pubdoc_3_24732_473
advertisement

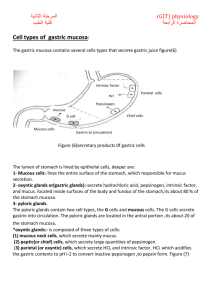
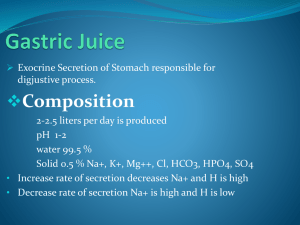
المرحلة الثانية كلية الطب ) GIT) physiology المحاضرة الرابعة Stimulation of HCL secretion: 1- Acetylcholine: Stimulation of gastric mucosa by distension. tactile stimulation or chemical stimulation include amino acid can cause two types of reflexes. ˲a- Long reflex: stomach mucosa…… through vagus nerve ….to brain stem…back to enteric nervous system of stomach wall and then to parietal cell. b- Short reflex: originates locally and transmitted entirely through local enteric nervous system. The receptor is muscarinic type and mediated is acetylcholine. so parietal cell stimulated directly by Ach for release HCL. 2- Histamine: the parietal cells operate in close association with another type of cell called enterochromaffin-like cells (ECL cells), the primary function of which is to secrete histamine. ECL cells lie in the deep of the oxyntic glands and therefore release histamine in direct contact with the parietal cells of the glands.stimulated by gastrin. The rate of formation and secretion of hydrochloric acid by the parietal cells is directly related to the amount of histamine secreted by the ECL cells The most commonly used anti ulcer drug cimetidine which is histamine antagonists that block H2 receptor on parietal cell 3- Gastrine: It is released from G cell through stimulation of vagus nerve in the antrum of stomach. Gastrine is carried by circulation to stimulate parietal cell for release HCL. Inhibition of HCL :Somatostatin: secret by Delta cells (or D cells), inhibits HCL secretion by parietal cell directly and indirectly by inhibits gastrine secretion by G cell. Phases of gastric HCL secretion:divided into three; phases cephalic, gastric and intestinal. 1- Cephalic phase: 30% of total HCL secreted in response to meal. The stimuli for HCL secretion in this phase are smelling, tasting, chewing, swallowing and conditioned reflexes. stimulation of the parietal cell by vagus nerves, which release Ach (direct). And stimulation of the parietal cells by gastrin (indirect), vagus nerve release, at G cells stimulating gastrin secretion, gastrin enters the circulation and stimulate the parietal cells. 2- Gastric phase: 60% of total HCL secreted in response to meal. The stimuli are distension of the stomach causes direct stimulation of the parietal cells by vagus nerve and indirect stimulation of the parietal cells via gastrin release .presence of breakdown products of protein, amino acid and small peptides gastrin releasing peptide(GRP)to stimulate gastrin release. Alcohol and caffeine also stimulate gastric HCL secretion GRP )) 3- Intestinal phase: It is only 10% of HCI secretion. It is mediated by products of protein digestion. Peptic ulcer and gastric barrier: A peptic ulcer is an excoriated area of stomach or intestinal mucosa caused principally by the digestive action of gastric juice or upper small intestinal secretion. peptic ulceration is an imbalance between the rate of secretion of gastric juice and the degree of protection by mucous which secrete along GIT and the alkalinity Secretion of the small intestinal(bicarbonate secretion) it caused by: 1- Breakdown of the barrier in which (the Stomach is lined with highly resistant mucous cells that secrete a viscid and alkaline adherent mucous. And the adjacent epithelial cells has tight junction between the gastric barrier prevent the stomach from auto digestion and irritation by gastric secretion or by infection with a bacterium ( Helico bacteria pylori ), disrupts this barrier, as do aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs), which inhibit the production of prostaglandins and consequently decrease mucous and HCO3–secretion. The NSAIDs are widely used to combat pain and treat arthritis. 2- Prolonged excess secretion of acid:two feedback control mechanisms that neutralization of gastric juices: A- When excess acid enters the duodenum, it reflexly inhibits gastric secretion and peristalsis in the stomach, both by nervous reflexes and by hormonal feedback from the duodenum, thereby decreasing the rate of gastric emptying. B- The presence of acid in the small intestine liberates secretin from the intestinal mucosa, which then passes by way of the blood to the pancreas to promote rapid secretion of pancreatic juice. This juice also contains a high concentration of sodium bicarbonate, for neutralization of the acid . Gastric and duodenal ulcers can be given a chance to heal by inhibition of acid secretion with drugs that block the H2 histamine receptors on parietal cells or drugs that inhibit H+– K+ ATPase. Bacteria can be eradicated with antibiotics, and NSAID-induced ulcers can be treated by stopping the NSAID. peptic ulcers most frequently occur, In a few centimeters of the pylorus ,and along the lesser curvature of the antral end of the stomach or, more rarely, in the lower end of the esophagus where stomach juices frequently reflux. Gastric digestion and absorption: *Carbohydrate digestion in the stomach depend on the action of salivary amylase, which remains active until by low pH in the stomach. *Protein digestion occur in the stomach by about 10% and mediated by HCL and gastric pepsin. *Fat digestion is minimal in the stomach due to restriction of gastric lipase activity. Very little absorption of nutrients take place in stomach. The stomach is a poor absorptive area of the gastrointestinal tract because:1)( it lacks the typical villus type of absorptive membrane) 2) the tight junctions between the epithelial cells. Only a few highly lipid-soluble substances, such as alcohol and some drugs like aspirin, As well as( non-ionized triglycerides of acetic ,propionic and butyric acid can be absorbed in small quantities). Aspirin at gastric pH is non-ionized and fat soluble, after absorption, it ionizes intracellular which damaging mucosal cells. Ethanol is rapidly absorbed by a process of simple passive diffusion along concentration gradients. water moves in both direction across mucous, Water-soluble substances including Na+ , K-,glucose and amino acid are very poorly absorbed. Vomiting (emesis): The sensory signals that initiate vomiting originate mainly from the pharynx, esophagus, stomach, and upper portions of the small intestines. It is reflex coordinated by multiple distributed nuclei in the brain stem called the “vomiting center". Or by“Chemoreceptor Trigger Zone” in the Medulla for Initiation of Vomiting by Drugs or by Motion Sickness. Causes of vomiting increased pressure within skull, rotating movement of head, intense pain, tactile stimuli applied to back of the throat and excessive distention or irritation of the duodenum. provides strong stimulus for vomiting when the vomiting center is directly activated. Define It is a forceful expulsion of contents of stomach and upper intestinal tract through mouth. In the early stages antiperistalsis begins to occur often many minutes before vomiting appears. (Antiperistalsis means peristalsis up the digestive tract rather than down ward), antiperistaltic wave travels backward up the intestine at a rate of 2 to 3 cm/sec; this process can actually push a large share of the lower small intestine contents all the way back to the duodenum and stomach within 3 to 5 minutes. Vomiting is preceded by increase salivation, sweating, increased HR, pallor and feeling of nausea. Vomiting begin deep inspiration, closure of glottis, elevation of soft palate, abdominal and thoracic muscles contract. Upper small intestine contract lower esophageal sphincter relax. Event occur repeatedly without vomiting is known retching Importance of vomiting with nausea:when the vomiting center is directly activated, it causes projectile vomiting not accompanied by nausea while stimulation of chemoreceptor trigger-zone is accompanied by nausea, to remove the ingested toxic substances before they can be absorbed. Nausea importance to avoid ingestion of food containing the same toxic substances.