Nursing Intervention
advertisement

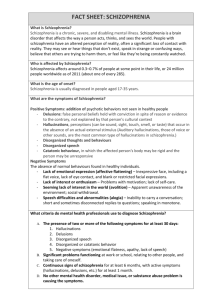
AL-barrak 1430 Nursing Management Assessment Nursing diagnosis Evaluation nursing intervention planing Assessment The nurse must be aware of the client’s status and of changes in the client’s personal life, family situation, and environment to plan care & intervenetio effectively. The symptoms of schizophrenia are divided into positive symptoms ,which represent an excess or distortion of normal functioning & negative symptoms, which represent a deficit in functioning . 1 AL-barrak 1430 Assessing Positive Symptoms of Schizophrenia The positive symptoms appear early in the first phase of the illness. The positive symptoms are presented in terms of alterations of thought, perception, & behavior I- Alteration of thought 1- Delusions: Most common delusional thinking includes : a- Ideas or reference. b- Delusions of persecution. c- Delusions of grandeur. d- somatic delusions. e- Delusions of jealousy. Other delusions observed:Thought broadcasting , the belief that one’s thoughts can be heard by others (e.g. “My brain is connected to the world mind”) Thought insertion, the belief that thoughts of others are being inserted into one’s mind Thought withdrawal , the belief that thoughts have been removed from one’s mind by an outside agency 2 AL-barrak 1430 Delusions of being controlled, beliefs that one’s body or mind is controlled by an outside agency 2- Autistic thinking. 3- Looseness of associations. 4- Clang association. 5- Neologism. 6- Concrete thinking. 7- Echolalia. 8- Word salad. II- Alterations in perception Hallucinations are the major examples of alterations in perception in schizophrenia, especially auditory hallucinations, and loss of ego boundaries (depersonalization & derealization 1- Hallucinations It is estimated that 90% of the people with schizophrenia experience hallucinations at some time during their illness. Although manifestations of hallucinations are varied, auditory hallucinations are most common in schizophrenia. These voices may seem to come from outside or inside the person’s head . The voice may be familiar or strange, single or multiple. 3 AL-barrak 1430 Voices speaking directly to the person or commenting on the person’s behavior are most common in schizophrenia. A person may believe the voices are from. God ,the devil, deceased relatives, or strangers. The auditory hallucinations may occasionally take the form of sounds rather than voices. Commanding hallucinations must be assessed for, because the “voices” may command the person to hurt himself or others. For examples, a client might state “the voices” are telling him to “ jump out of the window” or “take a knife & kill my child”. Commanding hallucinations are often frightening for the individual. A person experiencing them is often in panic levels of anxiety , & commanding hallucinations may signal a psychiatric emergency. 4 AL-barrak 1430 2- Loss of ego boundaries :????????????????????? People with schizophrenia often lack a sense of their body in relationship to the rest of the world, where they leave off and others begin. For this reason, many schizophrenics are confused over their own sexual identity. A client might say he or she is merging with others or is part of inanimate objects. a- Depersonalization ?????????????????????????? Is a nonspecific feeling that a person has lost his or her identity, that he or she is different and unreal . The person may be concerned that body parts do not belong to him or her. Or the person may have an acute sensation that his or her body has drastically changed. For example, people may see their fingers as snakes or their arms as rooting wood. Another may look in a mirror and state his face is that of an animal. b- Derealization ??????????????????????? Is the false perception by a person that the environment has changed. For example, everything seems bigger or smaller , or familiar surroundings have become somehow strange and unfamiliar. Both Depersonalization & Derealization can be interpreted as loss of ego boundaries . 5 AL-barrak 1430 III - Alterations in behavior Bizarre and agitated behavior is associated schizophrenia and may take a variety of forms. with 1. Bizarre behavior May take the forms of a stilted rigid demeanor, eccentric dress or grooming & rituals. The following behaviors are often seen in catatonia Extreme motor agitation Extreme motor agitation is agitated physical behavior Stereotyped behaviors Stereotyped purposeless behaviors are motor patterns that Automatic obedience Waxy flexibility Waxy flexibility consists of excessive maintenance of posture evidenced when a person’s arms or legs can be placed in any position and the position is held for long periods of time. 6 AL-barrak 1430 Stupor The person who is in stupor may sit motionless for long periods of time and may be motionless to the point of apparent coma. Negativism Agitated behavior Assessing Negative Symptoms of Schizophrenia These symptoms are that most interfere with individual’s adjustment and ability to survive. the Initiate and maintain relationships Initiate and maintain conversations Hold a job Make decisions Maintain adequate hygiene and grooming It is the presence of negative symptoms that contributes to the personal poor social functioning and social withdrawal . Affect of a schizophrenic person usually falls into one of three categories: Flat or blunted Inappropriate Bizarre Flat or blunted affect is commonly seen in schizophrenia 7 AL-barrak 1430 Inappropriate affect refers to an emotional response to a situation that is not congruent with the tone of the situation For example, a young man, told that his father is ill , breaks out laughing . Bizarre affect is especially prominent in the disorganized form of schizophrenia. Other negative symptoms include Anergia Anhedonia Avolition Poverty of speech. Thought blocking Nursing diagnoses are formulated from the information obtained during the assessment phase of the nursing process. The following is a listing of some of the more common diagnoses applicable to schizophrenia. 1- Altered thought processes. 2- Sensory perceptual alterations. 3- Impaired verbal communication. 4- Social isolation. 5- Ineffective individual coping . 6- Self-care deficit (bathing , hygiene , dressing , grooming , feeding , toileting ). 7- Altered family processes. 8- Risk for violence (directed at others) 9- Risk for violence (self-directed) 8 AL-barrak 1430 1- Altered thought processes Related to Impaired ability to process and synthesize internal and external stimuli Biologic factors (neurophysiologic, genetic) sensory-perceptual alterations. Psychosocial/environmental stressors Evidenced by Inability to distinguish internally stimulated irrational ideas leading to faulty conclusions(autistic) Perceives that others in the environment can hear his or her thoughts(thought broadcasting). Demonstrated neologisms, word salad, thought blocking, thought insertion, thought withdrawal, poverty of speech , or Mutism Believes that her thoughts are responsible for world events Goals Demonstrate reality-based thinking in verbal and nonverbal behavior. Demonstrate absence of psychosis (delusions, incoherent, illogical speech , magical thinking ideas of references, thought blocking thought insertions ,thought broadcasting). 9 AL-barrak 1430 Nursing Intervention 1. Approach the client in a slow , calm matter-of-fact manner, to avoid distorting the client’s sensory-perceptual field, which could foster altered thoughts and perceptions. 2. Maintain facial expressions and behaviors that are consistent with verbal statements. Patients care very sensitive to other’s responses to their symptoms. 3. Continue to assess the client’s ability to think logically and to utilize realistic judgment and problem-solving abilities. 4. Listen attentively for key themes and reality-oriented phrases or thoughts. Interpret , the client’s misconceptions and misperceived environmental events in a calm , matterof-fact manner ..Identification of reality by a trusted person is helpful. 5. Instruct the client to approach staff when frightening thoughts occur. A respectful, interested approach will enable the patient to discuss unusual and frightening thoughts. 6. Refrain from touching a client who is experiencing a delusion especially if it is a persecutory type. Touch may be interpreted as a physical or sexual assault. 7. Avoid challenging the client’s delusional system or arguing with the clients, since delusion cannot be changed through logic, and challenging the belief, may force the client to adhere to it and defend it. 10 AL-barrak 1430 8. Distract the client from the delusion by engaging him in a less threatening or more comforting topic or activity at the first sign of anxiety or discomfort. 9. Focus on the meaning, feeling , or intent provoked by the delusion rather than on the delusional content. 10.Avoid seeking the details of the client’s delusion so as not to reinforce the false belief and further distance client from reality. 11.Offer praise as soon as the client begins to differentiate reality based and non-reality based thinking. 12.Respond to the client’s delusions of persecution with calm , realistic statements. 13.Use simple declarative statements when talking to the client who demonstrates, disconnected , incoherent , or tangential speech patterns , which reflect loose associations . 2. Sensory / perceptual alteration : Related factors Psychosocial stressors, loneliness and isolation ( perceived or actual ). Withdrawal from environment. Lack of adequate support persons. Chronic illness and institutionalization. Altered thought processes. Disorientation. 11 AL-barrak 1430 Derealization , depersonalization. Ambivalence . Biologic factors (neurophysiologic, genetic). Evidenced by Negligent to surroundings (preoccupied with hallucination) Startles when approached and spoken to others. Talks to self (lips move as if conversing with unseen presence Appears to be listening to voices or sounds when neither are present (cocks head to side as if concentrating on sounds that are inaudible to others ). May act upon “voiced” commands ( may attempt mutilating gesture to self or others that could be injurious). Describes hallucinatory experience “ It’s my father’s voice and he’s telling me I’m not good” Goals Able to hold conversation without hallucinating. Remains in group activities. Attends to the task at hand (e.g. group process , recreational or occupational therapy activity ). States that hallucinations are under control. 12 AL-barrak 1430 Nursing Interventions 1. Continuously orient patient to actual environmental events or activities , to present reality. 2. Call the client and staff members by their names to reinforce reality. 3. Utilize clear statements. 4. Utilize clear, direct verbal communication rather than unclear or nonverbal gestures. 5. Focus on real events or activities to reinforce reality and divert client from the hallucinating experience. 6. Reassure the client (frequently if necessary ) that she is safe & won’t be harmed 7. Observe for verbal or nonverbal behaviors associated with hallucinations. 8. Attempt to determine precipitants of the sensory alteration (stressors that may trigger the hallucination ) 9. explore the content of the auditory hallucinations to determine the possibility of harm to self, others or the environment ( auditory command and hallucinations ) to prevent destructive behavior. 13 AL-barrak 1430 10.When danger or violence is imminent , protect the client and others by the following facility procedures and policies for seclusion , mechanical restraint to prevent harm or injury to client or others. 11.Teach the client techniques that will help stop the hallucinations . 3- Impaired verbal communication Related factors Disturbances in the form of thinking ( autistic ). Altered thought processes (e.g. delusions , magical thinking Poverty of speech / Mutism. Sensory / perceptual alternations ( e.g. hallucinations ) Disturbances in structure of associations ( e.g. neologisms , word salad , preservation) Evidenced by Loose associations Neologisms Word salad Clang associations Echolalia Goals Communicates thoughts and feelings in a coherent , goal directed manner. Demonstrates reality-based thought processes in verbal communication. 14 AL-barrak 1430 Nursing Interventions 1. Assess the degree to which the client’s impaired verbal communication interferes with her ability to get others understand the meaning behind the message and to clarify communication. 2. Demonstrate a calm , patient behavior , rather than attempting to force the client to speak coherently , to decrease the client’s fears & anxieties about the inability to communicate needs to demonstrate acceptance of client. 3. Actively listen to , observe verbal & nonverbal cues & behaviors during the communication process, to piece together each method of communication , to understand better the aim of the client’s message , and demonstrate a willingness to meet the client’s needs. 4. Use communication strategies such as restatement , classification, and consensual validation , to help reveal the intent of the client’s messages . 5. Acknowledge the client’s inability to use the spoken word while encouraging alternative methods to convey messages ( gestures, writing, drawing ) to communication process. 6. Instruct the client to seek assistance from staff when experiencing communication problems ,Staff can help facilitate the communication process. 7. Praise the client’s attempt to speak more coherently and to engage in more meaningful conversations with others , to 15 AL-barrak 1430 increase self-esteem and promote continued functional speech patterns. 4- Social isolation Related factors Altered sensory perception ( hallucinations or illusions ) Altered thought processes ( delusions , magical thinking , ideas of reference , thought blocking , thought insertion ). Impaired verbal communication ( neologisms , word salad , loose associations , tangentially , incoherence , poverty of speech , Mutism ). Long-term illness, hospitalization , or environmental withdrawal. Evidenced by Withdrawal from the environment and from others in the environment ( Isolates himself in his room or bed for most of the day and night ). Difficulty in establishing relationship with others in the environment ( fails to seek out or respond to others ). Verbalizations that indicate feelings of rejection from others in the environment. Inability to engage in social interactions or milieu activities. Inability to share or express feelings with others in groups or one-to-one . Goals Verbalize willingness to engage in social interactions and activities with others in the environment. 16 AL-barrak 1430 Nursing Interventions 1. Assess the extent of the client’s self-imposed isolation , to plan strategies to break the pattern of withdrawal with interactions and activities. 2. Assist the client to meet basic needs during times of social withdrawal (sleep, nutrition , personal hygiene ) to promote the client’s physical health and well-being. 3. Structure each day to include planned times for brief interactions and activities with the client to help the client organize times to engage with others and to let the client know that participation is expected and that he or she is a worthwhile member of the community . 4. Spend brief intervals with the client each day , engaging in meaningful , non challenging interactions , to ease the client out into the community by first developing trust , rapport , and respect. 5. Discuss with the client anything of interest to her , such as items in the client’s room , favorite activities, or hobbies , to encourage the client’s social skills and decrease social isolation. 6. Provide the client with stimulation from recreational and other milieu activities to expose the client to social activities and increase opportunities for socialization. 7. Encourage the client to engage in social activities that are within her physical capabilities and tolerance, to provide the client with successful social experiences that are likely to be repeated. 17 AL-barrak 1430 18