MS-1 FUND 1: 8:00-9:00 Transcriber: Ramon Reddick Monday
advertisement
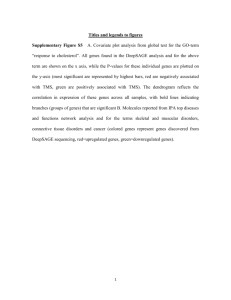
MS-1 FUND 1: 8:00-9:00 Monday, September 15, 2014 Dr. Nathaniel Robin Genetic Inheritance III Transcriber: Ramon Reddick Editor: Jessie Allaway Page 1 of 5 Abbreviations: MD=Myotonic Dystrophy; AD=Autosomal Dominant; UTR= Untranslated Region; HD= Huntington Disease; MtDNA= Mitochondrial DNA; PWS= Prader Willi Syndrome; AS= Angelman Syndrome; UPD= Uniparental Disomy Introductory Comments: Dr. Robin commented that some of the material in the lecture has been difficult for students in previous years. Some of the material will be extra information given will not be testable material. The time stamps are based on the ECHO recording. <ARS Question 00:48> Traditional (Mendelian) vs. Non-Traditional Inheritance (slide 3) 01:40 a. Traditional (Mendelian) i. Equal maternal and paternal contributions to the genome of the progeny a. Identical contributions from parents are identical ii. Mutations are static (do not change) across generations a. Mutations are exceptionally rare events b. What you pass on is basically are the genes you had yourself iii. Maternal and Paternal alleles of a gene are functionally equivalent iv. 2 copies of an autosomal gene are sufficient for health b. Non-Traditional Inheritance (do not work under the same principles) i. Mitochondrial genetics- mitochondrial inheritance are NOT from both patents ii. Triplet Repeat- have dynamic alterations and are NOT static; change through sex-specific meiosis iii. Imprinting 1. Functional ability, the paternal and maternal genes are turned off in certain states 2. Functionally, paternal and maternal genes are not equivalent functionally a. Having both copies of the gene may not result in normal functionality with imprinting II. Triplet Repeat Disorders (slide 4) 4:14 a. General Information i. Relatively recently identified set of conditions which certain common characteristics ii. Dynamic, not static genetic alteration I. II. 1. Expansion of a stretch of repeated 3- nucleotide sequence – CAG, CGG, GAA 2. Region of DNA could be a intron, promoter, slice site, etc 3. When they occur within genes the can result in a healthy, intermediate, or disease state b. Examples: [sn: you do not have to know the details of the conditions, however, you DO need to know how these diseases show principles of triplet repeat disorders] i. Fragile X Syndrome ii. Huntington Disease iii. Myotonic dystrophy c. Rules of Triplet Repeat Diseases i. Severity of the phenotype correlates with the degree of expansion of the triple repeat sequence 1. As the number of repeats in the gene increases, the earlier the disease will onset or the more severe it will be ii. Genetic anticipation- Expansion increases in subsequent generations; gets worse over time iii. Usually more specific to either maternal or paternal meiosis 1. For a given disorder, expansion will only occur in maternal or paternal meiosis, not both 2. (sn: specifics to each of the diseases are explained below) Fragile X Syndrome: Clinical (slide 6-9) 7:21 a. Common cause of intellectual disability (1or 2/1000) i. Originally known as Martin-Bell Syndrome b. AD with genetic anticipation i. Expansion occurs through maternal meiosis 1. Fathers can pass this on, but the symptoms are about the same as the father’s 2. When mothers pass the trait, the symptoms are worse ii. Phenotypes 1. Intellectual disability, autism 2. Characteristic facial findings a. Long face, prominent ears, larger head, deep set eyes, autistic mannerisms, initially taller, get shorter over time 3. Larger testicles 4. Shorter stature 5. Premature ovarian failure (premutation women): go through menopause earlier (40 or younger) 6. Fragile X Tremor/ataxia Syndrome (transmitting males) a. Shake when doing things MS-1 FUND 1: 8:00-9:00 Monday, September 15, 2014 Dr. Nathaniel Robin Genetic Inheritance III Transcriber: Ramon Reddick Editor: Jessie Allaway Page 2 of 5 Abbreviations: MD=Myotonic Dystrophy; AD=Autosomal Dominant; UTR= Untranslated Region; HD= Huntington Disease; MtDNA= Mitochondrial DNA; PWS= Prader Willi Syndrome; AS= Angelman Syndrome; UPD= Uniparental Disomy c. 7. Unusual inheritance pattern (Sherman Paradox) <ARS Question 10:05> Fragile X Inheritance: The Sherman paradox (slide 7) 10:53 i. Pedigree of a family carrying Fragile X syndrome. Findings show that: 1. Excess of affected females a. Percentage of affected women and severity increase 2. Obligate transmitting (unaffected carrier) males; may develop tremors 3. Increasing severity in progressive generations (‘anticipation’) i. Especially when conditions is transmitted by a female d. Fragile X Genetics (slide 8) 12:17 i. FMR1 genes (bottom part of X-chromosome) contains unstable, expandable CGG trinucleotide repeat in the 5’ UTR (untranslatied region) of exon 1 1. Normal state: 5-50 repeats a. Most people exist in this range. To go beyond 50 is extremely rare 2. Premutation: 55-200 repeats = risk to have child with Fragile X syndrome a. Female at very high risk for full expansion in meiosis child would have over 200 repeats b. Studies of healthy carrier women with even 50-60 repeats found to have higher rate of mild psychiatric disorders, depression, learning disabilities i. No true asymptomatic premutation state 3. Full mutation (Fragile X syndrome): > 200 repeats a. Causes excessive methylation, shuts off protein production <ARS Question 14:39> b. The more expansion you have, the worse the condition is e. Pathogenesis FXS and Treatment (slide 9) 15:48 [sn: this is just extra information. Dr. Robin said we will NOT have to know this] i. FXS is caused by transcriptional silencing of the FMR1 genes, but pathogenesis is unknown ii. mGluR5 theory- FXS symptoms are due to unchecked activation of metatrobic glutamate receptor (mGluR5) 1. Experimental drug blocks receptor; can design drugs to reverse or inhibit the process iii. 50% reduction of the mGluR5 ax in Fragile X mouse model reduce FRS symptoms iv. Drugs to reduce mGluR5 activity coming? <ARS Question 17:57> III. Huntington Disease (slide 10, 18:46) a. Famous because often used as an example in bioethical discussions about genetic testing b. Incidence 3-7/100,000 i. Scan of brain shows a large portion of brain missing; basal ganglia eroded away, causing choreaform movements c. Phenotype: i. Progressive dementia; chorea (involuntary movements; later in life); psychiatric disturbance ii. Early onset presents with psychiatric symptoms iii.Later onset is correlated with involuntary movements d. Genetics: AD, fully penetrant, 90% familial (if mutation present, you will get disease) i. Bigger the mutation, earlier the onset of symptoms, more psychiatric disorders; severity is pretty uniform ii. HD gene is huntington, on 4p12 iii. Normal: 10-29 repeats; HD: 37+ iv. [sn: student asks question about why 200 is the magic number of repeats that causes Fragile X. Dr. Robin explains and draws on board that there’s no known reason, represents somatic mosaicism; not important for test info] V. Myotonic Dystrophy [sn: there are no slides to this disease] 25:22 a. Patients develop Myotonia - inability to release a muscular contraction b. Other symptoms include cardiac symptoms and endocrine abnormalities c. Progressive: over generations, the disease worsens d. Became classic example of genetic anticipation; expansion only occurs through maternal meiosis VI. Summary of Triplet Repeat Disorders [sn: no slide] 27:03 a. Increased expansion leads to with increased severity of phenotype and decreases age of onset of symptoms b. Expansion is sex specific i. Fragile X and Myotonic dystrophy expand through maternal meiosis only ii. HD is expanded through paternal meiosis only c. All are neurologic-based diseases and there is no general mechanisms for these diseases i. HD is neomorphic (cause new function) ii. Fragile X is hypomorphic (shuts off gene’s function) Mitochondrial Inheritance (slide 11-15) MS-1 FUND 1: 8:00-9:00 Monday, September 15, 2014 Dr. Nathaniel Robin Genetic Inheritance III Transcriber: Ramon Reddick Editor: Jessie Allaway Page 3 of 5 Abbreviations: MD=Myotonic Dystrophy; AD=Autosomal Dominant; UTR= Untranslated Region; HD= Huntington Disease; MtDNA= Mitochondrial DNA; PWS= Prader Willi Syndrome; AS= Angelman Syndrome; UPD= Uniparental Disomy VI. Mitochondrion (slide 11) 28:03 a. Separate genome from the nucleus i. Make proteins for solely the mitochondria processes b. Makes energy ATP for the cell via oxidative phosphorylation c. Electron Transport Chain (ETC) in inner membrane i. 5 enzymatic complexes derived from both mitochondrial (13) and nuclear (>60 subunits) genomes VII. Disorders of energy metabolism (slide 12) 29:53 a. Mitochondrial disease are disease of energy supply b. Phenotype related to organ’s energy requirement and % abnormal mitochondria (heteroplasmy = mosciacism) i. Correlate with high energy requiring organs 1. Heart, skeletal muscle, brain, eye, ear 2. Leads to vision problems, deafness, seizures, other intellectual disabilities, myopathy, cardiac myopathy ii. Common Symptoms and signs: seizures, ataxia, MR, weakenss/hypotonia iii. More abnormal mitochondria the worse the phenotype iv. Phenotype usually worse over time (2˚ high mutation rate) 1. No repair mechanism; mitochondria do not work as well over time; another theory of aging VIII. Mitochondrial Inheritance (slide 13) 31:02 a. Maternally inherited ONLY i. Sperm and egg both have mitochondria, but all mtDNA in the zygote come from the egg 1. Mitochondria are housed in the sperm tail which falls off during fertilization ii. Pedigree shows maternal inheritance 1. Affected mom has only affected children, no healthy children 2. Affected dad has only healthy children <ARS Questions 31:50 & 33:02> IX. Mitochondrial Genome (slide 14) 34:05 Circular, 1600bp, with non-identical ‘heavy’ and ‘light’ chain, transcribed sequentially (vs. nuclear genome), no introns; strands that code for 2 rRNA, 22 tRNAs, 13 polypeptides i. Most mitochondrial/ETC proteins from nuclear DNA ii. All 13 polypeptides go to make ETC proteins b. Differences from nuclear DNA i. Transcription by mtDNA specific to RNA polymerase 1. Prevent nuclear transcriptional machinery from reading it ii. MtDNA does not complex with histone proteins iii. MtDNA does not have DNA repair machinery 1. Mutation rate 5-10x greater than nuclear DNA Imprinting (slide 15, 34:54) <ARS Question 35:07> XI. Imprinting is epigenetic (slide 17) 36:42 a. Genetic Imprinting is a type of epigenetic modification that is sex-specific i. Epigenetics- study of mechanisms that affect gene expression (typically defined as a hereditary alteration in gene a. expression through noncoding sequence events; this slightly different because it’s not strictly hereditary) 1. Do not involve changes in DNA sequence 2. Can be inherited through cell division a. Ex. For a male: receives a copy of mom’s & dad’s chromosome 15 (for example), will pass on only dad’s copy; will take mom’s copy & dad’s, erase it & reset it as a Dad’s copy (if male) or female copy (if you’re female) ii. Imprinting is not technically hereditary because the imprints are reset XII. Images (slide 18) 37:54 a. Hydatidiform mole – 46,XX (or 46, XY) (all paternal) b. Ovarian teratoma- 46, XX (all maternal); uniparental disomy for the whole thing c. Both are genetically normal product of conception, all with normal 46 chromosomes & DNA sequence but epigenetic problems <ARS Question 38:47> XIII. Imprinting (slide 19) 39:21 a. We have 2 copies of most genes (half from mom, half from dad); certain genes don’t function equally i. Basic assumptions for normal genes (NOT imprinted genes): MS-1 FUND 1: 8:00-9:00 Monday, September 15, 2014 Dr. Nathaniel Robin Genetic Inheritance III Transcriber: Ramon Reddick Editor: Jessie Allaway Page 4 of 5 Abbreviations: MD=Myotonic Dystrophy; AD=Autosomal Dominant; UTR= Untranslated Region; HD= Huntington Disease; MtDNA= Mitochondrial DNA; PWS= Prader Willi Syndrome; AS= Angelman Syndrome; UPD= Uniparental Disomy 1. Maternal and paternal genes are equal 2. Two copies of autosomal genes are sufficient for health a. Normal development requires contribution of both maternal and paternal genomic components b. Differential expression of alleles depending upon the parent of origin (slide 20) 39:31 c. Limited number of autosomal genes that can undergo imprinting, not evenly distributed throughout genome d. Exist in segments on certain chromosomes: 6, 7, 11, 14, 15, & 20 i. We know this because some people can have maternal/paternal UPD on other chromosomes and are perfectly healthy ii. Some imprinted genes show mono-allelic expression in some cell types, but bi-allelic expression in others 1. Using the same genes to do many functions XIV. Imprinting is epigenetic modification (non-hereditary) (slide 21) 40:37 a. Imprints may be “relaxed” during development b. Imprints “reset“ during gametogenesis i. Example: woman has a “dad” and a “mom” chromosome, for ex. Chromosome 15 ii. In her ovary, imprinting is erased iii. When she goes to make oocytes, the chromosomes are repainted to both be “pink” (her chromosome 15’s are only maternally imprinted) regardless of if it was from mom or dad (DNA sequence didn't change) 1. [sn: student question on imprinting] 2. Conventionally silences gene function but can enhance gene function 3. Imprinting is due to hypermethylation (non-coding modification) Imprinted genes must be ‘reset’ during gametogenesis (slide 22) 45:31 i. Failure to reset, due to mutation in imprinting region, causes her to pass on her paternally imprinted alleles (a deleterious mutation) i. Failure to switch a maternal imprint to a paternal imprint, or visa versa, can lead to disease ii. Failure provide an imprinted gene can also lead to disease 1. Not being able to reset imprints after erasing 2. Or not being able to erase the imprinting XV. Imprinting causes differential expression from maternal to paternal alleles (slide 23) 46:14 a. Transcription can be either enhanced or repressed i. Imprinted regions are conventionally shut off (inactivation of a region) c. 1. “inactivation” is technically NOT the definition of imprinting b. DNA methylation is involved in imprinting process XVI. Human Imprinted chromosomes (slide 24) 46:28 a. Many human chromosomes have imprinted regions (while some don’t) i. Regions of inactivation and activation are clustered together 1. Occur in clusters with imprinting centers ii. First suggested for chromosome 7 iii. Other chromosomes 6, 11, 14, 15, and 20 iv. Total, about 150 known genes from about 110 cytogenetic bands b. Other chromosomes do not have significant imprinted regions or genes i. Chromosomes 12 and 21 XVII. Imprinting (slide 25) 47:05 a. Mechanism: Methylation of CpG dinucleotides in genes or key regulatory elements i. Methylation silences genes expression b. Imprinted genes important in development, growth, embryonic viability i. Aberrations cause neurodevelopmental/cognitive impairment, birth defects, malignancy ii. Some genes are imprinted at certain parts of development iii. Other genes are imprinted only post-gestationally through life, and not in development iv. Some genes are imprinted only in certain tissues c. In total, about 1% of human genome i. Fewer than mouse genome, and different gees (implications for research) XVIII. Human Imprinting disorders (slide 26) 48:24 [sn: **know AS, PWS, and Beckwith Weidemann Syndrome (on Boards)] a. Angelman Syndrome (15q13) (slide 27, 48:28) i. Severe developmental delay/MR ii. Severe seizures iii.Absence/very limited speech; can’t put two words together in a sentence MS-1 FUND 1: 8:00-9:00 Monday, September 15, 2014 Dr. Nathaniel Robin Genetic Inheritance III Transcriber: Ramon Reddick Editor: Jessie Allaway Page 5 of 5 Abbreviations: MD=Myotonic Dystrophy; AD=Autosomal Dominant; UTR= Untranslated Region; HD= Huntington Disease; MtDNA= Mitochondrial DNA; PWS= Prader Willi Syndrome; AS= Angelman Syndrome; UPD= Uniparental Disomy iv. Gait ataxia (jerky movements and most can't walk) v. Inappropriate bouts of laughter vi. Subtle facial characteristics b. Prader Willi Syndrome (15q13) i. Neonatal hypotonia; low tone; “floppy kids”; can’t eat, failure to thrive, some males have hypogenitalism ii. Hyperphagia Severe Obesity 1. At 2-5yrs old, develop voracious appetite & eat everything, dogfood even; ex. 4yr old weighing 150lbs iii. Mild- moderate intellectual disability is common iv. Bad behaviors/tempers v. Hypogonadism vi. AS and PWS are not clinically similar, but caused by identical chromosome 15 deletion c. Beckwith Wiedemann Syndrome (11p15) d. Russell Silver Syndrome (7q, 11p) e. Albright hereditary osteodystrophy (20q) f. Maternal and paternal UPD14 g. Transient neonatal diabetes UPD6 [sn: lecture ends at slide 27] Student Questions Question 1: If the hypermethylation occurs at 200 (Fragile X), why does the disease get worse at higher repeats? Answer: The higher the number of cells with his somatic mosiacisms is not producing and of the fragile X gene and this is why the condition worsens and get earlier onset Question 2: Is imprinting associated with crossing over? Answer: No, crossing over has nothing to do with imprinting. <END OF LECTURE 51:39>