Simulated Patient Instructions
advertisement

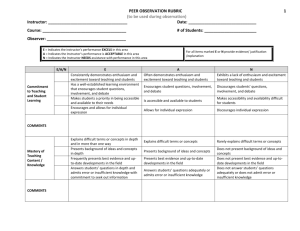
Patient Instructions Name of Patient: Mary Berry Description of the patient & instructions to simulator: A 65 yr old lady with a 10 day history of headache. Recently (1 month ago) had Amlodipine dose increased. Wonders if it is the tablet and whether she needs to switch treatment. Has read the Pilealfet and headache is one of the side effects. Also feeling a bit achy and has read the Pilealfet which says statins cause muscle pain Starts the consultation 'I wonder if I need to change my tablets doctor, as they are upsetting me' Nature of headache Particularly bad over right temple. Jaw aches with eating (only if asked) Feels generally unwell with it; tired, a little sickly and off food. No visual symptoms (only if asked) No vomiting. No positional symptoms. No neuro symptoms. (only if asked) Paracetamol has not really helped. Not tried much else. Idea: It's the tablets Concern: Worried it's the tables and her symptoms are have started to affect her baking performce - Womens Institute annual baking competition is on thehorizon. Expectation: Wants to get better. Would like something to help with pain. PMH/DH: HT Hypertension - Takes Amlodipine 10mg a day On Atorvastatin 20mg for primary prevention. 1 Doctor’s (GP ST) Instructions Name & age of patient Mary Berry age 65 Summary Card PMH: HT DH: Atorvastain 20mg, Amlodipine 10mg Allergies: None Case Notes - Last few entries in records: From 1 month ago BP not at QOF target - increase Amlodipine to 10mg 2 CSA EXAMINATION CARD Patient Name: Mary Berry Examination findings: Tender over temples/ temporal artery BP 150/80 Fundoscopy normal. Visual fields normal. CSA Case Marking Sheet Case Name: TA Case Title: Context of case New onset temporal arteritis Assessment Domain: 1. Data-gathering, technical and assessment skills Positive descriptors: Asks about jaw claudication and scalp tenderness Asks about visual symptoms Asks about PMR symptoms Rule out red flags: Symptoms of raised ICP Appropriate exam-Including BP and visual. Elicits ICE Negative descriptors: Does not check for visual problems. Does not rule out red flags Fails to examine or examination incomplete Fails to elicit ICE. Assessment Domain: 2. Clinical Management Skills Positive descriptors: Explains likely diagnosis in simple way. Explains risk of not treating (esp. re vision) Explains initial treatment and investigations(steroids and ESR/ CRP) Explains need for referal for urgent biopsy for definitive diagnosis Explains need for aspirin and possible bone protection as well Safety nets re. vision Makes a sensible plan for tests, referral Negative descriptors: Does not make a diagnosis of TA Explanation unclear. Fails to order investigations to confirm suspicion. Fails to start appropriate treatment. Safety netting not done, not appropriate or not explained. 3 and follow-up Assessment Domain: 3. Interpersonal skills Good rapport Elicits ICE. Establishes how headache affecting lifethrough psych social exploration Explains diagnosis, management and reason for safety netting in appropriate language. Checks for understanding. Doesn’t elicit ICE. Fails to explain things clearly to patient. Offers options inappropriately or without heavy spinning. 4


![njc6_publication_2[^]](http://s3.studylib.net/store/data/007850226_2-d94f2aa4ee57f77430443fae8e981d05-300x300.png)