SYSTEMIC SCLEROSIS (SSc)
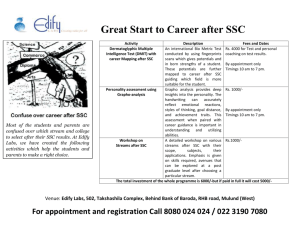
advertisement

SYSTEMIC SCLEROSIS (SSc) Systemic sclerosis is a chronic disease of unknown cause characterized by affection of small blood vessels and excessive synthesis and accumulation of extracellular matrix proteins (collagens, glycosaminoglycans, fibronectin) resulting in fibrosis and obliteration of vessels and tissue ischemia. Vascular endothelial damage and autoimmunity are thought to be important in the pathogenesis of this condition. The disease most characteristically involves the skin which becomes thick and tightly bound to underlying structures. The internal organs commonly involved are gastrointestinal tract, lungs, kidneys, and heart. The prognosis of the disease largely depends on the degree and extent of visceral involvement, particularly the lung and the kidney. Apart from the multisystemic, progressive and often fatal form of the disease known also as systemic sclerosis (systemic scleroderma, SSc), scleroderma may also occur as localized and circumscribed forms (like morphea and linear scleroderma) in which the internal organs are spared. Epidemiology This disorder is relatively rare. The peak age of onset is in the fourth and fifth decades, and overall prevalence is 10-20 per 100 000 with a 4:1 female preponderance. The mortality is highly variable and depends upon the extent and location of disease. Classification The extent of skin involvement bears close correlation with the degree and extent of internal organ disease. Based mainly on the extent of skin change, SSc can be classified into two subsets even though there is some overlap One subset is called diffuse cutaneous SSC and is characterized by the rapid development of symmetric skin thickening of proximal and distal extremities, face, and trunk and early involvement of kidney and other internal organs The other subset is called limited cutaneous SSC , typified by symmetric skin thickening limited to distal extremities and face. This subset may show features of the CREST syndrome, (calcinosis, Raynaud's phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia.) The prognosis in limited cutaneous is generally better. Systemic sclerosis sine scleroderma refers to visceral disease in absence of skin manifestations. Prognosis depends on the severity of involvement of internal organs, particularly the lungs, heart, and kidneys. The following types are recognized: Diffuse cutaneous SSc Onset of skin changes within 1 year of onset of Raynaud's phenomenon Truncal and acral skin involvement Tendon friction rubs Visceral disease : interstitial lung disease, renal failure, diffuse gastrointestinal disease, myocardial involvement Nail fold capillary dilatation and drop out Antitopoisomerase-l (Scl-70) antibodies (30% of patients) Limited cutaneous SSc Raynaud's phenomenon for years (occasionally decades) Skin involvement limited to hands, face, feet, and forearms (acral) Skin calcification, telangiectasia, and gastrointestinal involvement Dilated nail fold capillary loops, usually without capillary dropout A significant (10–15%) late incidence of pulmonary hypertension, with or without interstitial lung disease, primary biliary cirrhosis may occur. High prevalence (70–80%) of anti-centromere antibodies (ACA) Scleroderma sine scleroderma Raynaud's phenomenon No skin involvement Presentation with pulmonary fibrosis, renal crisis, cardiac or gastrointestinal disease Antibodies may be present (Scl-70, ACA, nucleolar) Overlap syndrome Systemic sclerosis occurring in association with features of other connective tissue diseases like SLE or rheumatoid arthritis. Mixed connective tissue disease (MCTD) is a syndrome showing features of SSc, systemic lupus erythematosus (SLE), , polymyositis, and rheumatoid arthritis and very high titers of circulating antibody to nuclear ribonucleoprotein (RNP) antigen. Undifferentiated connective tissue disease Patients who do not fulfill diagnostic criteria of any one particular connective tissue disease are classified in this group. Scleroderma-Like Disorders Cutaneous changes similar to scleroderma with or without other features like Raynaud’s phenomenon or pulmonary fibrosis may be observed in a number of patients who have been exposed to certain environmental toxins or drugs. Underground coal and gold miners are more likely to develop SSc owing to exposure to silica dust. An unusual form of scleroderma featuring Raynaud's phenomenon, skin changes, capillary abnormalities of the nail fold), osteolysis of the distal phalanges, and hepatic and pulmonary fibrosis may occur in workers exposed to polyvinyl chloride. Other agents connected with sclerodermatous disease include epoxy resins, industrial solvents, bleomycin, pentazocine, cocaine and denatured rapeseed oil. Scleroderma-like skin changes may be associated with scleromyxedema, porphyria cutanea tarda, and graft-versus-host (GVH) disease. Similar skin changes, primarily in the legs, may occur in the carcinoid Pathogenesis CD4 T-cells accumulate in the skin, release cytokines which in turn recruit various inflammatory cells. These in turn release various mediators(TGF-beta, IL-4, platelet derived growth factor) which upregulate genes encoding extracellular matrix proteins and collagen. Consequently, there is collagen deposition in the affected tissue. Another feature is microvascular disease induced by various mediators, presumably causing endothelial injury, and all patients with this disorder have intimal fibrosis in digital arteries. Pathology Characterized by excess collagen deposition in various tissues. In the skin the process begins with edema, which is followed by fibrosis and then atrophy. In the esophagus this causes fibrosis and impaired esophageal motility. Interstitial fibrosis can occur in the lung and intimal proliferation of blood vessels occurs in the kidney in some patients. Clinical features The patients most commonly present with Raynaud’s phenomenon on cold exposure. Some patients develop swelling of the hands which remain for a variable time before developing skin thickening. Symmetric joint pain and features of gastroesophageal reflux disease are other common presentations. Skin The skin changes on the hands may start with a non-pitting edema which is followed by induration and thickening of the skin which is bound tightly to the underlying structures. A long interval between the onset of edema and development of sclerosis carries a favorable prognosis. Rapid progression of sclerosis is often associated with extensive and severe internal organ involvement. Once sclerosis develops, the skin appears thick and tight with loss of hair and diminished sweating. It becomes difficult to raise a fold of skin. Thickening of the skin starts in the fingers and progresses proximally. Limited cutaneous scleroderma involves areas distal to the elbow and knee but may involve the face and neck. In the diffuse cutaneous variety of SSc ,the skin thickening affects the trunk and proximal aspects of the extremities in addition to the face and acral portions of the body. The face of the patients acquires a characteristics look: the skin is shiny and tightly bound, resulting in a loss of the facial expression lines. The skin over the nose sits tightly on the bone giving rise to a beak-like appearance. The lip becomes thin and the opening of the mouth gets smaller (microstomia). Linear furrows radiate from the angles of the mouth. Tightening of the skin makes it difficult for depressing the lower eyelid with fingers. The hands provide valuable clues to the diagnosis: the fingers are spindleshaped, with flexion contractures. Loss of substance from the finger pulp with small ulcers which heal with stellate-shaper scars are characteristic. There may be dilated nail-fold capillaries and ragged cuticles. Pigmentary changes include a mottled hypo- and hyperpigmentation (salt and pepper appearance) Telangiectasias are persistently dilated small blood vessels located on any skin area, but they are most obvious in the face (perioral area) and the neck. Calcification may occur on the fingertips and extremities, however, any area involved with scleroderma can be affected These calcifications may ulcerate, extrude calcified material, and heals very slowly. Vascular changes Raynaud phenomenon results from abnormal vasomotor control secondary to the microvascular damage of SSc and is characterized by sequential color changes of pallor, cyanosis, and then erythema (white, blue, red) accompanied by numbness, tingling, or pain. These events may be triggered by cold, smoking, vibration or emotional stress. Raynaud phenomenon may precede sclerosis of skin by months or even years. In diffuse cutaneous SSc, this time interval is usually less than a year, while sclerosis may occur years after the onset of Raynaud’s in the limited cutaneous form of the disease. Isolated Raynaud’s phenomenon without any underlying disorder (Raynaud’s disease ) carries excellent prognosis. A small minority of this population may eventually develop scleroderma. Severe vasospasm may lead to infarction and dry gangrene of the digits. Nail fold capillary microscopy (done with an ophthalmoscope) shows dilated capillary loops. In diffuse cutaneous SSc, some loops are destroyed giving rise to fewer than normal number of capillaries (capillary drop-out). Musculoskeletal system Pain, swelling, and stiffness of the fingers and knees is a common complaint Generalized arthralgias and morning stiffness may mimic rheumatoid arthritis. Thickening and tightening of overlying skin may impair mobility of joints. Palpable tendon friction rubs may be detected over moving joints as the tendon is moved actively or passively, Muscle weakness in advanced cases due to disuse atrophy. A proximal myopathy with muscle enzyme elevations may also occur. Acro-osteolysis (ie, resorption or dissolution of the distal end of the phalanx) may occur. . In addition to terminal phalanges, resorption of bone may involve ribs, clavicle, and angle of mandible. Any joint may be affected with flexion contracture. Gastrointestinal system Gastro-esophageal reflux disease from lower gastro-esophageal sphincter tone. Dysphagia due to atony of esophagus Esophagitis Barrett metaplasia Watermelon stomach (streaks of dilated submucosal capillaries seen with endoscope) Malabsorption Wide-mouth diverticula of the colon Decreased peristalsis throughout the GI tract leading to constipation and pseudoobstruction. Anal sphincter incompetence Primary biliary cirrhosis associated with antimitochondrial antibodies Respiratory system Pulmonary involvement is very common and is the leading cause of mortality. Interstitial fibrosis is the predominant pathology and occur more commonly with the diffuse cutaneous SSc. The most common symptom is exertional dyspnea, often accompanied by a dry cough. Bilateral basilar rales may be present. Pulmonary arterial hypertension some patients with limited cutaneous SSc. Aspiration pneumonia resulting from gastric reflux Chest movement may be restricted by severe sclerotic changes of the skin over the thorax. Superimposed bacterial or viral infection Increased frequency of alveolar cell and bronchogenic carcinoma Kidney Scleroderma renal disease is commoner in diffuse cutaneous SSC. Patients with rapidly developing diffuse scleroderma are at high risk of developing renal crisis Renal crisis presents as malignant hypertension with encephalopathy, retinopathy, severe headache, seizure and a rapidly rising serum creatinine. If untreated, this may lead to renal failure. In some patients , renal crisis may occur in the absence of hypertension. Renal crisis carries a high mortality if not treated appropriately. Heart Pericardial effusions Cor pulmonale may occur as a result of long-standing pulmonary fibrosis. Left ventricular failure from severe hypertension. Conduction abnormalities and arrythmias. Infiltrative cardiomyopathy Musculoskeletal system Pain, swelling, and stiffness of the fingers and knees is a common complaint Generalized arthralgias and morning stiffness may mimic rheumatoid arthritis. Thickening and tightening of overlying skin may impair mobility of joints. Palpable tendon friction rubs may be detected over moving joints as the tendon is moved actively or passively, Muscle weakness in advanced cases due to disuse atrophy. A proximal myopathy with muscle enzyme elevations may also occur. Acro-osteolysis (ie, resorption or dissolution of the distal end of the phalanx) may occur. . In addition to terminal phalanges, resorption of bone may involve ribs, clavicle, and angle of mandible. Any joint may be affected with flexion contracture. Nervous system Trigeminal neuralgia (uncommon) and carpal tunnel symptoms may result from peripheral entrapment neuropathies. The central nervous system (CNS) is spared. Obstetrics and gynecology Vaginal dryness, dyspareunia, and menstrual irregularities. Higher pregnancy loss and complication rates, but a diagnosis of scleroderma is not an absolute contraindication for pregnancy. During pregnancy, some symptoms may increase (eg, edema, arthralgias, reflux disease). Other manifestations: Hypothyroidism from fibrosis and autoantibodies. Erectile dysfunction in males. Loosening of teeth due to thickening of periodontal membrane and alteration of tooth suspensory ligament. Dry mouth and eyes (sicca syndrome) Constitutional features: weakness and weight loss. Investigations Routine haemogram: May reveal anemia. Urinalysis: For proteinuria , hematuria, casts . Biochemical : Blood urea ,creatinine, Liver function tests. Thyroid function tests, Muscle enzymes Immunological: Antinuclear antibodies are present in about 95% of the patients A nucleolar pattern is more specific than other patterns. Antibodies to Topoisomerase I (formerly Scl–70) is present in about onefourth of patients with diffuse cutaneous SSc (negative in limited disease ) and has an increased association with pulmonary fibrosis. Anticentromere antibodies : present in about 60-90% of patients with limited disease and 10-15% with diffuse disease. Fibrillarin antibodies (antibody to U3 ribonucleoprotein) are also relatively specific findings in diffuse disease. Antibodies to U3-ribonucleoprotein( U3 RNP) is present mostly in patients with diffuse disease and overlap syndromes. Anti-PM-Scl is present in limited and disease with SSc-polymyositis overlap. Imaging X-rays: Chest: May show evidence of pulmonary fibrosis: linear shadows, mottling or honeycombing particularly involving the basilar areas of lung. Extremities: soft tissue calcinosis and bony changes like absorption of terminal digits may be demonstrated. Barium studies CT scan High-resolution CT scan may reveal a ground-glass appearance indicative of active alveolitis. Echocardiogram For evaluation of pulmonary arterial pressure and pericardial effusion. Other Tests: Pulmonary function testing Examination of bronchoalveolar lavage: the cellular pattern may indicate active alveolitis. Cardiac rhythm monitoring.24-hour ambulatory Hotter monitoring to evaluate arrhythmias. Esophagogastroduodenoscopy, esophageal manometry Treatment: There is no cure for scleroderma. Treatment is aimed at relieving symptoms improving functions. Reassurance and explanations of the nature and course of the disease should be undertaken with a sympathetic attitude. Regular monitoring of blood pressure, blood count, urinalysis, and renal and pulmonary functions is indicated. Raynaud’s phenomenon: Avoidance of cold exposure and smoking cessation, warm clothing. Calcium channel blockers (Nifedipine, diltiazem) Aspirin and dipyridamole, pentoxifylline Losartan, Ketanserin, Fluoxetine Topical nitroglycerine paste over digits Intravenous alprostadil, and prostaglandin in sever Raynaud’s Skin fibrosis: A number of agents are used but few have been properly evaluated for efficacy. Penicillamine Colchicine, paraaminobenzoate, Relaxin Gamma interferon Cyclosporine Extracorporeal photochemotherapy GI symptoms: Antacids, H2-blockers, proton-pump inhibitors Prokinetic agents, octreotide Reflux precautions: frequent small meals, elevation of head end of the bed, not lying after meals, avoidance of tea, coffee, alcohol, spicy and fatty meals. Antibiotics for treatment of bacterial overgrowth and malabsorption. Pulmonary disease : Pulmonary fibrosis may be treated with systemic steroid and cyclophosphamide. Sever pulmonary hypertension may be benefitted by intravenous or aerosolized prostacyclin. Prompt treatment of infections. Renal disease Early management of hypertension with calcium channel blocker. Management of renal failure, Dialysis. Cardiovascular disease Treatment of heart failure. Pericarditis may respond to systemic steroids. Musculoskeletal symptoms: NSAIDs and paracetamol for arthralgia Myositis may be treated with steroids, methotrexate and azathioprine. Course and prognosis Course of the disease is variable, the prognosis largely dependant of the severity and extent of internal organ involvement particularly pulmonary and renal disease . Indicators for poor prognosis include: Advanced age at presentation Male sex Black American race Diffuse cutaneous involvement. Patients with diffuse disease has a 10 year survival rate of about 20% Rapidity of development of skin involvement. Presence of significant renal of pulmonary disease . Presence of anti-Scl 70 antibodies. MIXED CONNECTIVE TISSUE DISEASE (MCTD) Mixed connective tissue disease (MCTD) is an uncommon autoimmune disorder that causes overlapping features of primarily three connective tissue diseases — lupus, scleroderma and polymyositis. Mixed connective tissue disease also may have features of rheumatoid arthritis. Mixed connective tissue disease occurs most often in women and is usually diagnosed in their 20s and 30s. Occasionally children are diagnosed with mixed connective tissue disease. Clinical features Early indications of mixed connective tissue disease typically are nonspecific and may be mistaken for any of the three connective tissue diseases — lupus, scleroderma and polymyositis. Signs and symptoms include: Raynaud's disease — blood vessel spasms that interrupt blood flow to the fingers, toes, ears and nose Fatigue General feeling of being unwell (malaise) Muscle pains / weakness Joint pains Mild fever Joint swelling Swollen hands and puffy fingers Raynaud's phenomenon may begin years before other symptoms. As the disease progresses, it can affect any of the major organ systems, including skin, joints, muscles, heart, lungs, gastrointestinal tract, kidneys, central nervous system and blood cells. Mixed connective tissue disease and its treatment can lead to serious complications, including: Pulmonary hypertension. Pulmonary hypertension is the most common cause of death in people with mixed connective tissue disease. Heart disease including myocarditis and pericarditis. Side effects of long-term corticosteroid use. Pregnancy complications. There are conflicting studies, some of which suggest that women with mixed connective tissue disease may experience flares during pregnancy. Babies born to women with mixed connective tissue disease are at risk of being born with a low birth weight. Investigations The presence of this specific antibody, U1-RNP can help confirm the diagnosis of MCTD. Treatments and drugs There's no cure for mixed connective tissue disease, but medication can help manage the signs and symptoms of the disease. Mild forms of mixed connective tissue disease may not require treatment. Patients may require treatment only during flares or, if they have a more serious form of the disease, they may require continuous medication. Medications may include: Small dose of corticosteroids. These are the most common treatment for moderate mixed connective tissue disease. NSAIDS. Nonsteroidal anti-inflammatory drugs (NSAIDs) can relieve pain and reduce inflammation. Other immunosuppressants. Same indications for SLE.