Intervenous Therapy
advertisement
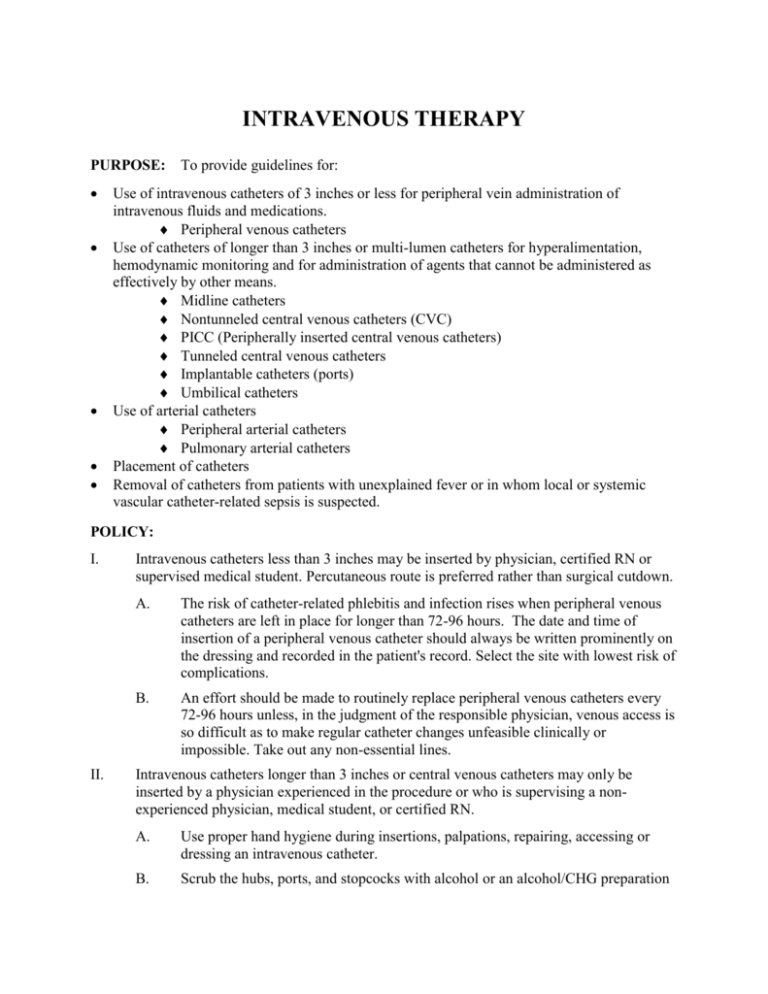
INTRAVENOUS THERAPY PURPOSE: To provide guidelines for: Use of intravenous catheters of 3 inches or less for peripheral vein administration of intravenous fluids and medications. Peripheral venous catheters Use of catheters of longer than 3 inches or multi-lumen catheters for hyperalimentation, hemodynamic monitoring and for administration of agents that cannot be administered as effectively by other means. Midline catheters Nontunneled central venous catheters (CVC) PICC (Peripherally inserted central venous catheters) Tunneled central venous catheters Implantable catheters (ports) Umbilical catheters Use of arterial catheters Peripheral arterial catheters Pulmonary arterial catheters Placement of catheters Removal of catheters from patients with unexplained fever or in whom local or systemic vascular catheter-related sepsis is suspected. POLICY: I. II. Intravenous catheters less than 3 inches may be inserted by physician, certified RN or supervised medical student. Percutaneous route is preferred rather than surgical cutdown. A. The risk of catheter-related phlebitis and infection rises when peripheral venous catheters are left in place for longer than 72-96 hours. The date and time of insertion of a peripheral venous catheter should always be written prominently on the dressing and recorded in the patient's record. Select the site with lowest risk of complications. B. An effort should be made to routinely replace peripheral venous catheters every 72-96 hours unless, in the judgment of the responsible physician, venous access is so difficult as to make regular catheter changes unfeasible clinically or impossible. Take out any non-essential lines. Intravenous catheters longer than 3 inches or central venous catheters may only be inserted by a physician experienced in the procedure or who is supervising a nonexperienced physician, medical student, or certified RN. A. Use proper hand hygiene during insertions, palpations, repairing, accessing or dressing an intravenous catheter. B. Scrub the hubs, ports, and stopcocks with alcohol or an alcohol/CHG preparation prior to access. Scrub the top and sides vigorously. C. Aseptic technique should be used during insertion and care. Sterile gloves should be worn for insertion of arterial and central catheters. D. Location of placement of central line site should be chosen to reduce complications of infections as well as potential mechanical complications. Remove non-essential lines. Use a CVC with the minimal amount of lumens needed to manage the patient clinically. E. Maximum sterile barrier precautions should be used for placement of CVC’s, PICC’s and during guidewire exchange. This includes: F. G. 1. Cap 2. Mask 3. Sterile gown 4. Sterile gloves 5. Large sterile drape. Disinfect skin with appropriate antiseptic before insertion. Chlorhexidine/alcohol, iodophor or 70% alcohol may be used. Povidone iodine must be allowed to dry prior to beginning insertion. Do not routinely replace central lines, PICC’s, hemodialysis catheters or pulmonary arterial catheters to prevent catheter-related infections. Use clinical judgment to evaluate appropriateness of line removal. 1. III. IV. Umbilical venous catheters should be removed as soon as possible when not needed but can be maintained aseptically for up to 14 days. Site care and maintenance of peripheral and central venous catheters A. Dressings may be transparent, sterile, semi-permeable material or sterile gauze. Replace dressing when it becomes wet, loose, soiled or to view site. Gauze dressings can be replaced every 2 days and 7 days for transparent dressings. When risk of dislodgement is a factor, time may be extended. B. Do not use topical antibiotic ointment or creams on insertion sites. C. Replace administration sets, add-ons and secondary sets no more frequently than 72 hours unless a problem develops. Tubing used to administer blood, blood products or lipids should be changed every 24 hours. D. Routine periodic site care is not required for peripheral venous catheters unless the dressing has become soiled or wet. E. Flushing or irrigation of the line should be avoided. Use of arterial catheters – additional recommendations. A. Sterilize reusable transducers according to the manufacturer’s instructions when disposable transducers are not available. Use disposable transducer assemblies when possible. B. Replace these every 96 hours, including all components of the system (tubing, flushing device and flush solution). V. C. When accessing the system through a diaphragm, use antiseptic first. D. Do not use solutions with dextrose or parenteral nutrition through the circuit. Removal of vascular catheters from patients with suspected sepsis A. Patients with unexplained fever or signs of systemic sepsis or any signs of local inflammation of the catheter site should always have the catheter removed and cultured by semiquantitative technique. Exception: some central catheters may be left in place in septic patients to allow for a trial of appropriate antimicrobial therapy to eradicate catheter related infections. In general, if the subcutaneous tunnel is obviously infected and certainly if the patient has not shown a satisfactory response to antimicrobial therapy within several days and the catheter is thought to be the probable source of septicemia, the catheter should be removed. B. Blood cultures should always be done if the patient has signs of sepsis. Ideally cultures should be taken peripherally and via the line. C. A notation should be made in the chart concerning local inflammation, pain and the presence or absence of pus upon compression of the puncture site after removal of the catheter. A physician should always be informed if purulence is expressed from the site. D. When contaminated fluid is suspected or found, the entire apparatus and unused fluid should be saved and the infection prevention department immediately notified. Major areas of emphasis, as noted in CDC Guidelines for Prevention of Intravascular Catheter-Related Infections include: 1. 2. 3. 4. 5. Reference: Education and training of personnel who insert and maintain catheters is essential. Maximum sterile barriers should be used when inserting central venous lines. 2% chlorhexidine preparation for skin antisepsis is recommended. Routine replacement of central venous catheters should be avoided. Antibiotic/antiseptic impregnated catheters may be considered for use if infection rate is high after institution of recommendations above. CDC, 2011 Guidelines for the Prevention of Intravascular Catheter-Related Infections, http://www.cdc.gov/hicpac/BSI/BSI-guidelines-2011.html Catheters used for venous and arterial access Catheter type Entry site Length Comments Peripheral venous catheters Usually inserted in veins of forearm or hand Peripheral arterial catheters Usually inserted in radial artery; can be placed in femoral, axillary, brachial, posterior tibial arteries Inserted via the antecubital fossa into the proximal basilic or cephalic veins; does not enter central veins, peripheral catheters >3 inches; rarely associated with bloodstream infection >3 inches; associated with bloodstream infection Phlebitis with prolonged use; rarely associated with bloodstream infection Low infection risk, rarely associated with bloodstream infection 3 to 8 inches Anaphylactoid reactions have been reported with catheters made of elastomeric hydrogel; lower rates of phlebitis than short peripheral catheters. Account for majority of CRBSI Midline catheters Percutaneously inserted into central veins (subclavian, internal jugular, or femoral) Inserted through a Teflon® introducer in a central vein (subclavian, internal jugular, or femoral) ≥8 cm, depending on patient size Inserted into basilic, cephalic, or brachial veins and enter the superior vena cava Implanted into subclavian, internal jugular, or femoral veins ≥20 cm depending on patient size Totally Implantable Tunneled beneath skin and have subcutaneous port accessed with a needle; implanted in subclavian or internal jugular vein. ≥8cm depending on patient size Umbilical catheters Inserted into either umbilical vein or umbilical artery ≥6 cm depending on patient size Nontunneled central venous catheters Pulmonary artery catheters Peripherally inserted central venous catheters (PICC) Tunneled central venous catheters Reference: ≥20 cm depending on patient size ≥8 cm depending on patient size Usually heparin bonded; similar rates of bloodstream infection as CVC’s; subclavian site preferred to reduce infection risk. Lower rate of infection than nontunneled CVC’s Cuff inhibits migration of organisms into catheter tract; lower rate of infection than nontunneled CVC’s Lowest risk for CRBSI; improved patient selfimage; no need for local catheter-site care; surgery required for catheter removal Risk for CRBSI similar with catheters placed in umbilical vein versus artery CDC, 2011 Guidelines for the Prevention of Intravascular Catheter-Related guidelines-2011.html Infections, http://www.cdc.gov/hicpac/BSI/BSI-