OS 212 Lec 03: Eczema and Dermatitis OS 212 [B]: Locomotion and
advertisement
![OS 212 Lec 03: Eczema and Dermatitis OS 212 [B]: Locomotion and](http://s3.studylib.net/store/data/007196028_1-eef607b1e671e329f23ac03bc4795a0c-768x994.png)
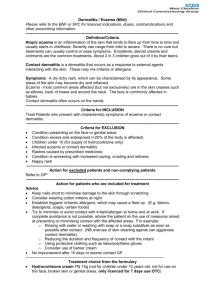
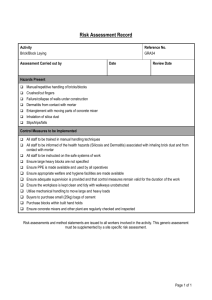
OS 212 [B]: Locomotion and Sensation - Dermatology 1 Lec 03: Eczema and Dermatitis March 17, 2014 Dr. Cynthia P. Ciriaco-Tan OUTLINE I. Introduction II. Histologic Features III. Exogenous Dermatitis A. B. C. D. E. Irritant Contact Dermatitis Allergic Contact Dermatitis Photodermatitis Signs and Symptoms of Contact Dermatitis Diagnosis of Contact Dermatitis Table 1. Classification of Eczema/Dermatitis EXOGENOUS ENDOGENOUS Irritant Contact Dermatitis Allergic Contact Dermatitis Photodermatitis o Phototoxic o Photoallergic UNCLASSIFIED Atopic dermatitis Seborrheic Dermatitis Nummular Dermatitis Dishydrotic Eczema Static Dermatitis Asteatotic Eczema Neurodermatitis/ Lichen Simplex Chronicus Prurigo Nodularis IV. Endogenous Dermatitis A. B. C. D. E. Atopic Dermatitis Seborrheic Dermatitis Nummular Dermatitis Dishydrotic Dermatitis Static Dermatitis V. Unclassified A. Asteatotic Eczema B. Neurodermatitis C. Prurigo Nodulari VI. Differential Diagnosis VII. Management I. INTRODUCTION Ekzein – AD 543, Greek. “to boil out” or to “effervesce” A layman’s term; medical term is DERMATITIS Pruritic papulovesicular process associated with: o Acute: erythema, vesiculation, weeping, edema o Chronic: thickening, lichenification, scaling Both lichenification and thickening may be caused by scratching; however, lichenification involves accentuation of skin lines Can either be exogenous, endogenous, or unclassified Skin inflammation with characteristic clinical and histologic features From Fitzpatrick: Eczema/Dermatitis is a polymorphic inflammatory reaction pattern involving the epidermis and dermis. Acute: pruritus, erythema and vesiculation Chronic: pruritus, xerosis, lichenification, hyperkeratosis + fissuring. II. HISTOLOGIC FEATURES Acanthosis: epidermal thickening and/or widening Spongiosis: edema and serous exudate between epidermal cells Exocytosis: upward movement of lymphocytic/mononuclear infiltrate in superficial dermis and epidermis Subcorneal pustule (neutrophils and bacteria) secondary impetignization; not always present o Presence of PMNs - signals infection (encircled) III. EXOGENOUS DERMATITIS Caused by external factors and/or substances A. IRRITANT CONTACT DERMATITIS Reaction to chemical in a potent concentration in a sufficient length of time Develops at site of contact No allergic mechanism (instant appearance) More common type of contact dermatitis Damage results from direct chemical actionimmediate reaction Provoking substances o Strong/absolute irritants Acids/ alkalis Metallic elements, salts Essential oils Figure 2. Irritant contact o Weak/mild irritants dermatitis Detergent Organic solvent Excessive water exposure B. ALLERGIC CONTACT DERMATITIS First contact with allergen: Sensitization occurs within a few weeks to months after but NO visible skin changes Subsequent contact: presentation of dermatitis May persist for months, years, or forever (due to sensitization) Delayed type hypersensitivity (Type IV) - mediated by Tlymphocytes (memory); may persist forever Education is important so patients can avoid inciting factors Named according to: o Inciting factors/allergens o Location of eczema INCITING FACTORS/ALLERGENS Figure 3. Allergic contact dermatitis due to earrings Plant dermatitis - distinguished by its linear configuration Metal dermatitis - caused by nickel; gold jewelry < 18 carat, gold jewelry > 20 carats recommended Other types - Clothing, footwear, cosmetic, topical medication, occupational dermatitis A Figure 1. Histologic features of eczema REMEMBER: Regardless of etiology, eczema will have similar chronic histologic features: Hyperkeratosis Irregular acanthosis of epidermis Thickening of collagen bundles in papillary dermis (scar) B Figure 4. A Metal dermatitis. B Plant dermatitis is linear and almost vesicular. C Footwear dermatitis. In the US, the Society for Contact Dermatitis identifies the contactant of the year. A Lichen Simplex Chronicus (LSC) – end stage of any eczema CARA, ANJ, NAOMI C A Page 1 / 3 Lec 03: Eczema and Dermatitis LOCATION OF ECZEMA Nipple eczema – usually bilateral, in the young and with family history of the family. It is differentiated from Paget’s disease of the breast (unilateral presentation). Ear eczema Eyelid dermatitis – commonly caused by nail lacquer Diaper dermatitis – spares the skinfolds. Differentiated from candidiasis (reverse). Hand eczema Mucous membrane dermatitis Figure 5. Diaper dermatitis Table 2. Irritant vs. Allergic Contact Dermatitis (Fitzpatrick) ICD ACD Occurs after a single Dependent on sensitization exposure to a an offending Occurs only in sensitized agent that is toxic to skin individuals Dependent on Minute amounts can elicit concentration (threshold) a reaction Occurs in everyone Immunologic reaction that (depends on the involves the surrounding penetrability and thickness skin (spreading of the stratum corneum) phenomenon) and may Confined to the area of generalize exposure (sharply marginated) C. PHOTOCONTACT DERMATITIS Eruption caused by sensitization due to sun-activated irritant/ allergen, as in a medicine, e.g. clindamycin, tetracycline, doxycycline Usually in sun-exposed areas Two types: o Phototoxic- counterpart of irritant contact dermatitis o Photoallergiccounterpart of allergic contact dermatitis Make sure it’s just photoallergy- inner sides of arms are not exposed to the sun, hence not involved D. SIGNS AND SYMPTOMS OF CONTACT DERMATITIS Always has pruritus- if it’s eczematous but not pruritic, think twice! Stages o Acute- erythema, edema, papules, vesicles, bullae (occasionally) o Subacute - dull erythema, minimal edema, vesiculation, crusting o Chronic - LSC; dry, lichenified scaly patches, occasional fissures May also be acneiform, with hyperpigmentation and purpura Can distinguish this from acne by checking if lesions are monomorphic: all lesions are of the same size, same appearance You can have all stages at one point. E. DIAGNOSIS OF CONTACT DERMATITIS Before doing a Patch Test, do History and PE first to close in on the diagnosis, as the test can be expensive. (PGH: P 3000; elsewhere: P 8000) Take the history - course of eruption Physical examination locat Figure 7. Patch Test ion, Cara, Anj, Naomi OS 212 pattern, regional clues, morphology Patch test o “application of specific allergens directly to the skin under controlled conditions, causing a local allergic reaction in a susceptible (sensitized) person (Ale & Maibach, 2010) o Wells/cells of the patch have corresponding chemicals. Allergens are placed in a chart. This will be placed on the skin for 2 days, then check and see where it lights up (reaction occurred). IV. INTERLUDE: Are you having fun? :) ENDOGENOUS DERMATITIS Caused by reactions of the body to self-molecules A. ATOPIC DERMATITIS Known as Besnier’s prurigo, neurodermatitis disseminata More commonly seen in Asians Appear as lichenified plaques Usually found in the antecubital and popliteal areas, neck, and cheek; chronic; hardly found in the acute stage, when found in the acute stage, they usually generalize Patients with atopic dermatitis usually have personal or family history of asthma, urticarial or hay fever Genetic predisposition o Increased IgE-mediated immune responses in early stages; defective T-cells in later stages o Defect in filaggrin gene encoding for filament aggregating protein involved in establishing epidermal barrier function (Sajić, Asiniwasis, & Skotnicki-Grant, 2012) o Atopic skin becomes like a sieve where allergens enter Essential elements (3) o Pruritus o Chronicity/ relapsing course o Characteristic eczema – area lesions appear on depends on stage of atopic dermatitis (discussed later) Stages (3) o Infantile – 2 months to 2 years; attacks on extensor areas, o Childhood – 2-10 years old; attacks on flexural areas Babies below 1 y/o don’t know how to scratch. They just rub against their cheeks when something feels good. As they age, lesions are seen on the areas they can reach (flexural areas) o Adult- localizes in antecubitals, popliteals (flexural areas), but patients can have the reverse, i.e. lesions are still seen in the extensor areas even in adulthood Associated conditions o Keratosis Pilaris A lot of Filipinos present with this lesion Closely associated with skin asthma but can appear in nonasthmatics Autosomal dominant- when your mother or father has it, chances are you have it Around 10 % of atopics are said to have this o Pityriasis Alba reddish rough patch becoming hypopigmented through time Ddx - Pityriasis Vesicolor- determined by KOH, fingernail test - Leprosy- Touch sensation test will not work for kids (they feel or not, it’s the same for them). Let them play outside. If they don’t sweat, positive for leprosy Figure 8. Leprosy B. SEBORRHEIC DERMATITIS Also known as seborrhea Yellowish or grayish, sharply marginated macules covered with greasy scales Macules or papules coalesce to form irregular patches Commonly found in seborrheic areas- areas of greater sebaceous activity such as: scalp, eyebrow, nasolabial area, pre- and postauricular areas, axillae, interscapular area, chest, back, groin Unknown etiology Factors o Stress- lack of sleep, Med school, Derma exam and OSCE o Hypertension, Diabetes, High Cholesterol Page 2 / 3 Lec 03: Eczema and Dermatitis o HIV- earliest dermatologic symptom is seborrhea o Infection- asymptomatic UTI o Change in weather o Alcohol intake Figure 9. Seborrhea on the nasolabial area A. NUMMULAR DERMATITIS Also known as discoid eczema Coin-shaped and eczematous Discrete, erythematous, edematous, papulovesicular plaques Most commonly found in the legs and arms (back of the hands and fingers) Unknown etiology o Simple insect bites, scratches and wounds may develop into nummular dermatitis Figure 10. Nummular dermatitis B. DYSHIDROTIC DERMATITIS Also known as dyshidrosis, cheiropompholyx, pompholyx Recalcitrant, deep-seated vesicular eruptions on the palms and B. OS 212 NEURODERMATITIS Also known as Lichen Simplex Chronicus (LSC) - end stage of any eczema Due to stress or habit of scratching/ rubbing Common in med students, they find a place to pick at constantly o When cause is unidentifiable, the lesions are usually due to stress Single, fixed lichenified plaque Legs, forearms, anogenital areas - areas you can reach In addition to treatment, STOP scratching/touching the lesion Figure 14. Lichen Simplex Chronicus C. PRURIGO NODULARIS Hard nodules on proximal limbs-reachable areas Caused by chronic scratching or rubbing If one finger is used in scratching, the result is prurigo nodularis; if five fingers are used, LSC Example is an insect bite that you keep scratching soles Described as “parang sago-sago sa daliri” Usually clear fluid, but gets easily infected when ruptured purulent (turn into pustules) Location: acral (peripheral); lateral sides of fingers, palms, soles Simultaneous hyperhidrosis Ddx: tinea - important to differentiate due to difference in treatment o Steroids: dyshidrotic dermatitis; Antifungals: tineas Figure 11. Dyshidrotic dermatitis on dorsal side of hands C. STASIS DERMATITIS Varicose eczema - common among adults and elderly Venous insufficiency Pooling of blood Varicosities Varicose edema Static dermatitis Poor nutrition (deoxygenated blood) leads to dryness, itchiness, and edema Chronic condition of lower leg, especially in high heel wearers o Check medial side (note presence/absence of varicosities) Accompanied by hemosiderin deposition (dark spots) and lipodermatosclerosis - thickening of skin Chronic wounds and frequent ulcer formation due to poor blood perfusion Differentiate from edema from Figure 12. Static dermatitis systemic causes by asking “Kailan on lower leg kayo minamanas?” o Upon waking up: systemic o Only in the afternoon: Venous insufficiency V. UNCLASSIFIED DERMATITIS A. ASTEATOTIC ECZEMA Xerotic eczema; winter dry skin, eczema craquele (skin cracks) Common among elderly due to skin dryness Dry skin, with redness, scaling, fine crackling or fine superficial fissures (“crazy paving”) Figure 15. Prurigo Nodularis VI. DIFFERENTIAL DIAGNOSES Fungal infection – has a clear center, advancing border with papules and pruritus is not present all the time Tenia pedis – interdigital webs Psoriasis – with Auspitz’s sign, silvery scales but sometimes shows as red papules so harder to differentiate from eczema Scabies – may present like eczema, but nocturnal pruritus is more intense, interrupting sleepvery small lesions na di mukhang makati Pityriasis rosea Secondary syphilis – if you’re not sure what it is, DON”T TOUCH o Primary is an ulcer in genital area. Secondary is associated with bacteria and can manifest in various forms: copper colored macules and papules; may appear as alopecia, nummular dermatitis Drug reactions Erysipelas Icthyosis Acrodermatitis enteropathica – Zinc deficiency Histiocytosis X – bad case of seborrhea, it can present like a cradle cap, should be spotted early. When you see a baby in the ward with petecchial lesions on the soles and hands with hepatomegaly, think HX Pellagra – Niacin deficiency VII. MANAGEMENT Dressings – so that when you put steroids they won’t ooze out Dessicants – like alcohol Topical steroids – class 1-7, 7 weakest (e.g. Hydrocortisone), know when to use ointments (oil-based, makes acute lesions weep more) versus cream (for acute) Oral Antihistamines – to stop nocturnal itching (atopic dermatitis) Systemic steroids – to downregulate inflammation; use when acute stage is worse Immunomodulators – alternative to systemic steroids (ex. tacrolimus) Ancillary o Antibiotics o Emollients – use for dry skin (atopic dermatitis and eczema craquele) Try to identify contactants, educate patients to avoid them and stop scratching; otherwise, useless treatment END OF TRANSCRIPTION Cara: Hello to everyone, especially packmates Meggie, Anton, Kevin, Owa. Wala na palang IDC so goodbye BSLR-W with seatmates Kei and the broken chair, plus backmates Bernette, Vince, Danette. Goodbye CH222 with Jantan and backmates TheMurillo, Yan 2, JCP. Anj: everything in graciousness and good faith This is the trip. This is the best part of the trip. It’s gonna be wild. It’s gonna be great. You’re gonna be stars. But dig it. We are never, ever gonna be this young again. - Dito Montiel, A Guide to Recognizing Your Saints Naomi: Summeeeeeerrrrrrr! Figure 13. Asteatotic eczema on the leg Cara, Anj, Naomi Page 3 / 3