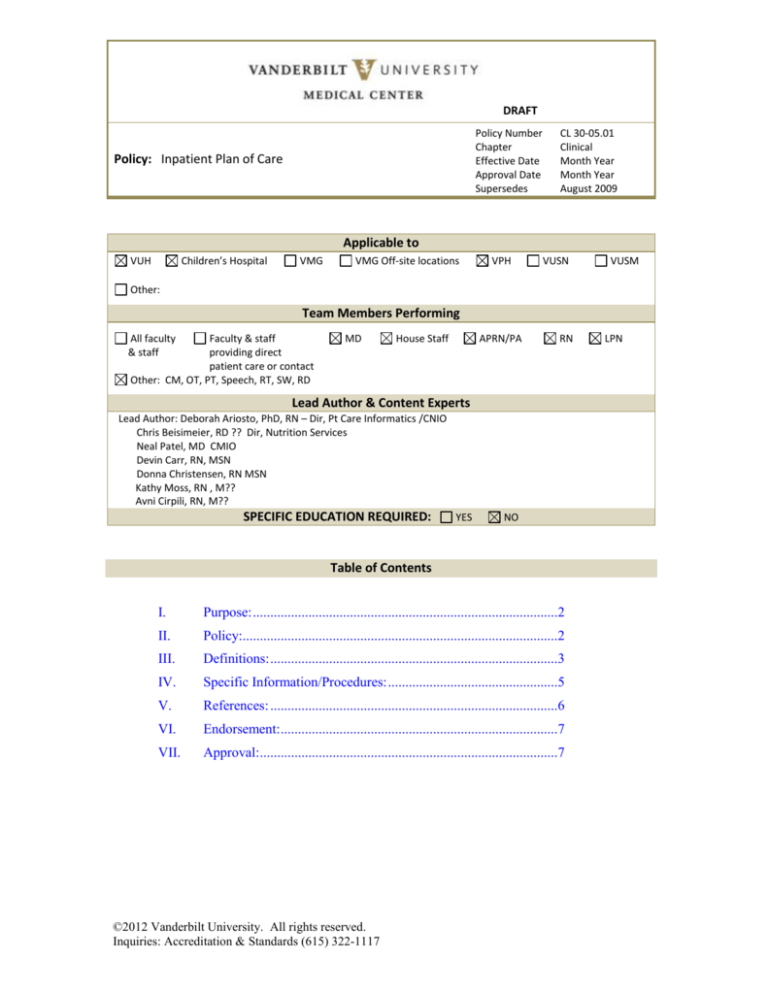
DRAFT
Policy Number
Chapter
Effective Date
Approval Date
Supersedes
Policy: Inpatient Plan of Care
CL 30-05.01
Clinical
Month Year
Month Year
August 2009
Applicable to
VUH
Children’s Hospital
VMG
VMG Off-site locations
VPH
VUSN
VUSM
Other:
Team Members Performing
All faculty
& staff
Faculty & staff
providing direct
patient care or contact
Other: CM, OT, PT, Speech, RT, SW, RD
MD
House Staff
APRN/PA
RN
Lead Author & Content Experts
Lead Author: Deborah Ariosto, PhD, RN – Dir, Pt Care Informatics /CNIO
Chris Beisimeier, RD ?? Dir, Nutrition Services
Neal Patel, MD CMIO
Devin Carr, RN, MSN
Donna Christensen, RN MSN
Kathy Moss, RN , M??
Avni Cirpili, RN, M??
SPECIFIC EDUCATION REQUIRED:
YES
NO
Table of Contents
I.
Purpose: ........................................................................................2
II.
Policy:...........................................................................................2
III.
Definitions: ...................................................................................3
IV.
Specific Information/Procedures: .................................................5
V.
References: ...................................................................................6
VI.
Endorsement: ................................................................................7
VII.
Approval:......................................................................................7
©2012 Vanderbilt University. All rights reserved.
Inquiries: Accreditation & Standards (615) 322-1117
LPN
Plan of Care
Policy Number
I.
CL 30-05.01
Purpose:
To establish guidelines for providing individualized patient care that is
multidisciplinary, consistent, coordinated, high quality, and cost effective.
To provide guidelines for initiating, customizing, and following a goal-directed
plan of care based on best practice.
To facilitate communication among multidisciplinary team members providing
patient and family-centered care.
II.
Policy:
The overview of patient care (OPC) is used to visualize the elements of the plan
of care. Each member of the care team contributes to a multidisciplinary plan of
care based on assessed patient/family needs/goals that is guided by evidence
and/or best practices. Care is initiated as clinically-indicated and documented
accordingly. The patient’s plan of care includes the following components as
applicable:
A.
Provider plan of care and individualized evidence-based orders.
B.
Nursing plan of care which includes:
1.
2.
3.
4.
5.
C.
Patient-specific priority problems
Short-term goals and measurable outcomes
Interventions to meet the goals
Nursing Summary reflecting response to care interventions
Nursing Plan Priorities changes and recommendations
Other multidisciplinary plans of care, where indicated.
1.
2.
3.
4.
5.
6.
Nutrition;
Case Management;
Social Work;
Rehabilitation (Occupational Therapy (OT), Physical Therapy
(PT), Speech Therapy (ST);
Respiratory Therapy;
Others as applicable.
Page 2 of 7
Plan of Care
Policy Number
III.
CL 30-05.01
Definitions:
A.
Patient Plan of Care - The patient’s plan of care and goals are developed
with the patient/family and reflect individualized care and treatment
provided by the multidisciplinary team.
B.
Provider Plan of Care is developed by the physician or other licensed
independent practitioner and is reflected in provider orders and progress
notes.
C.
Nursing Plan of Care
Nursing Plan of Care
Developed in conjunction with the provider plan of care and orders.
Individualized with priority problems and established goals and interventions
Nursing Priority Problems
result in
Based on the structured Clinical Care
Classification® terminology and reflect:
Patient’s priorities [pain, nutrition]
Actual or potential problems that can
be diagnosed independently by
nursing [safety, skin integrity risk]
Significant deviations from the overall
multidisciplinary team plan of care
[cardiac output, gas exchange, fluid
balance]
Nursing Priority Problem Outcomes
Reflect realistic discharge outcomes
(select one):
Improve – Support Recovery [fracture
will heal]
Stabilize – Chronic [asthma, heart failure]
Support Decline [ESRD, palliative care]
Note –when no longer a priority, these
problems are ended, with outcomes stated
(improved, stabilized, decline supported)
Priority Problem Short Term Goals are established every shift for the current shift’s Priority
Problems. Note: day and night shift may have different priorities (ambulation versus
sleep).
Plan Priorities are used to communicate the patient’s plan of care and are part of an
optimal handover when a change in caregiver occurs. It is a statement regarding
interventions that were effective, new problems, and/or recommendations for the next
caregiver (e.g., continue q4h Percocet, reinforce ambulation)
Nursing Summary is a concise, overall summary of the patient’s response to care
interventions (VSS, pain=2 on Percocet) and any significant events that occurred
Documentation Systems:
HED – Horizon Expert Documentation™ is the current inpatient nursing documentation
system in which the nursing plan is documented and then displayed in StarPanel™
(electronic health record [EHR]). This same application is used in the Peds Emergency
Department.
VPIMS is the Perioperative documentation system
WITT Cardiac Cath Lab documentation system
Page 3 of 7
Plan of Care
Policy Number
CL 30-05.01
Order Tracker is the Emergency Department (ED) order tracking system and includes some
nursing documentation.
StarForms, one of the documentation tools available in StarPanel, are used for nursing
documentation in the Adult ED.
D.
Evidence-Based Practice (EBP) – reflect validated standards of care in the
literature. EBP care guidelines are reflected in one or more of the
following resources:
1.
2.
3.
E.
VUMC evidence-based order-sets;
Published Nursing Standards of Care (Mosby’s Skills/Consult);
VUMC Clinical Pathways where appropriate for groups of like
patients by diagnosis (e.g., heart failure), procedure (e.g., cardiac
cath) or age (e.g., toddler). A list of approved pathways is
available on E-Docs. (See References.)
Nutrition Plan
1.
Nutrition Problems are identified for patients at high nutrition risk
after completion of a nutrition assessment of:
a.
b.
F.
Current intake and nutrition-related data; and
Identification of nutrition-related deficits and excesses
(e.g., protein, calories/energy, vitamins, minerals, fluid),
using comparative standards derived from evidence-based
norms and standards. Problems are identified from a list of
nutrition problems and their signs and symptoms, as
published in International Dietetics and Nutrition
Terminology (IDNT).
2.
Desired Nutrition Outcomes are developed for each nutrition
problem, and short-term goals necessary to reach desired nutrition
outcomes are identified during the initial nutrition assessment and
at each monitoring evaluation.
3.
The nutrition plan lists nutrition intervention strategies that
promote desired nutrition outcomes and short-term goals.
Nutrition intervention strategies are identified from a list of
nutrition interventions published in International Dietetics and
Nutrition Terminology (IDNT).
Additional Multidisciplinary Plans of Care (where applicable):
1.
Case Management;
Page 4 of 7
Plan of Care
Policy Number
2.
3.
4.
G.
IV.
CL 30-05.01
Social Work;
Rehabilitation (OT, PT, ST);
Respiratory Therapy.
The Overview of Patient Care (OPC) is a summary view of patient care in
StarPanel™ (EHR) with hyperlinks to additional detail, including
multidisciplinary care plans.
Specific Information/Procedures:
The inpatient interdisciplinary documentation of the plan of care is organized
through the Overview of Patient Care (OPC) in StarPanel. To initiate and update
the individualized plan of care:
A.
Review data available from the OPC (team summary, progress notes, orders, and
available results. (See References.)
B.
After considering the patient plan of care, the current patient condition and
patient’s stated goals, identify priority problems and expected outcomes
(improve, stabilize, support decline) that will be addressed this shift as part of the
multidisciplinary plan of care.
Active participation by patient and family is encouraged in developing and
revising the Plan of Care, by soliciting input regarding Priority Problems,
Patient/Family Goals, strategies to meet those goals, and by soliciting input
regarding short term goal status (met/not met) and actual outcomes (stabilized).
C.
For each priority problem, set short term goals at the beginning of the shift and
document whether they were met at the end of the shift.
1.
Evaluate the patient’s condition, the patient’s response to care and
document in the Nursing Summary at the end of the shift. Re-visit any
new information in provider and team notes and plans.
2.
Communicate your recommendations for changes in plan of care and areas
of focus through Plan Priorities.
3.
Problems that are resolved or that are no longer priorities are completed
(ended) for the patient. At discharge, post discharge plans are provided to
the patient for unresolved priority problems.
4.
The Discharge and Teaching Plans are parts of the individualized plan of
care.
Page 5 of 7
Plan of Care
Policy Number
V.
CL 30-05.01
5.
Areas using electronic documentation other than HED will make changes
to the plan of care as appropriate to the patient’s specific conditions using
the software’s edit functions. Such plans of care are uploaded to Star Panel
after the episode of care.
6.
Areas not documenting electronically: Each caregiver documenting on a
paper plan of care or pathway signs name and initials once at the bottom
of each page of the document. Changes made to the document to reflect
the patient’s specific conditions should be dated, timed and initialed by the
person making the change.
References:
Patient Care E-Docs. Retrieved January 25, 2012, from
http://edocsprod.mc.vanderbilt.edu/EDocsList.aspx
VUMC Policy Manual. Retrieved January 24, 2012, from
http://vumcpolicies.mc.vanderbilt.edu/E-Manual/Hpolicy.nsf
Clinical Policy Manual:
CL 30-05.06 Discharge Plan
CL 30-05.09 Emergency Department Documentation Guidelines on
Admitted Patients
CL 30-05.11 Teaching Record
Centers for Medicare and Medicaid Services. Section 482.13(b). Retrieved
January 27, 2012, from http://www.cms.gov/
Clinical Care Classification System. Retrieved January 24, 2012, from
http://www.sabacare.com
The Joint Commission’s Comprehensive Accreditation Manual for Hospitals
(CAMH). Retrieved online October 10, 2011, via Eskind Digital Library (search
word “CAMH”, then select “Accreditation Requirements”)
http://www.mc.vanderbilt.edu/diglib/
Provision of Care Standards: PC.01.03.01; PC.02.01.01
[add reference to link to document containing screenshots for help with
documentation]
Page 6 of 7
Plan of Care
Policy Number
VI.
VII.
CL 30-05.01
Endorsement:
Children’s Clinical Policy and Practice Committee
Date
Clinical Practice Committee
Date
Susan Hernandez BSN, MBA
Chief Nursing Officer
Associate Hospital Director – Patient Care Services
Monroe Carell Jr. Children’s Hospital at Vanderbilt
Date
Pam Jones MSN, RN
Chief Nursing Officer
Vanderbilt University Hospital
Date
Approval:
Marilyn Dubree RN, MSN, NE-BC
Executive Chief Nursing Officer
Date
C. Wright Pinson MBA, MD
Deputy Vice Chancellor for Health Affairs
CEO of the Hospitals and Clinics for VUMC
Date
Page 7 of 7