Lec 02: Hypersensitivity and Allergic History, Physical Examination
advertisement

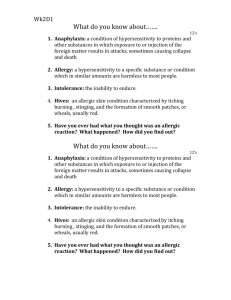
OS 216: Hematopoiesis and the Immune Response Lec 02: Hypersensitivity and Allergic History, Physical Examination and Diagnostics Dr. Cherie Ocampo-Cervantes 1 November 20, 2013 TOPIC OUTLINE I. II. III. IV. V. VI. The Four Types of Hypersensitivity Reactions Type I: Immediate Hypersensitivity Type II: Antibody-Mediated Hypersensitivity Type III: Immune Complex-Mediated Hypersensitivity Type IV: Delayed Hypersensitivity Allergic History and Physical Examination A. History B. Physical Examination Legends: From the Powerpoint presentation From the lecturer and from other sources (textbook, Internet, etc.) I. THE FOUR TYPES OF HYPERSENSITIVITY REACTIONS A. INTRODUCTION Figure 1. Types of Immune Responses Autoimmunity – failure of normal mechanisms or self-tolerance resulting to reactions against one’s cell or tissues Reaction Against Microbes – may cause disease if the reaction is excessive or if they are persistent Reaction Against Environmental Antigens – about 20% of the population are abnormally responsive to environmental antigens ALLERGENS Antigens that elicit immediate hypersensitivity Usually common environmental proteins and chemicals (e.g. food, animal hair, dust mites, pollens, certain medication) II. TYPE 1: IMMEDIATE HYPERSENSITIVITY IgE-mediated a rapid immunologic reaction occurring within minutes after the combination of an antigen with antibody bound to mast cells in individuals previously sensitized to the antigen may occur as a systemic disorder or as a local reaction The development of immediate hypersensitivity reactions is dependent on the coordinated actions of a variety of chemotactic, vasoactive, and spasmogenic compounds Figure 2. Sequence of Events in Immediate Hypersensitivity Immediate hypersensitivity reactions are initiated by the introduction of an allergen, which stimulates TH2 responses and IgE production in genetically susceptible individuals. IgE binds to Fc receptors (FcεRI) on mast cells, and subsequent exposure to the allergen activates the mast cells to secrete the mediators that are responsible for the pathologic manifestations of immediate hypersensitivity. (Release of cytokines by the mediators would result to late phase reaction which happen 2-4hours after repeated exposure to the allergen) (sorry di maedit ung pictue box na late phase) Sequence of Events in Immediate Hypersensitivity Upon first exposure to an allergen, TH2 cells are activated stimulating the B cells to produce IgE antibodies IgE binds to Fc receptors (FcεRI) on mast cells Upon subsequent exposure to an allergen, the allergen crosslinks to IgE receptors on mast cells leading to its activation The activated mast cell releases the mediators (vasoactive amines and lipid mediators) which leads to immediate hypersensitivity after repeated exposure Sensitization Occurs when a specific IgE antibody produced against the allergen binds to the mast cell Figure 3. Biological Effects of Mediators of Type 1 Hypersensitivity Lorvin, Roms, Deni Page 1 / 6 Lec 02: Hypersensitivity and Allergic History, Physical Examination and Diagnostics A. The Immediate and Late Phase Reactions (from Robbins, 2016) Immediate or Initial Reaction Wheal and flare reactions Vasodilation, vascular leakage, and depending on the location, smooth muscle spasm or glandular secretions. Changes usually become evident within 5 to 30 minutes after exposure to an allergen and tend to subside in 60 minutes. Late Phase Reaction Mainly inflammation and edema Occurs in allergic rhinitis and bronchial sets in 2 to 24 hours later without additional exposure to antigen and may last for several days infiltration of tissues with eosinophils, neutrophils, basophils, monocytes, and CD4+ T cells as well as tissue destruction, typically in the form of mucosal epithelial cell damage B. IMMEDIATE HYPERSENSITIVITY DISEASES 1. Anaphylaxis A life threatening response of a sensitized human that appears within minutes after administration of a specific antigen Manifestations of anaphylaxis include the following: o Wheals o Respiratory Involvement Laryngeal edema with or without bronchospasm Bronchial asthma (BA): predisposed to severe lower airway involvement Difficulty in breathing due to airway constriction o Cardiovascular Lowered blood pressure Cardiac malfunction tachycardia o Gastrointestinal Diarrhea Abdominal pain and vomiting 2. Allergic Rhinitis 3. Atopic Dermatitis (early phase) 4. Bronchial Asthma 5. Urticaria C. DIAGNOSTIC TESTS Anaphylaxis Diagnosis is clinical Laboratory tests are NOT specific for anaphylaxis Histamine o Onset Total tryptase o Obtain blood sample within 15min to 30hours of symptom onset Allergy Tests Adjuncts to thorough exposure history that indicates the presence of relevant IgE-mediated symptoms or signs and the physical exam In Vivo Allergy Skin Test Most sensitive Most cost-effective Based on mast cell degranulation due to the patient’s skin’s being exposed to specific allergens Wheals and flare reaction OS 213 o Food allergy o Drug allergy o insect sting hypersensitivity In Vivo Testing of Total Serum IgE identify persons with high likelihood of atopy should not be used as a diagnostic or screening test on its own measures total circulating IgE, and not amount of IgE responsible for clinical symptoms variations of levels with age considerable overlap between normal and abnormal values Antigen-Specific IgE ELISA o Quantitatively measures IgE antibodies to specific allergens Inhaled allergens Food allergens Drugs Latex Table 1. Comparative Advantage of Skin Tests VS In Vitro Tests Comparative Advantage Skin Tests In Vitro Tests high sensitivity Inhaled allergens results available in Food allergen minutes no risk of anaphylaxis greater selection of medications do not effect results allergen (not necessary to withhold cheaper than in vitro tests antihistamine, unlike in skin test) minimal equipment not dependent on skin condition needed convenient for patient afraid of needles perceived by patients as more scientific D. TREATMENT Antihistamines – against biologic amines Bronchodilators (B2 agonist) – for bronchoconstriction Steroids (topical, inhaled, intranasal, oral)– addresses inflammation Epinephrine IM – drug of choice for anaphylaxis (IMPORTANT) o 0.01mg/kg of a 1mg/mL (1:1000) aqueous dilution o Adults: 0.5mg maximum o Children: 0.3mg maximum the E. MANAGEMENT Allergen avoidance F. IMMUNOTHERAPY OR DESENSITIZATION For IgE-mediated reactions Administration of increasing doses of the allergen to induce a shift from TH2 to TH1 III. TYPE II: ANTIBODY-MEDIATED (Hypersensitivity) Hypersensitivity reaction produced by antibodies that react with antigens present on cell surfaces or in the extracellular matrix Antigenic determinants may be intrinsic to the cell membrane or matrix or an exogenous antigen (i.e. drug metabolite) Results from the binding of antibodies to normal or altered cell surface antigens A. ANTIBODY-MEDIATED DISEASES Produce by antibodies that bind to antigens in particular cells or extracellular tissues Often not systemic Usually autoantibodies o May occasionally be produced against a foreign antigen that is immunologically cross-reactive with a component of self tissues Figure 4. Skin Allergy Tests In Vivo Allergy Skin Test Indications Documentation of allergic sensitivity to specific allergens in patients with: o Asthma o Rhinitis o Eczema o Urticaria Lorvin, Roms, Deni Page 2 / 6 Lec 02: Hypersensitivity and Allergic History, Physical Examination and Diagnostics OS 213 Figure 8. Abnormal Physiologic Responses w/o cell/tissue Injury (Left) Grave’s Disease- antibodies against the thyroid-stimulating hormone receptor on thyroid epithelial cells stimulate the cells, resulting in hyperthyroidism. antibodies overstimulate receptors and cause excessive production of TSH (Right) Myasthenia gravis- antibodies reactive with acetylcholine receptors in the motor end plates of the skeletal muscles block neuromuscular transmission and therefore cause muscle weakness. Antibodies inhibit binding of acetylcholine receptors, causing myasthenia gravis. Autoimmune urticaria- positive to IgG antibodies against these possible self-antigens: o IgG o Alpha subunit of the high affinity IgE o complex formed by anti-IgE Leads to degranulation of mast cell and the resultant release of histamine, Test using the plasma-serum skin test. Figure 5. Antibody-Mediated Diseases. The antibodies can bind to tissue antigens and the deposited antibodies can induce inflammation leading to tissue injury. B. 3 MECHANISMS OF ANTIBODY-MEDIATED DISEASES OPSONIZATION AND PHAGOCYTOSIS IgG or complement fragments are attached to cell surfaces, making the cell more attractive to phagocytes, thus increasing the efficiency of phagocytosis and eventually the cell is engulfed Autoimmune Hemolytic Anemia Autoimmune Thrombocytopenic Purpura- individuals produce antibodies against their own blood cell which are then destroyed Hemolysis in transfusion reactions- cells from an incompatible donor react with and are opsonized by preformed antibodies in the host 2015: Opsonins are molecules that target antigens for an immune response (e.g. antibodies like IgG and IgM, components of complementary system C3b, C4b, mannose-binding lectin). Opsonization is the process by which bacteria are altered by opsonins so as to become efficiently engulfed by phagocytes Figure 9. Autoimmune urticaria. The patient’s serum and plasma are injected intradermally to the patient’s skin. IV. TYPE III: IMMUNE COMPLEX MEDIATED Figure 6. Opsonization and Phagocytosis. COMPLEMENT AND Fc RECEPTOR-MEDIATED INFLAMMATION Antibodies that are deposited in the tissues recruit neutrophils and macrophages, which bind to antibodies Neutrophils are activated and their products induce acute inflammation and tissue injury Example: Antibody-mediated Glomerulonephritis (also known as Goodpasture Syndrome) Figure 7. Complement Fc Receptor Mediated Inflammation. ABNORMAL PHYSIOLOGIC CELL/TISSUE INJURY RESPONSES WITHOUT Antigen-antibody complexes produce tissue damage mainly by eliciting inflammation at the sites of deposition. Can be systemic or localized to particular organs. The disease-causing immune complexes may be composed of antibodies bound to either self-antigens or foreign antigens, PHYSIOLOGY Antigens injected to the patient put him in the zone of antigen excess As the patient starts to develop antibodies against that antigen, antigen-antibody complexes are formed, which is the zone of equivalence Later in the immune response, antibody production surpasses antigen concentration, which leads to the zone of antibody excess Antibodies formed at the zone of equivalence are large and insoluble. These are readily taken up by phagocytosis of cells and are therefore eliminated by phagocytes. PATHOLOGY The pathology occurs when the antigen continues to be present in high quantities. the antigen-antibodies complexes are still formed but they become slightly more soluble and less likely to be taken uo by the phagocytes. they can trigger inflammatory complexes and lead to increased vascular permeability and deposition of immune complexes on tissues, the pathologic sequel of tissue damage occurs. Antigen-antibody complexes cause disease when: o produced in excessive amounts o not efficiently cleared o deposited in tissues This can be clinically present as vasculitis, which can occur in skin and joints. Glomerulonephritis can also occur. LOCAL IMMUNE COMPLEX DISEASE 1. Arthus Reaction Induced by injecting an antigen subcutaneously into a previously immunized animal Localized form of experimental immune complex mediated vasculitis Lorvin, Roms, Deni Page 3 / 6 Lec 02: Hypersensitivity and Allergic History, Physical Examination and Diagnostics OS 213 A. TYPE IVA Figure 10. Arthus Reaction. The deposition of immune complezes in local tissues causes a local inflammatory response known as an Arthus reaction (Janeway). B. TYPE IVB 2. Pneumonitis caused by Hypersensitivity SYSTEMIC IMMUNE COMPLEX DISEASE Acute Serum Sickness SLE Post-streptococcal glomerulonephritis Vasculitis- polyarteritis nodosa in chronic hepatitis NEWER TREATMENT MODALITIES Most important: Remove the offending agent Anti-inflammatory agents (steroids, NSAIDS)- for serum sickness Monoclonal anti-C5 antibody Rituximab (anti-CD20 antibody) for antibody suppression)- depletes B cells Intravenous immunoglobulin (IVIG)- competes with FCyR in blocking platelet destruction in idiopathic thrombocytopenic Also called cell-mediated hypersensitivity Four general subtypes: Types IVA, IVB, IVC, and IVD based on T cell subpopulation involved T lymphocytes respond against an antigen and usually induce a chronic inflammatory reaction o These cells, sensitized after contact with a specific antigen, are activated by reexposure to the antigen; they damage tissue by direct toxic effects or through release of cytokines, which activate eosinophils, monocytes and macrophages, neutrophils, or killer cells depending on type. o NOTE: For each subtype, take note of the highlighted cell and chemical mediators and also the disorders involving these reactions Type 2 helper T cell (Th2) and eosinophil-mediated immune response TH2-type T cells, upon presentation of antigens, secrete cytokines (IL-4, IL-13 and IL-5) which promote B cell IgE and IgG4 production, deactivate macrophages and cause activation of mast cells and eosinophils High production of cytokines leads to chronic inflammation, which eventually leads to tissue injury and fibrosis Examples: o chronic allergic rhinitis o chronic asthma o chronic atopic dermatitis o maculopapular exanthema with eosinophilia C. TYPE IVC V. TYPE IV: DELAYED-TYPE HYPERSENSITIVITY (DTH) Type 1 helper T cell (Th1) and monocyte-mediated immune reactions Soluble protein antigens processed by macrophages and dendritic cells, which are then presented to TH1 lymphocytes TH1 lymphocytes, after multiplying and migrating to the dermis, in return, will release interferon-γ, TNF-β and IL-2 (proinflammatory cytokines) Interferon-γ from TH1 cells will activate surrounding macrophages, which will then release prostaglandins, leukotrienes, ROS, NO, cytokines and chemokines – inflammatory response Examples: o tuberculin tests o contact dermatitis to rubber slippers Cytotoxic CD8+ T cell mediated with cytokines perforin, granzyme B, and Fas ligand Examples: o Contact dermatitis o Steven-Johnson Syndrome (bullous reaction) and Toxic Epidermal Necrolysis o Most drug-induced delayed hypersensitivity reactions o Macropapular and bullous exanthems D. TYPE IVD CD4+ and CD8+ T cell and neutrophil-mediated with cytokines IL8 and GM-CSF TH17 T-cells act as effector cells Emigrate to tissues and can kill tissue cells (ex. hepatocytes, keratinocytes) TH17 cells release IL-17, which then induce cytokine production in other surrounding cell types (ex. fibroblasts) and neutrophil migration Examples: o Psoriasis o Behcet’s disease o Acute generalized exanthematous pustulosis (AGEP) E. DIAGNOSTICS FOR TYPE IV HYPERSENSITIVITY PATCH TESTING Measure of delayed hypersensitivity reaction Artificially attempts to reproduce the clinical symptoms of the patient Helps to determine provocative antigens Sensitivity and specificity of 70% VI. ALLERGIC HISTORY AND PHYSICAL EXAMINATION A. HISTORY Figure 11 . DTH Subtypes. Please refer to this figure as you go through DTH. This concisely covers the four DTH subtypes. But if you want more details (higher learning!), please see the low quality pictures in the handout in UVLE. Lorvin, Roms, Deni Single most important in diagnosing allergic disorders Focused allergic history consists of: o Symptoms o Alleviating/exacerbating factors o Family History o Environmental History o Psychosocial Issues (stress may aggravate allergies) SYMPTOMS Age of onset Duration of illness Time of occurrence (morning, afternoon, evening, dawn) o Urticaria usually occurs in the afternoon or evening o Nocturnal cough in asthma Pattern of occurrence (perennial, episodic, seasonal) Page 4 / 6 Lec 02: Hypersensitivity and Allergic History, Physical Examination and Diagnostics o Episodic – dust mite or cockroach o Seasonal - pollens Ocular Symptoms (can be a accompanied by allergic conjunctivitis) Pruritus Photophobia Lacrimation Angioedema (e.g. NSAID allergy) Congestion Throat Symptoms Throat pruritus Post-nasal drip Cough Palatal Itch Throat clearing Soreness Hoarseness Lung Symptoms Dyspnea Chest tightness Wheezing Expectoration Gurgly chest (halak) Ear Symptoms Pruritus Angioedema Discharge Fullness Otitis media (complication of allergic rhinitis) Nasal Symptoms Sneezing Pruritus Rhinorrhea Congestion Sniffing Anosmia Skin Symptoms Pruritus Wheal Macule/patch Papule/plaque Vesicle/bulla Hyper- or hypopigmentation PRECIPITATING/EXACERBATING FACTORS Dust Strong odors o Exhaust fumes o Perfumes o Cigarette smoke Changes in temperature Changes in weather Sweat Bath – hot or cold Exercise Respiratory infections Emotions Stress Hormonal changes o Pregnancy o Menstruation/menopause Food Medications ASSOCIATED SYMPTOMS Headache Paranasal pain Maxillary fullness Nausea Vomiting OS 213 Dizziness Abdominal pain Joint pain (may indicate an autoimmune disease) Orthopnea Jaundice (can be due to drug allergy) PAST MEDICAL HISTORY Previous consults, work-up, surgeries and procedures Previous and current medications, dose, and frequency, duration and response to treatment Other medical problems FAMILY MEDICAL HISTORY Allergies have a strong hereditary link One parent: 40% risk Both parents: 60-80% risk ENVIRONMENTAL HISTORY Manner of cleaning (broom, moist rag, vacuum cleaner) Dust-collecting fixtures (curtains, drapes, carpet, books, clothing, stuffed toys, screens, upholstery) Beddings o Pillow material (kapok, down feathers, cotton, foam) o Blanket material (Wool, cotton, flannel) Ventilation (air conditioning, electric fan, open windows) and humidity (damp, dry or dusty) Presence of pests/pets Yard and vicinity (trees, vacant lots, busy streets, factory fumes and smoke) School or workplace (dusty books or papers, chemical fumes, chalk dust, ventilation and humidity) Activities (indoor deskwork, field work, manual labor, prolonged sun exposure, sports and exercise) Psychosocial issues – stress may aggravate allergies B. PHYSICAL EXAMINATION ANTHROPOMETRICS AND VITAL SIGNS Weight and height Stunting or muscle wasting Vital signs: BP, HR, RR, temperature HAIR AND SCALP Alopecia Cradle cap - infantile or neonatal seborrhoeic dermatitis Figure 12 . The Atopic March. It refers to natural history of atopic manifestations, which is characterized by a typical sequence of immunoglobulin E (IgE) antibody responses and clinical symptoms that appear early in life, persist over years or decades, and often remit spontaneously with age. SKIN Xerosis (abnormal dryness) Keratosis pilaris (“chicken skin”) Macules, papules, nodules, and wheals Excoriations, lichenifications Mucosal involvement (i.e. Stevens-Johnson Syndrome) Pityriasis alba (dry, finescaled, pale patches on the face) Ichthyosis Patches, plaques, tumors, and urticarial Hyper– and hypopigmentation Nikolsky sign (for pemphigus vulgaris) – the epidermis detaches when you stroke the skin EYES Conjunctival injection Icteric sclerae Allergic shiners (in allergic rhinitis) Cobblestoning Tearing Dennie-Morgan fold (fold or line in the skin lower eyelid caused by edema in atopic dermatitis) below the EARS Check pinnae, ear canal, tympanic membrane Check for discharge Figure 13 . Drug allergy. The most recently introduced drug is usually the culprit. In this case, it is cotrimoxazole. Lorvin, Roms, Deni NOSE Allergic salute – the gesture of wiping of the nose in an upward movement using the palm, the back of the hand or the fingers Nasal crease – formed along the border between the cartilaginous and bony parts of the nasal bridge, due to the constant wiping of the nose, especially when the patient has a habit of doing the allergic salute Page 5 / 6 Lec 02: Hypersensitivity and Allergic History, Physical Examination and Diagnostics Bunny red nose Alar flaring NASAL TURBINATES Pink/pale Congested Boggy Polypoid Check if the left, right, or both turbinates have the same characteristics NASAL DISCHARGE Check whether it is watery, mucoid, purulent, or bloody THROAT Cobblestoning (in chronic post-nasal drip) Hyperemia Tonsillar hypertrophy Post-nasal drip ORAL CAVITY Cheilitis – inflammation of the lips NECK AND THYROID Thyromegaly (thyroiditis from urticaria) CHEST AND LUNGS Use of accessory muscles Breath sounds (decreased, hyperresonant) Adventitious sounds (rales, wheezing, rhonchi) APPENDIX A: TYPES OF HYPERSENSITIVITY REACTIONS OS 213 HEART Check for presence of irregular rhythms or murmurs ABDOMEN Check for hepatomegaly, splenomegaly, or both EXTREMITIES Palmar hyperlinearity, edema, joint swelling, dry palms OTHERS Lymphadenopathies Headlight sign o For atopic dermatitis patients, the nose is spared from the spread of itch making it appear to have lighter color than the surrounding skin END OF TRANSCRIPTION Greetings! LORVIN: Hello! ROMS: Hi! DENI: Hi! AFTG! Types 1, 2, 3 = antibody-mediated Type 4 = T-cell mediated Lorvin, Roms, Deni Page 6 / 6