Acute Pyelonephritis Pathogenesis and Sources of Infection The
advertisement
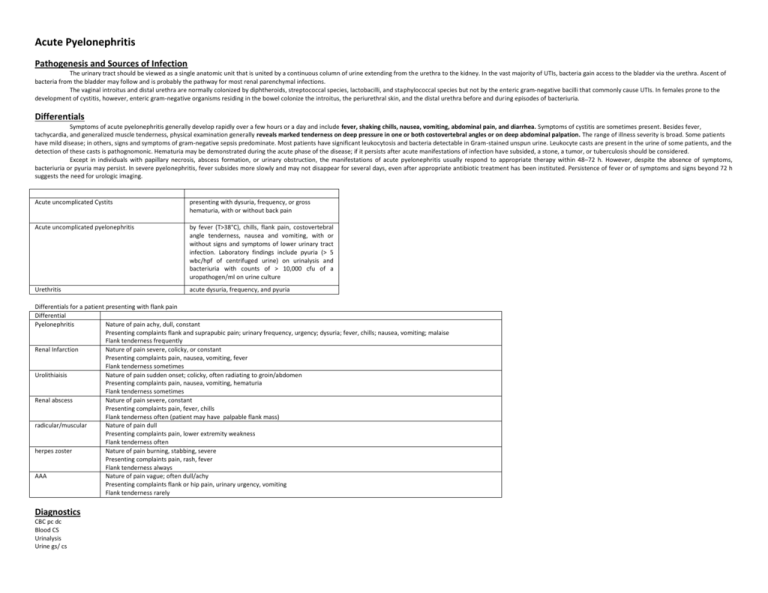
Acute Pyelonephritis Pathogenesis and Sources of Infection The urinary tract should be viewed as a single anatomic unit that is united by a continuous column of urine extending from the urethra to the kidney. In the vast majority of UTIs, bacteria gain access to the bladder via the urethra. Ascent of bacteria from the bladder may follow and is probably the pathway for most renal parenchymal infections. The vaginal introitus and distal urethra are normally colonized by diphtheroids, streptococcal species, lactobacilli, and staphylococcal species but not by the enteric gram-negative bacilli that commonly cause UTIs. In females prone to the development of cystitis, however, enteric gram-negative organisms residing in the bowel colonize the introitus, the periurethral skin, and the distal urethra before and during episodes of bacteriuria. Differentials Symptoms of acute pyelonephritis generally develop rapidly over a few hours or a day and include fever, shaking chills, nausea, vomiting, abdominal pain, and diarrhea. Symptoms of cystitis are sometimes present. Besides fever, tachycardia, and generalized muscle tenderness, physical examination generally reveals marked tenderness on deep pressure in one or both costovertebral angles or on deep abdominal palpation. The range of illness severity is broad. Some patients have mild disease; in others, signs and symptoms of gram-negative sepsis predominate. Most patients have significant leukocytosis and bacteria detectable in Gram-stained unspun urine. Leukocyte casts are present in the urine of some patients, and the detection of these casts is pathognomonic. Hematuria may be demonstrated during the acute phase of the disease; if it persists after acute manifestations of infection have subsided, a stone, a tumor, or tuberculosis should be considered. Except in individuals with papillary necrosis, abscess formation, or urinary obstruction, the manifestations of acute pyelonephritis usually respond to appropriate therapy within 48–72 h. However, despite the absence of symptoms, bacteriuria or pyuria may persist. In severe pyelonephritis, fever subsides more slowly and may not disappear for several days, even after appropriate antibiotic treatment has been instituted. Persistence of fever or of symptoms and signs beyond 72 h suggests the need for urologic imaging. Acute uncomplicated Cystits presenting with dysuria, frequency, or gross hematuria, with or without back pain Acute uncomplicated pyelonephritis by fever (T>38°C), chills, flank pain, costovertebral angle tenderness, nausea and vomiting, with or without signs and symptoms of lower urinary tract infection. Laboratory findings include pyuria (> 5 wbc/hpf of centrifuged urine) on urinalysis and bacteriuria with counts of > 10,000 cfu of a uropathogen/ml on urine culture Urethritis acute dysuria, frequency, and pyuria Differentials for a patient presenting with flank pain Differential Pyelonephritis Nature of pain achy, dull, constant Presenting complaints flank and suprapubic pain; urinary frequency, urgency; dysuria; fever, chills; nausea, vomiting; malaise Flank tenderness frequently Renal Infarction Nature of pain severe, colicky, or constant Presenting complaints pain, nausea, vomiting, fever Flank tenderness sometimes Urolithiaisis Nature of pain sudden onset; colicky, often radiating to groin/abdomen Presenting complaints pain, nausea, vomiting, hematuria Flank tenderness sometimes Renal abscess Nature of pain severe, constant Presenting complaints pain, fever, chills Flank tenderness often (patient may have palpable flank mass) radicular/muscular Nature of pain dull Presenting complaints pain, lower extremity weakness Flank tenderness often herpes zoster Nature of pain burning, stabbing, severe Presenting complaints pain, rash, fever Flank tenderness always AAA Nature of pain vague; often dull/achy Presenting complaints flank or hip pain, urinary urgency, vomiting Flank tenderness rarely Diagnostics CBC pc dc Blood CS Urinalysis Urine gs/ cs RBS, BUN, Crea Ultrasound of the kidneys Urine culture and sensitivity test should also be performed routinely to facilitate costeffective use of antimicrobial agents because of the potential for serious sequelae if an inappropriate antimicrobial regimen is used. Blood cultures are not routinely recommended (Grade D). Blood cultures done twice are recommended for patients who present with signs of sepsis defined as presence of any two of the following: temperature >38 0C or < 360C, leucopenia (WBC< 4,000) or leukocytosis (WBC > 12,000), tachycardia (HR>90 beats/min), tachypnea (RR> 20/min or PaCO2 <32mmHg), or hypotension (SBP< 90mmHg or >40mmHg drop from baseline) (Grade C). PLAN The following principles underlie the treatment of UTIs: Except in acute uncomplicated cystitis in women, a quantitative urine culture or a comparable alternative diagnostic test should be performed to confirm infection before empirical treatment is begun, and antimicrobial sensitivity testing should be used to direct therapy. Factors predisposing to infection, such as obstruction and calculi, should be identified and corrected if possible. Relief of clinical symptoms does not always indicate bacteriologic cure. Each course of treatment should be classified after its completion as a failure (symptoms and/or bacteriuria not eradicated during therapy or in the immediate posttreatment culture) or a cure (resolution of symptoms and elimination of bacteriuria). Recurrent infections should be classified as same-strain or different-strain and as early (occurring within 2 weeks of the end of therapy) or late. In general, uncomplicated infections confined to the lower urinary tract respond to short courses of therapy, while upper tract infections require longer treatment. After therapy, early recurrences due to the same strain may result from an unresolved upper tract focus of infection but often (especially after short-course therapy for cystitis) result from persistent vaginal colonization. Recurrences >2 weeks after the cessation of therapy nearly always represent reinfection with a new strain or with the previously infecting strain that has persisted in the vaginal and rectal flora. Despite increasing resistance, community-acquired infections (especially initial infections) are usually due to relatively antibiotic-sensitive strains. In patients with repeated infections, instrumentation, or recent hospitalization, the presence of antibiotic-resistant strains should be suspected. Although many antimicrobial agents reach high concentrations in urine, in vitro resistance usually predicts a substantially higher failure rate. The following are considered as indications for admission: inability to maintain oral hydration or take medications; concern about compliance; presence of possible complicating conditions; severe illness with high fever, severe pain, marked debility and signs of sepsis (Grade B). ADMITTING ORDERS Admit to: W___ B ___ or ICU if with severe malaria Diet: DAT VS: VS Q4 with temp IVF: D5NM 1L x 8hrs Diagnostics: as above Therapeutics: IV antibiotics can be shifted to any of the listed oral antibiotics (Table 6) once the patient is afebrile and can tolerate oral drugs (Grade B). The choice of continued antibiotic therapy should be guided by the urine culture and sensitivity results once available (Grade B). References CPG UTI guidelines 2004 Harrisons