Neuromuscular
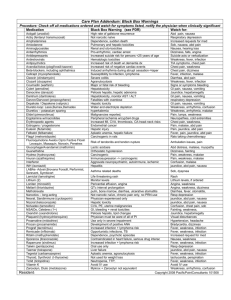
advertisement
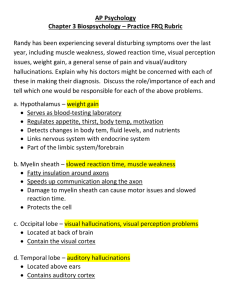
Neuromuscular Questions: 1. A 3 ½ month old previously vigorous baby is brought to the ER by her parents with complains that the infant has constipation, shortness of breath, and a recent loss of spontaneous movements giving the appearance of a limp doll. On exam, the infant is floppy and has some respiratory distress. The most likely diagnosis is: A. Spinal Muscular Atrophy B. Hypomyelinating neuropathy C. Transverse myelitis D. Infantile botulism E. Muscular dystrophy 2. An 18 year old college student competed in the 400-meter dash for the first time. That evening, his muscles were very sore and he passed dark urine. His creatine kinase was 24,000. He came to the university hospital where they consult you for evaluation. Her neurological examination and muscle EMG 3 weeks later were normal. The next most useful clinical test would be: A. Repetitive Nerve Stimulation B. An ischemic exercise test for a defect in glycogen metabolism C. An ischemic exercise test for a defect in lipid metabolism D. Nerve conduction studies E. A search for occult neoplasm 3. (45, 2008.) A 60 year old female develops nausea, vomiting, abdominal cramping and diarrhea with rapid evolution of blurry and double vision, ptosis, dysarthria and dysphagia. Examination after 14 hours of symptoms reveals external and internal Ophthalmoparesis, ptosis, orthosis hypotension, and weakness of the face, palate and tongue in the context of normal sensorium. DTRs are difficult to elicit, and plantar responses are flexor. The abnormality underlying this patient’s symptoms may best be characterized by: A. Antibody binding to the alpha-subunit of the acetylcholine receptor B. Reduction of presynaptic calcium current related to antibodies directed against P/Q type voltage gated calcium channels at the nicotinic cholinergic synapses C. Reduced number and density of acetylcholine receptors at the postsynaptic membrane due to cross linkage of antibodies and complement fixation D. Cleavage of a soluble N-ethylmaleimide sensitive fusion associated protein receptor protein by a zinc endopeptidase E. Anti-GT1a antibodies binding to myelin epitopes specific for cranial nerves 4. You are consulted from the LTAC on a patient who has been transferred from an outside facility with the diagnosis of Statin-induced myopathy. The patient is a 70 year old female with a history of progressive weakness for 6 months. She was taking a statin for one year but she stopped it three months ago because of her weakness and elevated creatine kinase (CK) of 8,000 u/L. Muscle biopsy revealed abundant necrotic muscle fibers. Her strength has continued to decline is she is no longer ambulatory. Examination reveals proximal greater than distal weakness, sparing ocular and bulbar muscles. Sensation is normal. What should be the best next step in management? A. B. C. D. E. Repeat the muscle biopsy Start prednisone and methotrexate Perform an electromyographic study Resume treatment with other statin Perform genetic testing for AR forms of LGMD 5. A 59 year old male presents to the ER department with acute low back pain that refers into the left leg. Physical examination of the left lower limb demonstrates an absent patellar reflex, quadriceps weakness and decreased sensation in the medial leg. An MRI of the lumbar spine without contrast showed no structural abnormalities or nerve root impingement. Which laboratory study will be most helpful in determining the cause of the patient’s symptoms? A. Thyroid stimulating hormone B. Creatine kinase C. Hemoglobin A1C D. Urine porphyrins E. Serum folate 6. A 23 year old female has a 4-month history of facial weakness, severe neck extensor weakness and progressive dysphagia. You performed a RNS at 3 Hz recorded in the nasalis muscle and she has a significant decremental response. After starting her on pyridostigmine she developed profuse fasciculations without improved strength, but with excellent response to plasma exchange. Which diagnosis is most likely? A. Amyotrophic lateral sclerosis B. Kennedy disease C. MuSK myasthenia gravis D. DOK7 congenital myasthenia syndrome E. Dermatomyositis 7. A patient is brought to the ER Department with a suspected attack of hypokalemic periodic paralysis. Which clinical finding would be most consistent with this diagnosis? A. Ophthalmoplegia B. Altered consciousness C. Diminished deep tendon reflexes D. Percussion myotonia of thenar muscles E. Anarthria 8. Following normal development, a 4 month-old infant develops a weak cry, reduced ability to suck, hypotonia and constipation over 2 days. RNS studies at 50 Hz elicit sustained 120% facilitation of the CMAP amplitude in the abductor digiti quinti. The best initial treatment is administration of: A. Clindamycin B. C. D. E. Guanidine Neostigmine bromide 3,4 diaminopyridine Botulism immune globlulin IV (human) 9. A 25 year old male underwent a surgical procedure on his right knee under general anesthesia. During the procedure, his arms were abducted to 90 degrees and at one point he was placed in the Trendelenburg position. Two days postoperatively, he complained of subacute, intense pain along the lateral aspect of his right shoulder. The severe pain persisted for 3-4 days at which point it was replaced by a dull aching sensation. Around this time he became aware of severe right upper extremity weakness. Abnormalities noted on examination included an inability to flex the right forearm (2/5) and winging of the right scapula. These findings most likely reflect: A. Upper trunk brachial plexopathy related to the Trendelenburg position B. Ligamentous stretch injury related to the crucifix position C. Neuralgic amyotrophy D. Rotator cuff tear E. C5-C6 radiculopathy related to neck hyperextension 10. A female with bulbar myasthenia gravis began treatment with an unknown immune suppressive medication and developed increased weakness and respiratory failure 4 days later. Which medication would be most likely to cause this event? A. Azathioprine B. Mycophenolate mofetil C. Cyclosphophamide D. Prednisone E. Methotrexate 11. You are consulted for evaluation of a patient with suspected acute motor axonal neuropathy variant of Guillain-Barre Syndrome (GBS). Which antibody is most strongly associated to this variant of GBS? A. GQ1b B. GM1 C. GT1a D. Myelin protein zero E. Myelin associated glycoprotein 12. A patient presents with acute ophthalmplegia, unsteady gait, and absent DTRs. Testing for which antibody is most appropriate? A. Anti- GM1 B. Anti- GQ1b C. Anti- Myelin associated glycoprotein D. Anti-Neuronal nuclear antibody, type 1 (Hu-type) E. Anti-sulfatide 13. Which of the following best represents an indication for urgent surgical decompression of a large midline lumbar disk herniation identified by radiographic imaging studies? A. Positive straight leg raise maneuvers B. Absent lower limb proprioception C. Lower limb paresthesias and dysesthesias D. Steppage gait pattern E. Absent medial hamstring and Achilles tendon reflexes 14. A middle aged male develops acral paresthesias and difficulty walking and standing over 8 days. Bowel and bladder function are normal. Examination reveals mild bifacial and limb weakness and areflexia. EDX studies demonstrate prolonged F-waves latencies, motor conduction block in the left median nerve, absent lower extremity CMAPs, and a normal sural sensory potential. What is the optimal treatment for this patient? A. IV methylprednisolone 500 mg every 12 hours over 10 days B. Plasma exchange 250 ml/kg over 10 days C. Plasma exchange 250 ml/kg over 10 days followed by intravenous immunoglobulin (IVIG) infusion 2 gm/kg over 2 or more days D. Plasma exchange 250 ml/kg over 10 days concurrently with methylprednisolone 500 mg every 12 hours over 10 days E. Intravenous immunoglobulin (IVIG) infusion 2 gm/kg over 2 or more days with concurrent with methylprednisolone 500 mg every 12 hours over 10 days 15. A patient with seropositive, bulbar MG begins treatment with prednisone 60 mg daily, azathioprine 150 mg daily, and pyridostigmine bromide 60 mg tid. Two weeks later, the patient presents to the ER department with nausea, vomiting, abdominal pain, erythematous truncal rash, and a fever of 39 degrees C. What is the most likely cause for the new symptoms? A. Azathioprine reaction B. Pyridostigmine toxicity C. Appendicitis precipitated by recent immune suppression D. Aspiration pneumonia E. Exacerbation of coexisting ulcerative