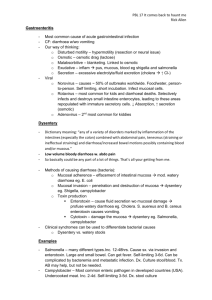
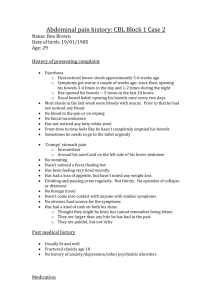
Diarrhoeal illness including dysentery handout
advertisement

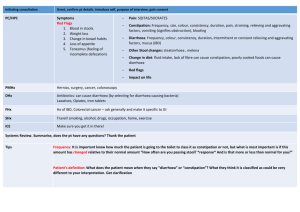
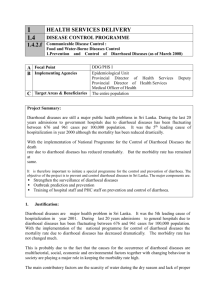
Diarrhoeal illness including dysentery There are key questions in assessing someone with diarrhoea o o o o o o o How long has this been going on? How frequently are they going? How much fluid are they taking in? What colour is the stool/any blood? Any fever? Are they HIV positive? Are they also vomiting? (how much? What colour?) Then examine the patient Assess fluid status, is the patient dehydrated… o BP (low in dehydration) o Pulse (raised in dehydration) o JVP (not seen in dehydration) o Skin turgor (decreased in dehydration) o Restlessness/lethargy o Look at fluid input/output o Sunken eyes Examine the patient fully especially looking at the abdomen for signs of perforation (rigid, distended, tinkling bowel sounds), which is common in typhoid. Ensure all vital signs are recorded. Bowel sounds are usually increased in diarrhoeal illness. Stool sample should be sent for ova, cysts and parasites. FBC and U+E should be taken to assess level of infection and dehydration/ electrolyte imbalance. Ensure MPS rule out malaria. HIV status should be known on all diarrhoeal patients. Specific diarrhoeas Typhoid A high fever with bradycardia is indicative of Typhoid, these usually occur within the 2nd week of illness. The first week tends to have a vague illness with malaise, fever and constipation. In the third week of illness the patient can become delirious with pea soup diarrhea. Leucopaenia and thrombocytopaenia are often found in the FBC. This should be treated as below (ciprofloxacin 500mg bd for 14 days or co-trimoxazole 960mg bd for 14 days) Cholera Provided by T. Whitfield 2012 White stool/ rice coloured watery diarrhea indicates cholera, the patient will need isolating as it is highly infectious. The patient will need high volumes of fluid replacement via oral rehydration salts (ORS) or IV fluids as the priority management. Doxtycline or azithromycin (if pregnant) can also be used. Managing acute diarrhoea (usually less than a week) The key is to administer adequate fluid re-placement and administer antibiotics if appropriate. Fluids In dealing with a diarrhoeal patient we must decide if they have adequate fluid replacement and how serious the diarrhoeal illness is. More than 6 non bloody stools a day is severe and warrants iv fluids. Less than 5 stools a day warrants oral fluids only, unless the patient is clearly dehydrated (low BP, tachycardia, poor urine output, poor skin turgor, lethargic/agitated), or they are vomiting and unable to take oral fluids. If the patient is clearly dehydrated give a bolus fluid to try to improve the blood pressure and urine output. A suitable bolus of fluid would be 250-500ml normal saline 0.9%. Further boluses can be given if this is ineffective, the patient who is dehydrated should have at least 3 Liters of fluid a day. (refer to fluid management guidelines) The use of antibiotics in acute diarrhoea Antibiotics can be with held if the patient is well hydrated, without fever and normal observations. In severe diarrhoea (6 or more stools a day then antibiotics are appropriate, ciprofloxacin 500mg BD or cefuroxime if too ill to take) If cholera is suspected and the patient has severe diarrhea then give either doxycycline 300mg PO (not if pregnant), or azithromycin 1g PO. Blood in the stool Blood in the stool could as a result of bacillary dysentery such as campylobacter shigella, salmonella, typhoid and E coli. These are sudden illnesses often with fever and systemic uset (other vital signs are effected). These bacteria do not necessarily produce large amounts of diarrhea but are important to treat. These can be treated with ciprofloxacin 500mg po bd, or iv ceftriaxone 2g bd if the patient is very ill. Amoebic dysentery does not tend to produce fever but causes prolonged bloody diarrhoea. This can be treated with metronidazole 400-800mg tds Provided by T. Whitfield 2012 Severely wasted HIV patients are more vulnerable to severe diarrhoeas and antibiotic therapy (IV ceftriaxone and IV metronidazole) is often started as a precautionary measure as these patients are so frail. Persisant diarrhea (3 or more liquid stools a day for over a month.) There are many causes of prolonged diarrhea, the first step should be to rule out infective causes. Chronic diarrhea due to many different organisms is common in those immunocompromised by HIV, the step is to test for HIV. A stool sample should be sent for ova, cysts and parasites Ask what drugs (prescribed and non-prescribed) the patient takes and see if those cause diarrhoea. Consider stopping them if they do. In HIV patients the portozoans Cryptosporidium parvum and Cyclospora cayetanensis (also occurs in non HIV patients) can cause persistant watery diarrhea. These can be identified by oocysts in the stool. Cryptosporidiosis necessitates the start of HAART treatment and rehydration there is no specific treatment. Cyclospora can be treated with cotrimoxazole 960mg bd for 7-10 days. The HIV guidelines give a clear guideline on HIV patients with diarrhea. Strongyloides can also cause persistent diarrhoea in HIV patients, the larvae can be detected in the stool, under microscopy, this is treated with albendazole 400mg bd for 14 days or ivermectin 200mcg/kg po for 2 days.) Metronidazole 800mg tds for 7 days can be used to treat amoebic dysentery which can cause prolonged diarrhea usually with blood. It can also invade outside the intestine to enlarge the liver, cause abscesses and perforate the bowel. Three stool samples should be taken to look for cysts. In Malawi laboratory facilities and testing kits can be difficult to get hold of, it therefore may be appropriate to treat patients with the above therapies blindly to see if there is any improvement. If there is no obvious cause to the diarrhea is found, and no improvement is seen from the antimicrobial therapies then colonoscopy and biopsy could be indicated to look for diseases such as inflammatory bowel disease, whipples and intestinal TB. Provided by T. Whitfield 2012