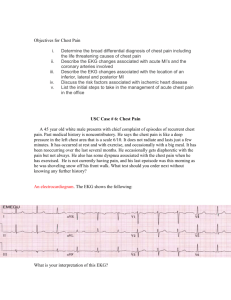
The use of EKG to exclude a diagnosis of acute coronary syndrome
advertisement

The use of EKG to exclude a diagnosis of acute coronary syndrome in a population with low-risk chest pain Alexander Leung1,3, Gaurav Puri, M.D.2, Vincent Ho, M.D.2, Steven Rhee, M.D.2 1 – MD Candidate 2015, Faculty of Medicine, University of Toronto, Toronto, Ontario, Canada, M5S 1A8 2 – Department of Emergency Medicine, St. Joseph’s Health Center, Toronto, Ontario, Canada, M6R 1B5 3 – To whom correspondence may be addressed. Email: alexander.leung@mail.utoronto.ca 1 Background: Chest pain is a common chief complaint to emergency departments (ED) across Canada. These patients often have low-risk chest pain where incidence of acute coronary syndrome (ACS) is minimal. The development of a strategy to assess low-risk chest pain could improve and accelerate patient care. Objective: To determine whether findings of a normal electrocardiogram (EKG) can rule out ACS in patients presenting with chest pain classified as low-risk in the ED. Methods: A retrospective chart review of patients presenting to the ED with low-risk chest pain, defined as patients between 16 and 40 years of age, was conducted in a medical center during a 1-year period from April 2011 to March 2012. Results: Medical charts from a total of 1019 patients between the ages of 16 and 40 with a chief complaint of chest pain were identified. The EKG had sensitivity and specificity values of 71% and 65% respectively. The positive predictive value and negative predictive value were 14% and 97% respectively. Post-hoc subgroup analysis was performed to assess EKG findings and ACS in age groups 16-20, 21-30 and 31-40 years of age, and the sensitivities and specificities were calculated. For those 16-20 years of age, the sensitivity and specificity were 80% and 77%, respectively. For those 21-30 years of age, the sensitivity and specificity were 50% and 64%. For those 31-40 years of age, the sensitivity and specificity were 77% and 64%. Conclusion: The use of EKG alone to exclude ACS is not recommended in patients presenting with low-risk chest pain. 2 Annually, approximately 500 000 Canadians present to emergency departments (ED) with chest pain, a symptom that raises concern of acute coronary syndrome (ACS). ACS encompasses unstable angina, ST-segment elevation myocardial infarction and non-ST segment elevation myocardial infarction.1 These patients undergo a lengthy assessment in the ED to rule out an acute myocardial infarction (AMI). This often involves testing two samples of blood collected 6 hours apart for biomarkers of myocardial necrosis, most frequently troponin.2 It is estimated that 20% of these patients are ultimately admitted with a diagnosis of acute coronary syndrome.1,3 Therefore, the majority of patients presenting with chest pain complaints do not have ACS.4,5 In addition, these patients may undergo additional diagnostic tests which can produce misleading results, thereby contributing to unnecessary inpatient hospitalizations and prolonged treatment.6 Diagnostic evaluation of chest pain in the ED remains a constant challenge to physicians. Extensive research has focused on developing strategies to risk-stratify chest pain patients with the likelihood for ACS. However, the majority of these studies involve patient populations above the age of 40 years.7-11 Accordingly, evidence-based strategies for the management of chest pain in younger patients in the ED is limited. Particular interest in this specific patient population is warranted, considering the increased potential years of life lost. 4% to 8% of patients diagnosed with ACS and 14% of chest pain visits to the ED are patients younger than 40 years of age.10,12 In general, patients in this age group present with chest pain where the incidence of life-threatening ACS is minimal. Furthermore, ACS in younger patients have different clinical presentations, receive earlier treatment and have a more favorable outcome relative to 3 older patients.12 Therefore, an age under 40 years is used as an objective and efficient measure to risk-stratify patients presenting with chest-pain into a ‘low-risk chest pain’ category where risk of ACS is low. Previous studies have shown that of patients presenting to the ED with chest pain, those with normal electrocardiogram (EKG) findings have lower rates of cardiac complications and mortality.13 However, in a general ED setting, Turnipseed et al. have shown that normal EKG findings do not exclude ACS in patients with chest pain. Their study population was predominantly over 40 years of age.14 We hypothesized that younger, “low-risk” patients presenting to the ED with chest pain and normal EKG findings would have a low rate of ACS diagnosis. Therefore, a normal EKG could be used to exclude the diagnosis of ACS in a low-risk chest pain patient presenting to the ED. Methods Study Design We conducted a retrospective chart review of patients at St. Joseph’s Health Center (SJHC). Inclusion criteria for this study were patients admitted to the ED with a chief complaint of chest pain between the ages of 16 and 40 years, irrespective of previous medical treatments or history, within a 1-year period from 1 April 2011 to 31 March 2012. The initial ED EKG interpretation by the attending physician and the first troponin value were collected. The EKG findings were then classified under “normal” or “abnormal” categories using pre-defined criteria, and the first troponin result was used 4 to determine ACS diagnosis. Patients without an EKG or troponin test result were excluded from the study. There was no re-interpretation of any clinical findings. The study was approved by the SJHC Research Ethics Board. Study Setting and Population All patients charts were reviewed at SJHC, a community hospital setting with an annual visit volume of approximately 100 000, and a catchment population over 500 000. It should be noted that patients with significant ST-segment elevation on the EKG during ambulance transportation were automatically re-directed to a designated regional hospital with cardiovascular intervention labs. Since this population of patients bypassed the hospital, they were excluded from the study. Study Protocol Patient charts were screened for inclusion criteria followed by a review for exclusion criteria by the study co-investigators. A chief complaint of chest pain was ascertained by first identifying the presenting complaint on the nursing triage note. This was compared to the chief complaint recorded by the attending physician on the emergency registration outpatient record. If the two records were consistent, the patient had a chief complaint of chest pain. Conversely, if there was a discrepancy, the chief complaint recorded on the outpatient record was used for data collection. The initial EKG findings on presentation to the ED were documented by the ED physician. From there, two patient groups were generated: patients with “normal” EKG findings and patients with “abnormal” EKG findings. Other clinical data recorded were age, sex, troponin I levels, and discharge diagnosis. 5 Criteria for “normal” EKG findings included: (1) heart rate of 55-105 beats/min and normal sinus rhythm or sinus arrhythmia, (2) normal sinus rhythm with left axis deviation up to -30°, (3) sinus rhythm with normal variant RSR’ patterns in leads V1 or V2, (4) normal QRS interval and ST segment, and (5) normal T-wave morphology. All other patterns were excluded and categorized as “abnormal,” which included any of: potentially pathologic Q waves, ST-T wave abnormalities, premature ventricular contractions, premature atrial contractions, ectopic and pacemaker rhythms, left ventricular hypertrophy, low voltage, and heart block. These criteria are consistent with EKG criteria used by Turnipseed et al.14 For the study, only the original EKG interpretation by the ED physician was used. Likewise, there was no reinterpretation of clinical findings. With the collected data, an outcome of ACS was defined by an elevation in troponin I level ≥0.07 μg/L (Cardiac Troponin I by Siemens Inc., NY, USA; 99th percentile of normal with <10% variance). Data Analysis Out of the study population, the total numbers for normal and abnormal EKG findings, and positive and negative ACS diagnostic results were collected and cross-tabulated. These cross-tabulations were used to calculate sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV). All values were multiplied by 100 to yield a percentage. For patients stratified by age, comparisons were made for sensitivity, specificity, PPV and NPV with the use of the χ2 test for associations. Microsoft Excel 2007 was used for analysis (Microsoft Corp., WA, USA). 6 Results Records of 1019 patients, aged 16 to 40 years old, who met the inclusion criteria and presented to the ED during the study period (1 April 2011 to 31 March 2012) for chest pain at SJHC were selected. From those patients, 153 were excluded according to the exclusion criteria, resulting in 866 study patients. Mean and median ages for the study population were 30 and 31 years, respectively. There were 79 persons within the ages of 16 to 20 years, 324 persons within the ages of 21 to 30 years, and 463 persons within the ages of 31 to 40 years. Patient demographics are summarized in Table 1. 541 (62.5%) patients had a “normal” EKG finding and 62 (7.16%) patients had a finding diagnostic of ACS, a positive troponin I value. The frequency of ACS in the study population was 7.2%. Of the patients with ACS, 18 persons (29.0%) had a diagnosis of ACS with a “normal” initial EKG and a positive troponin I result. 44 patients with ACS had an “abnormal” EKG and elevated troponin I values. Lastly, 281 (32.5%) persons had “abnormal” EKG findings and were found not to have ACS through troponin I testing (Table 2). Therefore, the EKG had sensitivity and specificity values of 71.0% (95% confidence interval [CI], 57.9% to 81.4%) and 65.0% (95% CI, 61.6% to 68.3%) respectively. The PPV and NPV were 13.5% (95% CI, 10.1% to 17.9%) and 96.7% (95% CI, 94.7% to 98.0%), respectively (Table 2). Post-hoc analysis was completed by dividing the total patient population into subgroups defined by the ages 16-20, 21-30 and 31-40 years. The statistical measures were calculated and are summarized in Table 3. The EKG sensitivities were: 16-20 year olds, 80.0% (95% CI, 29.9% to 98.9%); 7 21-30 year olds, 50.0% (95% CI, 24.0% to 76.0%), 31-40 year olds, 76.7% (95% CI, 61.0% to 87.7%). These differences were not statistically significant. Similarly, there were no significant differences in the specificity, PPV and NPV of the EKGs between the groups. Table 1: Demographics for study population (n = 866) Age Mean (and SD), years Median, years 30 (6.7) 31 Gender Male Female 347 519 Subgroups No. ages 16-20 years No. ages 21-30 years No. ages 31-40 years 79 324 463 Table 2: Overall accuracy of ACS diagnosis with “normal” EKG findings Diagnosis; no. of patients EKG Finding ACS No ACS Total no. of patients Abnormal Normal 44 18 281 523 325 541 Total no. of patients 62 804 866 Sensitivity 71.0% (44/62), 95% confidence interval (CI) 57.9%-81.4% Specificity 65.0% (523/804), 95% CI 61.6%-68.3% Positive predictive value 13.5% (44/325), 95% CI 10.1%-17.9% Negative predictive value 96.7% (523/541), 95% CI 94.7%-98.0% 8 Table 3: Subgroup Analysis; Sensitivity, specificity, PPV and NPV of the EKG in detection of ACS by age group Age range of subgroups (years) Parameters 16-20 21-30 31-40 Sensitivity 80.0 (4/5), 29.9-98.9 50.0 (7/14), 24.0-76.0 76.7 (33/43), 61.0-87.7 Specificity 77.0 (57/74), 65.5-85.7 63.9 (198/310), 58.2-69.2 63.8 (268/420), 59.0-68.4 PPV 19.0 (4/21), 6.29-42.6 5.90 (7/119), 2.60-12.2 17.8 (33/152), 12.8-24.3 NPV 98.3 (57/58), 89.5-99.9 96.6 (198/205), 92.8-98.5 96.4 (268/278), 93.3-98.2 Data expressed as a percentage (95% CI), calculations provided in brackets. None of the differences were statistically significant (χ2 test for association, p > 0.05). Discussion EKGs can be performed cheaply and rapidly at the time of patient presentation. The test also lacks the lengthy waits usually associated with cardiac biomarkers. These practical qualities are especially important in the ED, an environment where providing efficient care with limited resources and time is essential. For common presenting complaints like chest pain, the ability to quickly rule out life-threatening ACS would be extremely valuable. In the midst of advances in medical technology, physicians have numerous strategies available to assess chest pain in patients and identify ACS. This may make it tempting for ED physicians to perform additional tests to ensure a definitive exclusion of ACS. However, since chest pain in low-risk patients have diagnoses which are by and large benign, this "more is better" approach is not entirely acceptable in a time of escalating healthcare costs.6 Hence, given its low cost and practical advantages, studying whether a normal EKG can be used to exclude ACS in patients with low-risk chest pain is warranted. 9 We hypothesized that patients between the ages of 16 to 40 years presenting to the ED with chest pain would have the diagnosis of ACS ruled out if the initial EKG was normal. The overall sensitivity of the EKG in this young study population with low-risk chest pain was 71.0%. Of the 62 patients diagnosed with ACS, 44 had abnormal EKG findings while 18 had normal findings Our results demonstrate that for individuals between 16 and 40 years of age, in whom chest pain may be considered “low-risk”,12 a normal initial EKG is associated with a lower frequency of ACS compared to those with abnormal EKG findings. Despite this result, the sensitivity of the EKG in the overall study group was low. We then proposed that the sensitivities of EKGs might improve with age stratification: the younger a patient with chest pain, the more likely ACS could be excluded with normal EKGs. This improvement would also be seen in the specificity, PPV and NPV values. However, our results demonstrate that the ability of EKG to rule out ACS does not improve with younger age. There was no similar improvement in other statistical parameters as well. This significant type II error rate severely restricts the value of a normal EKG in excluding the diagnosis of ACS. These results are consistent with previous studies on the effectiveness of using normal EKG findings to exclude the diagnosis of ACS in a general ED population. Zalenski et al.15 showed that patients diagnosed with AMI who had normal EKGs on presentation did not have significantly lower complication rates than those with positive EKGs. They found that both groups had similar rates of hospital complications and intensive procedures. Similarly, Turnipseed et al.14 and Singer et al.16 showed that in cases of suspected ACS, irrespective of the presence of chest pain at that moment or the duration of symptoms from onset, obtaining a normal EKG finding does not reliably 10 exclude ACS. In the aforementioned studies, however, the mean age of the study population was over 50 years, a cohort which is at higher risk for ACS.14-17 Nevertheless, the studies build upon the notion that normal EKGs cannot be used to rule out ACS in any patient population, and our data is consistent with that conclusion.14,15 Singer et al.16 used the NPV of normal EKG findings to rule out AMI. For symptoms that lasted 0 to 3 hours from onset, the NPV of the EKG in the detection of AMI was 93.2% (95% CI, 87.4-96.1). Our study had a similar NPV of 96.7% (95% CI, 94.7-98.0). Despite their findings, Singer et al. concluded that many patients with a normal EKG would still require admission to reliably exclude ACS. Specifically, patients with high-risk unstable angina may present with normal EKG findings.16 Lastly, given the life-threatening and legal implications of ACS misdiagnosis, the risks associated with failure to diagnose cannot be ignored.18 Even with the practical advantages, the EKG alone does not fulfill the demand for a highly sensitive clinical test to exclude a diagnosis of ACS in patients with low-risk chest pain. Limitations This study has several limitations. Our patient population was identified at one community hospital and as a result, the study size was relatively small. The study also focused on patients presenting with a chief complaint of chest pain. However, the classic symptom of chest pain may not present in all cases of ACS, especially in young women.19,20 In addition, patients with ST-segment elevation during ambulance 11 transportation were not included the study. Secondly, the definition of low-risk chest pain varies widely.6 The criteria of age (16-40 years) used in this study to define low-risk chest pain may not be sufficient when other known cardiac risk factors and medical history could have been collected and utilized.8,14 In terms of diagnostic tests, EKG findings were not re-interpreted in the study and this may have impacted the accuracy and precision of the results. Furthermore, the criteria for abnormal EKG included findings that could be categorized as non-specific for ACS. This was done to facilitate the rapid analysis of EKG, a common practice demanded in the ED environment. As such, this would have increased the sensitivity of EKG. Due to limitations in acquiring patient data, our definition of ACS did not include results from imaging studies including echocardiography or coronary angiograms, which are more definitive tests for ACS.22 Also, the elapsed time between chest pain presentation and the initial troponin result was not included, and only the first troponin value was used. As a result, the troponin values used in the study may have been obtained before serum levels rose to detectable levels. This would lead to an underestimation of ACS.23 Troponin values can also be elevated in a variety of other clinical conditions which present with chest pain, including myocarditis and pulmonary embolus.24 Since these causes of chest pain were not excluded in the study, this would lead to over-diagnosis of ACS. Lastly, patients with misdiagnosed ACS may have been included in this study. 12 Conclusion This study demonstrates that in patients 16 to 40 years old with a chief complaint of chest pain at the emergency department, a normal electrocardiogram is not sensitive enough to reliably rule out acute coronary syndrome. Acknowledgements A.L. would like to thank the Comprehensive Research Experience for Medical Students (CREMS) Programs and the Jones, Janes and Howard O. Bursary Fund for providing the summer scholarship for this project. Conflicts of Interest The authors have no conflicts of interest to declare. References 1. Christenson J, Innes G, McKnight D, et al. Safety and efficiency of emergency department assessment of chest discomfort. CMAJ. 2004;170:1803-1807. 2. Anderson J, Adams CD, Antman EM, et al. 2011 ACCF/AHA Focused Update incorporated into the ACC/AHA 2007 Guidelines for the Management of Patients with Unstable Angina/Non-ST-Elevation Myocardial Infarction. Circulation. 2011;123:e426-e579. 3. Charles River Associates. The economical and societal burden of Acute Coronary Syndrome. Available at: http://www.crai.ca/uploadedFiles/RELATING_MATERIALS/Publications/files/B 13 urden%20of%20ACS%20in%20Canada_STC_151210Final%20(2).pdf (Accessed September 9th, 2012). 4. Ekelund U, Akbarzadeh M, Khoshnood A, et al. Likelihood of acute coronary syndrome in emergency department chest pain patients varies with time of presentation. BMC Res Notes. 2012;5:420. 5. Agostini-Miranda A, Crown L. An Approach to the Initial Care of Patients with Chest Pain in an Emergency Department Located in a Non-Cardiac Center. Am J Med. 2009;6:24-29. 6. Yiadom MY, Kosowsky JM. Management strategies for patients with low-risk chest pain in the emergency department. Curr Treat Options Cardiovasc Med. 2011;13:57-67. 7. Lee TC, Goodman S, Yan RT, et al. Disparities in management patterns and outcomes of patients with non-ST-elevation acute coronary syndrome with and without a history of cerebrovascular disease. Am J Cardiol. 2010;105:10831089. 8. Yan AT, Yan RT, Huynh T, et al. Understanding physicians’ risk stratification of acute coronary syndromes. Arch Intern Med. 2009;169:372-378. 9. Yan AT, Yan RT, Tan M, et al. Risk scores for risk stratification in acute coronary syndromes: useful but simpler not necessarily better. Eur Heart J. 2007; 28:1072-1078. 10. Marsan RJ, Shaver KJ, Sease KL, et al. Evaluation of a clinical decision rule for young adult patients with chest pain. Acad Emerg Med. 2005;12:26-31. 14 11. Schoenenberger AW, Radovanovic D, Stauffer JC, et al. Acute coronary syndromes in young patients: presentation, treatment and outcome. Int J Cardiol. 2011;148:300-304. 12. Goldman L, Cook EF, Johnson PA, et al. Prediction of the need for intensive care in patients who come to the emergency departments with acute chest pain. N Engl J Med. 1996;334:1498-1504. 13. Forest RS, Shofer FS, Sease KL, et al. Assessment of the standard reporting guidelines EKG classification system: the presenting EKG predicts 30-day outcomes. Ann Emerg Med. 2004;44:206-212. 14. Turnipseed SD, Trythall WS, Diercks DB, et al. Frequency of acute coronary syndrome in patients with normal electrocardiogram performed during presence or absence of chest pain. Acad Emerg Med. 2009;16:495-499. 15. Zalenski RJ, Rydman RJ, Sloan EP, et al. The emergency department electrocardiogram and hospital complications in myocardial infarction patients. Acad Emerg Med. 1996;3:318. 16. Singer AJ, Brogan GX, Valentine SM, et al. Effect of duration from symptom onset on the negative predictive value of a normal EKG for exclusion of acute myocardial infarction. Ann Emerg Med. 1997;29:575–579. 17. Welch RD, Zalenski RJ, Frederick PD, et al. Prognostic value of a normal or nonspecific initial electrocardiogram in acute myocardial infarction. JAMA. 2001;286:1977-1984. 18. Gallagher S, Wragg A. Medicolegal pitfalls in the management of chest pain. Clin Risk 2010;16:161-168. 15 19. Canto JG, Rogers WJ, Goldberg RJ, et al. Association of age and sex with myocardial infarction symptom presentation and in-hospital mortality. JAMA. 2012;307:813-822. 20. Alspach JG. Acute myocardial infarction without chest pain. Crit Care Nurse. 2012; 32:10-13. 21. Sharkey SW, Berger CR, Brunette D, et al. Impact of the electrocardiogram on the delivery of thrombolytic therapy for acute myocardial infarction. Am J Cardiol. 1994;73:550-553. 22. Bassand JP, Hamm CW, Ardissino D, et al. Guidelines for the diagnosis and treatment of non-ST elevation acute coronary syndromes. Eur Heart J. 2007;28:1598-1660. 23. Katus HA, Remppis A, Looser S, et al. Enzyme linked immuno assay of cardiac troponin T for the detection of acute myocardial infarction in patients. J Mol Cell Cardiol. 1989;21:1349-1353. 24. Burness CE, Beacock D, Channer KS. Pitfalls and problems of relying on serum troponin. QJM. 2005;98:365-371. 16