PP DES Phoenix Surgery Report 2014
advertisement
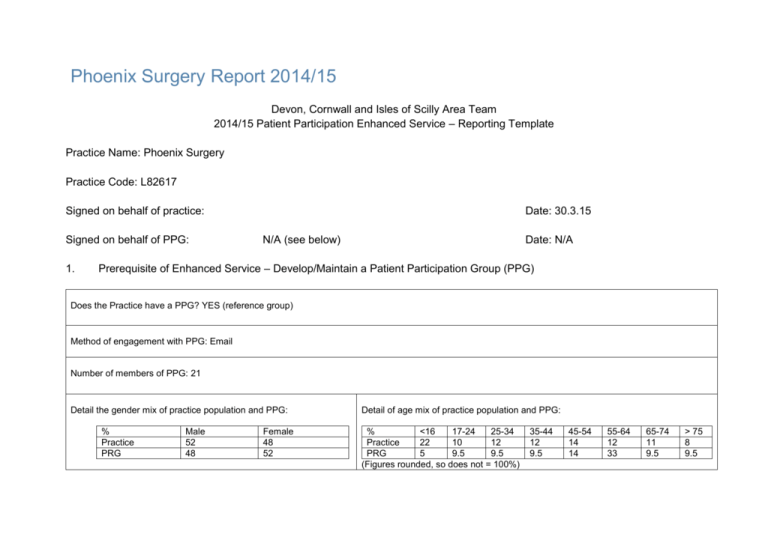
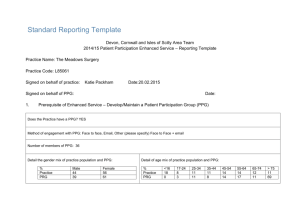
Phoenix Surgery Report 2014/15 Devon, Cornwall and Isles of Scilly Area Team 2014/15 Patient Participation Enhanced Service – Reporting Template Practice Name: Phoenix Surgery Practice Code: L82617 Signed on behalf of practice: Signed on behalf of PPG: 1. Date: 30.3.15 N/A (see below) Date: N/A Prerequisite of Enhanced Service – Develop/Maintain a Patient Participation Group (PPG) Does the Practice have a PPG? YES (reference group) Method of engagement with PPG: Email Number of members of PPG: 21 Detail the gender mix of practice population and PPG: % Practice PRG Male 52 48 Female 48 52 Detail of age mix of practice population and PPG: % <16 17-24 25-34 Practice 22 10 12 PRG 5 9.5 9.5 (Figures rounded, so does not = 100%) 35-44 12 9.5 45-54 14 14 55-64 12 33 65-74 11 9.5 > 75 8 9.5 Detail the ethnic background of your practice population and PRG: Practice PRG British Irish 28 100 0.05 0 White Gypsy or Irish traveller 0 0 Other white 7 0 White &black Caribbean 0.06 0 Mixed/ multiple ethnic groups White &black White African &Asian 0.03 0.1 0 0 Other mixed 0.08 0 PLEASE NOTE: Not all of our patients have supplied their ethnic origin; we ask for this information at registration, but it is frequently omitted Practice PRG Indian Pakistani 0.03 0 0 0 Asian/Asian British Bangladeshi 0.02 0 Chinese 0.13 0 Other Asian 0.16 0 Black/African/Caribbean/Black British African Caribbean Other Black 0.07 0 0.03 0 0 0 Arab 0 0 Other Any other 1.1 1 Describe steps taken to ensure that the PPG is representative of the practice population in terms of gender, age and ethnic background and other members of the practice population: Our PRG is advertised on our website, for which Google Translate is available for 90 languages, as well as on posters within the surgery building. We run the PRG primarily via email to avoid excluding patients who cannot attend meetings due to childcare/shift work. However, we are aware this may exclude some population groups, including those who lack technical knowledge or those without home internet access due to social deprivation. We are also aware that only 35% of over 65’s are online in Cornwall (http://www.ageuk.org.uk/PageFiles/34785/Full%20table%20for%20internet%20use%20amongst%20people%20aged%2065%20and%20over.pdf?dtrk=true). Should any individuals express an interest in the PRG who are unable to access the internet, we would aim to include them via postal or telephone surveys. As the PRG is conducted without face to face contact, this means that any individuals with conditions which they may not wish to discuss in a public forum can have their say on how their conditions are catered for by the surgery. Our advertisement specifically states that “We aim to gather people from as broad a spectrum as possible to get a truly representative sample. We need young people, workers, retirees, people with long term conditions and people from non-British ethnic groups”. Are there any specific characteristics of your practice population which means that other groups should be included in the PPG? e.g. a large student population, significant number of jobseekers, large numbers of nursing homes, or a LGBT community? YES If you have answered yes, please outline measures taken to include those specific groups and whether those measures were successful: See above RE: social deprivation 2. Review of patient feedback Outline the sources of feedback that were reviewed during the year: Patient experience survey 2013/14 (conducted March 14, results received April 14) This survey was carried out over a period of some weeks, encompassing every day of the week and a wide cross section of patients. This provided a good cross section of ages, though unfortunately there were a higher proportion of female respondents than would be representative of our practice population (64%). However, this is to be expected as women generally utilise primary care more than men (http://bmjopen.bmj.com/content/3/8/e003320.full), and this survey was carried out on patients attending the surgery during the reporting period. 87% of all patient ratings were good, very good, or excellent, with 40% being ‘excellent’. Our results placed us in the highest 25% of all means for 12 indicators, the middle 50% of all means for 16 indicators, and in the lowest 25% of all means for 1 indicator. Verbal suggestions Complaints How frequently were these reviewed with the PRG? Reviewed by annual survey 3. Action plan priority areas and implementation Priority area 1 Description of priority area: Waiting time What actions were taken to address the priority? We looked at data from our practice which showed it was often the doctor on duty that was running late as a result of squeezed in queries and phone calls, and in order to improve this for the future we have replaced 2 face-to-face appointments in the duty doctor’s clinic with 4 telephone appointment slots. This means that the duty doctor has scheduled time to take these telephone queries to avoid running late for their face-to-face patients, whilst sacrificing a minimal number of appointments to achieve this. It was also noted that patients were sometimes not informed if their clinic was running behind. Sometimes, this was a result of an unexpected delay after they had booked in, and so a sign was put up behind reception asking patients to inform reception if they experienced a wait of 30mins or more. Result of actions and impact on patients and carers (including how publicised): Patient reference group reported that they have noticed a reduction in waiting times since this was first trialled. We have publicised this via posters in the waiting room. Priority area 2 Description of priority area: Ability to speak to a practitioner on the phone What actions were taken to address the priority? See Priority area 1 – this action also contributed to addressing this. We also allowed for appointments to be booked in regular clinics as telephone consultations, as long as this was approved by the doctor in advance (to avoid consultations being booked in that may require examination). Result of actions and impact on patients and carers (including how publicised): We have publicised this via posters in the waiting room. Our receptionists sometimes offer telephone appointments with the duty doctor as an alternative to an ‘on the day’ appointment, particularly when the patient is asking for a later appointment due to work commitments, but the appointments are most commonly recommended by the doctor when requesting the patient book in for a follow up, as it is as this point it can be decided if this would be an appropriate method of review for the problem in question. There has been a good uptake of telephone appointments since these have been introduced. Priority area 3 Description of priority area: See practitioner of choice What actions were taken to address the priority? Whilst this is a priority for many patients, there are only so many patients a doctor can see in one day, and so this was a challenging area. We took the decision to offer additional sessions to our own partners before booking externally sourced locums, and aim to book the same locums consistently wherever possible. This means that our own GPs are available more often, and ensures that even if a patient’s first choice of doctor is not working that day, they can see another doctor they are likely to be more familiar with. Implementation of the duty doctor telephone consultations has also helped with this somewhat, as these consultations are shorter and so allow for more appointments during the duty session. Result of actions and impact on patients and carers (including how publicised): We have publicised this via posters in the waiting room. Our PRG reported that they have found it easier to book an appointment with a practitioner they are familiar with. This allows for better continuity of care. Progress on previous years If you have participated in this scheme for more than one year, outline progress made on issues raised in the previous year(s): Last year’s patient survey highlighted that whilst 83% of respondents were happy with the surgery environment, there were some actions we could carry out which would improve on this. These included installing a mirror in the gents toilet, new benches in the waiting room, more up to date reading material in the waiting room, and revamping the notice boards. We have since actioned two of these points. We were unfortunately unable to obtain permission from our landlord to install a mirror in the gents toilet. Due to budgetary constraints we have not yet been able to replace the benches in the waiting room, and so this action has been carried forward to next year. The noticeboards have been reorganised, including revitalising the young person’s noticeboard (and moving it to the lobby area on recommendation from EEFO), tidying the notice board behind reception, and dedicating a notice board to the care.data project. We have just released the first edition of our new quarterly patient newsletter to ensure patients have new reading material which keeps them updated on what’s going on at the surgery (and which includes an advert to say our PRG is looking for new members). We have also cleared the children’s reading corner to remove some of the older books and replaced them with new material, and cleared a number of outdated leaflets and magazines to ensure relevant material is available. 4. PPG Sign Off Report signed off by PPG: NO – group does not have a nominated spokesperson and does not meet in person. Please see above for the reasons for this. Date of sign off: N/A How has the practice engaged with the PPG: 1. How has the practice made efforts to engage with seldom heard groups in the practice population? 2. Has the practice received patient and carer feedback from a variety of sources? 3. Was the PPG involved in the agreement of priority areas and the resulting action plan? 4. How has the service offered to patients and carers improved as a result of the implementation of the action plan? 5. Do you have any other comments about the PPG or practice in relation to this area of work? 1. Please see Section 1 above regarding attempts to engage with all sectors of the population. 2. Please see Section 2 above regarding patient and carer feedback. The practice received patient and carer feedback from sources including but not limited to: - Website feedback form - Friends and family test - Annual survey - Patient satisfaction questionnaires (PSQs) - In person feedback (usually directed to practice manager, but sometimes passed on via reception staff) - Anonymous suggestions via prescriptions box - Postal comments, compliments and complaints 3. Following identification of the priority areas from our patient survey, we trialled the solutions outlined above, then consulted the PRG via a further survey, which was targeted on these priority areas. All respondents agreed that the actions outlined above should be implemented on a permanent basis. 4. Our survey revealed that we should aim to improve waiting times, ability to speak to a doctor by phone, and ability to see a doctor of the patient’s choice. As a result of the actions identified above, our PRG noted an improvement in all 3 areas. 5. N/A