final1-mc-publishable-summary
advertisement
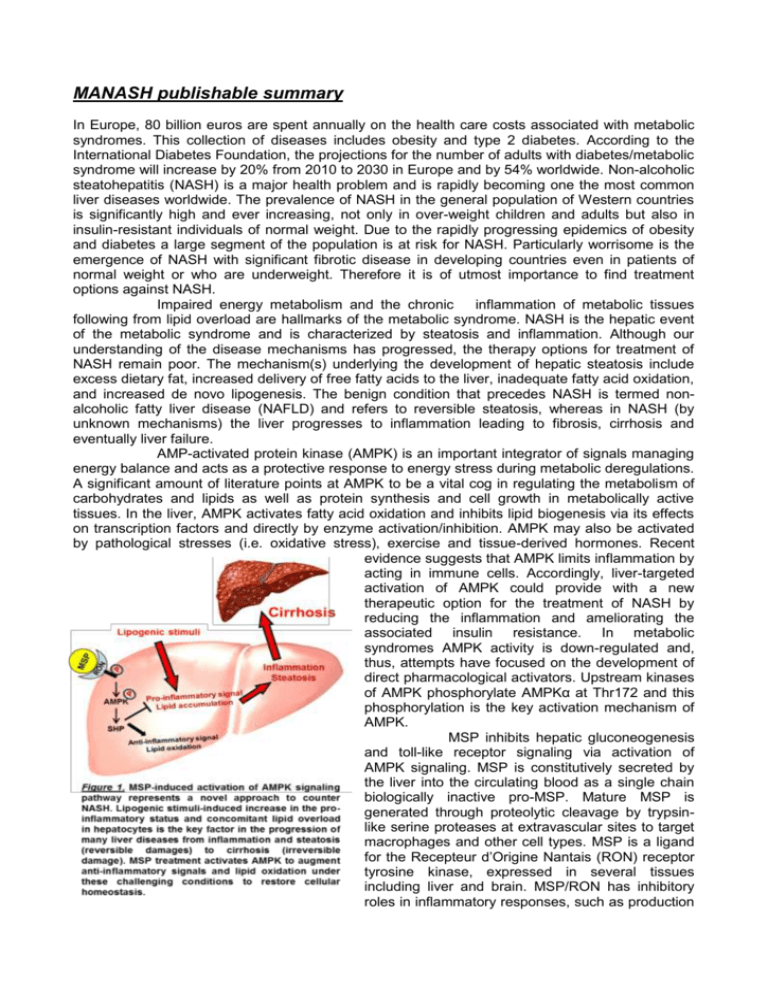
MANASH publishable summary In Europe, 80 billion euros are spent annually on the health care costs associated with metabolic syndromes. This collection of diseases includes obesity and type 2 diabetes. According to the International Diabetes Foundation, the projections for the number of adults with diabetes/metabolic syndrome will increase by 20% from 2010 to 2030 in Europe and by 54% worldwide. Non-alcoholic steatohepatitis (NASH) is a major health problem and is rapidly becoming one the most common liver diseases worldwide. The prevalence of NASH in the general population of Western countries is significantly high and ever increasing, not only in over-weight children and adults but also in insulin-resistant individuals of normal weight. Due to the rapidly progressing epidemics of obesity and diabetes a large segment of the population is at risk for NASH. Particularly worrisome is the emergence of NASH with significant fibrotic disease in developing countries even in patients of normal weight or who are underweight. Therefore it is of utmost importance to find treatment options against NASH. Impaired energy metabolism and the chronic inflammation of metabolic tissues following from lipid overload are hallmarks of the metabolic syndrome. NASH is the hepatic event of the metabolic syndrome and is characterized by steatosis and inflammation. Although our understanding of the disease mechanisms has progressed, the therapy options for treatment of NASH remain poor. The mechanism(s) underlying the development of hepatic steatosis include excess dietary fat, increased delivery of free fatty acids to the liver, inadequate fatty acid oxidation, and increased de novo lipogenesis. The benign condition that precedes NASH is termed nonalcoholic fatty liver disease (NAFLD) and refers to reversible steatosis, whereas in NASH (by unknown mechanisms) the liver progresses to inflammation leading to fibrosis, cirrhosis and eventually liver failure. AMP-activated protein kinase (AMPK) is an important integrator of signals managing energy balance and acts as a protective response to energy stress during metabolic deregulations. A significant amount of literature points at AMPK to be a vital cog in regulating the metabolism of carbohydrates and lipids as well as protein synthesis and cell growth in metabolically active tissues. In the liver, AMPK activates fatty acid oxidation and inhibits lipid biogenesis via its effects on transcription factors and directly by enzyme activation/inhibition. AMPK may also be activated by pathological stresses (i.e. oxidative stress), exercise and tissue-derived hormones. Recent evidence suggests that AMPK limits inflammation by acting in immune cells. Accordingly, liver-targeted activation of AMPK could provide with a new therapeutic option for the treatment of NASH by reducing the inflammation and ameliorating the associated insulin resistance. In metabolic syndromes AMPK activity is down-regulated and, thus, attempts have focused on the development of direct pharmacological activators. Upstream kinases of AMPK phosphorylate AMPKα at Thr172 and this phosphorylation is the key activation mechanism of AMPK. MSP inhibits hepatic gluconeogenesis and toll-like receptor signaling via activation of AMPK signaling. MSP is constitutively secreted by the liver into the circulating blood as a single chain biologically inactive pro-MSP. Mature MSP is generated through proteolytic cleavage by trypsinlike serine proteases at extravascular sites to target macrophages and other cell types. MSP is a ligand for the Recepteur d’Origine Nantais (RON) receptor tyrosine kinase, expressed in several tissues including liver and brain. MSP/RON has inhibitory roles in inflammatory responses, such as production of nitric oxide in stimulated macrophages. Downstream of RON, phosphoinositide-3-kinase (PI3K)/Akt, mitogen activated protein kinase (MAPK), β-catenin and others have been suggested to mediate the effect. However, an obvious link to explain AMPK activation is missing at present. Remarkably, on normal diet MSP-deficient mice develop steatosis. Furthermore, MSP is both necessary and sufficient to induce macrophage polarization into the anti-inflammatory M2 phenotype (opposed to the pro-inflammatory M1 activation), which assists in attenuation of inflammation. The possible implication of the MSP/RON-AMPK axis in NASH has not been investigated before. Therefore, we elucidated and evaluated MSP/RON-mediated activation of AMPK in the context of NASH (Figure 1). The main objectives of this study were (1) to investigate the molecular mechanism of MSP-mediated AMPK activation and (2) to assess the potential of MSP for ameliorating NASH. The results obtained clearly show the beneficial effects of MSP in the context of NASH-inducing conditions in vitro and ex vivo. In primary hepatocytes, MSP treatment leads to significant activation of AMPK signaling pathway. This activation is sustained even in the presence of lipogenic as well as inflammatory stimuli. Concomitantly, we observe that lipogenic/inflammatory stimulus-induced expression of several pro-inflammatory cytokine genes was significantly reduced upon MSP treatment. To confirm this observation, we analysed pro- and anti-inflammatory cytokine production level under these conditions. Our results demonstrate that MSP reduces production of pro-inflammatory cytokine and elevates anti-inflammatory production level in this set-up. Additionally, MSP reduces lipogenic stimulus-induced lipid accumulation in these cells. Furthermore, MSP treatment of bone marrow derived macrophages (BMDMs), which were exposed to NASH-mimicking stimuli, led to significant reduction in pro-inflammatory genes expression. These results strongly support the anti-inflammatory role of MSP and indicate a potential beneficial effect of MSP in treating NASH. Knockdown of RON receptor expression in human hepatic HepG2 cell line dramatically reduced the effect of MSP as was evidenced by a significant decrease in AMPK activation. After knockdown of RON, MSP failed to inhibit the free fatty acid-induced increase in pro-inflammatory genes expression under this condition. These results clearly demonstrate that an intact MSP/RON-AMPK axis is required to counter NASH. In conclusion, MSP has been verified as a potential treatment strategy against NASH. However, further analysis of in vivo data and long-term studies will be required to substantiate the efficacy and safety of MSP in mice and other experimental models. In long-term we foresee clinical testing of recombinant MSP for amelioration of human NASH. Given the severity and rising incidence of NASH, identifying potential ways of ameliorating the disease directly correlates to the well being of the society from the economical (keeping in mind the rising costs of healthcare in Europe) till the humanitarian point of view.