokers with at least 30 pack-years of cigarettes randomized to screening with 3 annual plain chest x-rays or chest CT scans. They were then followed for up to another 5 years. The trial was stopped in October 2010 because the data necessary for inferring effects on the primary end point of lung cancer-specific mortality had been collected. At that point, it was noted that 354 deaths from lung cancer had occurred among participants in the CT arm of the study as compared with 442 lung cancer deaths in the chest x-ray arm. The mortality rate difference of 20.3% is statistically significant. Remaining issues to be resolved include an assessment of risk regarding the cumulative effects of multiple
CT scans as well as cost-effectiveness of screening. Analysis of the data remains incomplete and unpublished. Results of the largest European randomized trial
(NELSON) are still pending. The role of chest CT scan in screening for lung cancer remains uncertain.
For asthma, studies of chest CT have demonstrated some correlation between degree of airway remodeling and lung pathology; however, it is uncertain how such imaging may improve clinical outcomes.
III.
Discussion
2
HCLA Clinical Practice Protocols Chest CT Scan Rev. Date 2015-10-30
Chest CT scan is indicated for further evaluation of abnormal chest x-ray findings, including lung nodules or masses, nonresolving pneumonia, pleural disease, interstitial lung disease, and widened mediastinum or mediastinal masses.
Chest CT scan is used for imaging mediastinal masses, such as thymoma or teratoma, hilar adenopathy suspicious for sarcoidosis, or Hodgkin lymphoma.
CT scan is indicated for further characterization of a solitary pulmonary nodule found on chest x-ray regarding size, shape, and type of opacity; higher rates of malignancy are associated with increasing size, irregularities in shape (speculated or lobular), and ground-glass appearance.
The frequency of CT scan for observation of benign-appearing nodules is guided by nodule size, radiographic appearance, and patient risk factors for malignancy.
Chest CT scan is routinely used for staging and restaging primary lung cancer and for post-treatment surveillance.
Chest CT is commonly used for cancer staging to detect pulmonary metastases secondary to other types of cancer, most commonly head and neck cancer, melanoma, bone and soft tissue sarcoma, and renal cell carcinoma.
Reference:
Milliman Care Guidelines, “Ambulatory Care”, 15 th
Edition.
3