Programme Specification - University of Bradford
advertisement

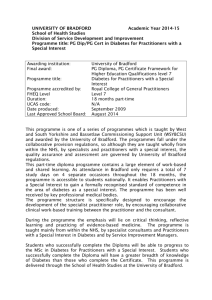
Programme Specification Awarding institution: Teaching institution: Final award: Programme title: Duration: Programme accredited by: Clinical opinion sought from: Date revised: University of Bradford Bradford and Airedale teaching Primary Care Trust Post Graduate Diploma Post Graduate Certificate Post Graduate Diploma in Diabetes for Practitioners with a Special Interest Post Graduate Certificate in Glycaemic Control for Practitioners with a Special Interest (exit award only) Normally 18 months part-time, but up to five years Royal College of General Practitioners; Royal College of Physicians June 2007 This part-time diploma course comprises a large element of work-based and shared learning. Students therefore need not be Bradford-based to undertake the course. This course enables General Practitioners (GPs) and other registered health professionals, in particular, primary care practitioners, to gain a formally recognised standard of competence in the area of diabetes as a special interest. It is the first postgraduate competence-based course to offer national accreditation in diabetes, run from within the NHS. In this regard, the course has been well received by key professional medical bodies. The programme is in the process of gaining the approval in its structure and clinical components by the Royal College of Physicians. It is being approved by the Royal College of General Practitioners (RCGP) in line with national guidance for GPs and other registered health professionals in higher professional education. The RCGP is now using the term Practitioners with a Special Interest (PwSI) to refer to all registered health practitioners who intend to work at an advanced level within a specialism and the course title reflects this. The course structure is specifically designed to encourage the development of this specialist practitioner role, by encouraging collaborative clinical work-based training between the GP/Practitioner and the consultant. Additionally, the course links the GP/Practitioner's training with their host Primary Care Trust (PCT) service, in order to attempt to ensure that newly acquired skills are put to appropriate use within the PCT post-qualification. Your learning will be channelled through the Bradford Primary Care Trusts, which have seen sustained national achievements for innovation in practice and excellence in training. Bradford Primary Care Trusts have been instrumental in moving the General Practitioner with a Special Interest (GPwSI) agenda forward nationally. In 1999, Bradford South and West Primary Care Group was awarded the Service Development Award of the National Association of Primary Care for its work on the role of the GPwSI and in 2001 achieved "Beacon" status for this aspect of its work. Equally the Commission for Health Improvement Reports on Clinical Governance gave the Bradford PCTs involved in the development of this course a commendation for their work with GPwSIs. A Programme Aims The programme is intended to: A.1 Enable GPs and other Practitioners to work independently at a ‘special interest’ level in Diabetes. A.2 Contribute to the extension of the role of the PwSI in Diabetes. A.3 Provide a nationally recognised standard in the training of PwSIs in Diabetes. A.4 Establish and/or extend professional collaboration within care of patients with diabetes, in order to develop the most appropriate care pathways for the patient. B. Programme Learning Outcomes These learning outcomes are compatible with the Framework for Higher Education Qualifications. On successful completion of this award, the Practitioner will be able to: B1 Subject knowledge and understanding Page 1 of 5 B1.1 Use current and emerging knowledge to apply an advanced critical appreciation of the pathophysiology and epidemiology of diabetes and its complications. B2 Discipline skills B2.1 Triage and refer appropriately, patients whose symptoms may be due to diabetes and its complications. B2.2 Undertake appropriate investigations for patients presenting with symptoms of diabetes and its complications and interpret the results accurately. B2.3 Diagnose and manage appropriately patients who present with diabetes and its complications, by means of clinical interventions. B2.4 Undertake appropriate evaluation and preventative management of patients with diabetes, addressing lifestyle and diabetes issues. B2.5 Evaluate the PwSI role, and its implications for the whole patient pathway and current techniques for improving the delivery of patient care. B3 Personal Transferable Skills B3.1 Work autonomously and collaboratively, in a multidisciplinary context. B3.2 Critically appraise and update clinical knowledge. B3.3 Apply information technology as a medium for communication and presentation of data. C The Curriculum The Postgraduate Diploma in Diabetes for Practitioners with a Special Interest is a modular programme which can be completed in 18 months if modules are taken sequentially, or may be staggered over a period not exceeding three years, excepting in exceptional circumstances, where study is proved viable over five years. Exceptional circumstances may include illness, pregnancy or long-term family crises, although each application will be taken on its merit. Each of the three clinical modules lasts six months. The fourth module is the Applied Methodologies (AM) module which can be taken alongside one or more of the other modules, over a maximum period of 18 months. Each module is worth 30 credits, amounting to a total of 120 credits. For the Postgraduate Diploma, all 30-credit modules are core modules. The curriculum is summarised in the following table: Module Unit title C (o) Credits Level Semester* code HH-8000T Applied Methodologies C 30 M 18 months HH-8013T Glycaemic Control C (o) 30 M 6 months HH-8014T Microvascular Management in Diabetes C (o) 30 M 6 months HH-8015T Macrovascular Management in Diabetes C (o) 30 M 6 months C = Core; (o) = Optional for a certificate *This programme is outside the normal semester timetable D Teaching Learning and Assessment Strategies This postgraduate diploma is run by Bradford and Airedale teaching Primary Care Trust (B&AtPCT). The award is made through the University of Bradford, and this award articulates with the Postgraduate requirements of the University of Bradford. A variety of learning methods is employed in the programme, to enable students to fulfil the varied modular learning outcomes. The programme of study starts with two teaching days in Bradford (one for the course introduction and the AM module, one for the first clinical module), followed by a clinical placement and directed study for at least 14 weeks (clinical modules). Alongside this, directed study for the AM module will begin, for up to 18 months. For clinical modules only, students will return to Bradford after placement for an assessment day. A large portion of study will be work-based learning, i.e. those elements of the programme, which take place in the student’s locality: 1 The clinical components of the programme centre around work-based learning, i.e. practical learning in a work environment. This learning is undertaken on placement in the locality, under the supervision of a clinical mentor. Students will approach the mentor in the first instance: he/she must be a GMC registered consultant diabetologist whose name appears on a national Page 2 of 5 register of practitioners, and who has teaching experience. The clinical mentor will receive a specific Mentor Guide including advice and support from the course management team in fulfilling the role of mentor. 2 The tasks for directed study on placement are as follows: the development and fulfilment of a programme of activities with the mentor, to fulfil clinical competence-based learning outcomes; recording 12 interesting placement cases using a learning diary, to reveal learning progress and learning needs; through guided reading, which underpins the knowledge base for the course, (in the form of lists and website references) obtaining essential background information to the module studied to inform the student’s practice and the preparation of assessed work; through scheduled meetings with his or her mentor, discussions concerning learning needs and possible solutions e.g. advice, further reading, alteration of elements of your programme. 3 The AM module involves working within the healthcare community to apply 3 different methodologies. Directed study comprises researching and reading information, planning, preparation and application of these. 4 It is anticipated that students will continue to work in their normal practitioner setting during the period of study, and it is expected that ongoing learning will be applied in this context. 5 Peer learning is encouraged through peer contact in Bradford during teaching/assessment days, and through participation in the online group learning environment. Outcome B1.1 will be developed through: lectures, seminars and workshops on the teaching/assessment days; a course manual; guided study via websites, journals and books; and mentor-led discussion of cases. Outcome B1.1 will be assessed through clinical case studies. Outcomes B2.1 - B2.4: will be developed through practical engagement with patients, mainly in the hospital setting, under the supervision and mentorship of the consultant and his/her team (supervision in community clinics may be included here); reflective discussion with the mentor; reflective learning through case study preparation and clinical logbook recording; the application of learning with patients in general practice; and will be supported by guided reading. These outcomes will be assessed principally by the mentor and other clinicians, who will observe and sign off the participant as competent. Additionally, the learning diary provides a record of the 12 most interesting cases experienced, and the case studies indicate the student’s ability to demonstrate skills coherently. Outcome B2.5: will be developed through lectures, seminar and workshop-style sessions, interviews with professionals in the service and with patients, and through guided study, especially of current NHS websites. Outcome B3.1: is intrinsic to the nature of the placement, and will be tested through continual mentor observation. Outcome B3.2: will be developed through lectures, guided study and the preparation of a selected case study for presentation. Assessment for outcomes B2.5-B3.2 will be made through submission of a critical appraisal paper, a patient pathway paper and a portfolio of evidence showing patient involvement methodologies. Outcome B3.3: will be developed and assessed through the submission of documentation for the course, especially within the AM module, and participation in online group learning environment learning. All written clinical assessments will be submitted by hand in Bradford on the assessment day following each modular placement. Submissions of assessed work are made electronically in the AM module. Assessments will be marked in accordance with the University of Bradford, School of Health Studies, Master's level marking criteria. E Admission Requirements The application process is divided into three parts: 1. Submission of an application form indicating that the applicant meets the professional/educational criteria. 2. Identification of a suitable mentor. 3. Submission of letters of support showing suitability for the applicant to undertake this course of study. To be accepted onto the Diploma, and to benefit from this course of study, potential students must meet the admission requirements for Masters level, as outlined by the University of Bradford, in addition to those required by B&AtPCT. Applicants should be registered practitioners (GMC, NMC or HPC as appropriate) falling within the following groups: General practitioner; diabetes specialist nurse; nurse practitioner; nurse consultant; hospital practitioner; other suitably qualified registered primary care practitioner. GPs are additionally required to provide their GP Qualification details and GMC registration number, and to show an interest or a background in diabetes. It is desirable, but not essential, for GPs to be Members of the Royal College of General Practitioners. If applicants are not GPs, they must provide evidence of a Diabetes-related diploma or equivalent; Page 3 of 5 several years' experience in diabetes care; and 2-3 years post-qualifying practitioner experience. It is desirable for candidates to have experience in postgraduate education. All applications will be judged on their own merit and prior learning experience. Once an application has been made for the programme, support must be obtained from the local NHS hospital trust diabetes consultant (GMC Registered) for mentorship and the provision of a placement. Support must also be obtained from the local Primary Care Trust, for approval and direct or indirect support for training, as it relates to the local setting. Without this evidence of support, candidates cannot be admitted on to the programme. Applications are welcomed from candidates with disabilities, who will be considered on the same academic grounds as all other applicants. F Admissions Policy There will be a maximum of 12 participants per clinical module, all of whom can access the Applied Methodologies module. The diploma is offered twice a year, with entry points in April and October. Groups must normally have a minimum of 6 participants to run. As the assessment elements of the postgraduate diploma require a substantial amount of written work at masters level, in accordance with regulations from the University of Bradford we ask that non-native speakers complete an IELTS English Language Exam at the required level before they begin their studies. G Progression Verification of clinical competence must be indicated by the consultant-mentor's signature on assessment day. Failure to present the signed documents which evidence this signify failure of the module, irrespective of other work presented. All written work and the case study presentation must also be presented on assessment day, in order for students to progress to the next module. The results of assessments will normally be made known in the six weeks following assessment day. All assessment tasks for all modules must be passed by attaining 40% of the full marks. Masters level marking criteria will be made available to help students check their work. Clinical competence is a pass/fail element, with no assessment percentage attached to it. Should students be unsuccessful in this element, they will be allowed to complete another 8 clinical sessions with the agreement of their consultant. A new study plan covering the areas of concern will be devised and signed off by the mentor. This should be returned within three weeks of dispatch of the letter detailing the requirement to resit. Students will normally have one opportunity to resit this element. Should they fail any other element of their assessments, one opportunity to resubmit work along the same lines as the sessional assessment will normally be allowed. In accordance with the Ordinances and Regulations of the University of Bradford, the following apply. To be eligible for a Postgraduate Diploma, all four 30-credit modules must be successfully completed, amounting to a total of 120 credits. For those who are not eligible for the Diploma, having successfully completed the Applied Methodologies and the Glycaemic Control module and possibly one other, the Post Graduate Certificate in Glycaemic Control may be awarded; the thresholds described above will also apply. Participants who do not succeed in the Glycaemic Control module will not qualify for any of the above awards, However, they may be eligible for the award of a Certificate of Continuing Education and may have their credits awarded. Exam boards will be scheduled as required to recommend completed awards. H Student support and guidance The course manual will support students in all aspects of work-based learning and assessment. Tutor support, during the placement period, will be provided by a system of email queries, initially. The course coordinator will handle enquiries of a general nature or allocate queries to tutors. Peer support is available to assist students with clinical questions through participation in the online group learning environment. It is anticipated that a significant amount of discussion relating to cases, working arrangements, progress, and approaches to study will result from this source. Support that can be expected from the mentor is outlined in the mentor guide (see rear of course manual). Mentors have the responsibility to ensure appropriate induction of the mentee, in order to identify any learning needs and direct the programme accordingly. Feedback and time for case discussion should be provided, allowing for confidential and focused discussion of pertinent professional experiences, as well as to encourage self-appraisal and assessment of clinical Page 4 of 5 competence. The guide also enables mentors to understand the support they will receive automatically, and can gain if required, from the course tutors. Participants will be represented on a Course Management Committee, and may give feedback about the course through this, in addition to the paper-based evaluation processes for end of unit (module) and stage (course) evaluation from the University of Bradford. Whilst students are made aware of support offered, they are also made aware of their responsibilities in the participant course manual: i.e. taking responsibility for organising their own learning, ensuring placement arrangements are acceptable; returning course forms/assessment submissions on time; attendance at the first teaching day and the concluding assessment day for each clinical module and at the initial teaching day for the applied methodologies module; patient confidentiality; working to a professional code of conduct; and alerting the course tutors to problems which will affect their training. Any complaints/appeals against marks should be made to the student co-ordinator in the first place, who will then forward this to the course team. The team will review the case, involving the appropriate tutor and/or mentor at its discretion if necessary. Should the complaint/appeal not be solved satisfactorily at this stage, the University’s appeals procedure will be invoked. Any appeals following an Assessment/ Examination Board should be made to the Education Lead, who will then forward this via the appropriate channels to the University. I Further Information/Disclaimers. For further details about the course including course dates, costs, and more detailed learning outcomes students should email: psi@bradford.nhs.uk. Changes in the above specification may be made at any time by B&AtPCT, but notification will be made as appropriate. Elements of the programme are subject to University conditions including its status as an approved course. The University reserves the right to alter or withdraw these elements at any time, and you will be notified by the B&AtPCT should this occur. Page 5 of 5