Development of a Nurse Practitioner
advertisement
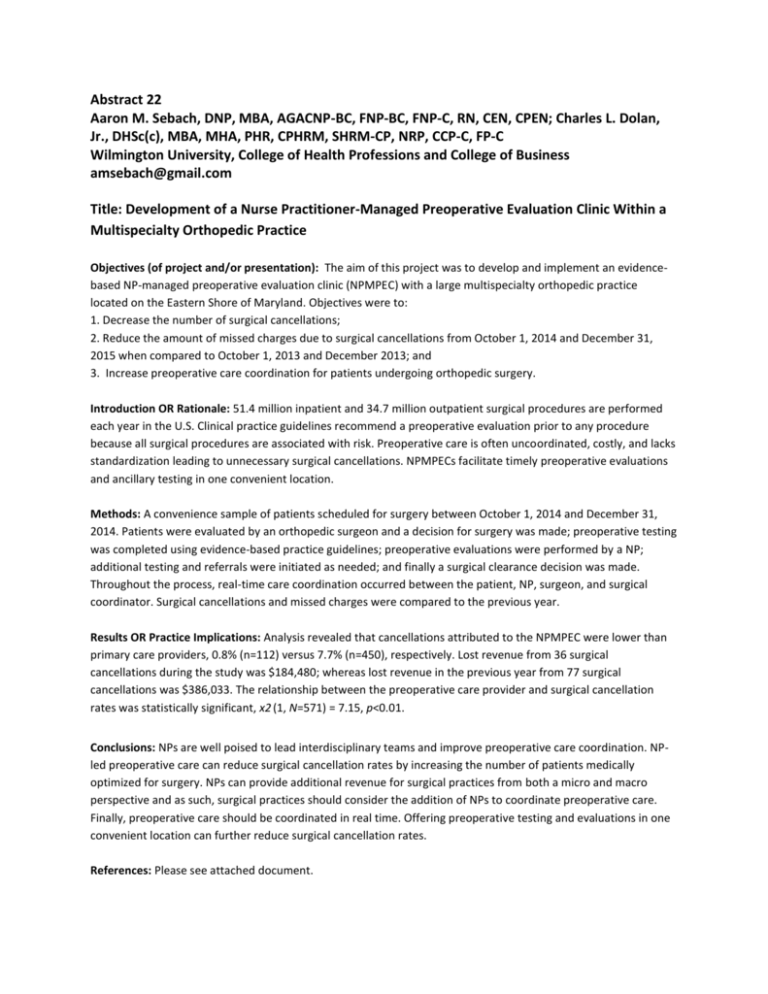
Abstract 22 Aaron M. Sebach, DNP, MBA, AGACNP-BC, FNP-BC, FNP-C, RN, CEN, CPEN; Charles L. Dolan, Jr., DHSc(c), MBA, MHA, PHR, CPHRM, SHRM-CP, NRP, CCP-C, FP-C Wilmington University, College of Health Professions and College of Business amsebach@gmail.com Title: Development of a Nurse Practitioner-Managed Preoperative Evaluation Clinic Within a Multispecialty Orthopedic Practice Objectives (of project and/or presentation): The aim of this project was to develop and implement an evidencebased NP-managed preoperative evaluation clinic (NPMPEC) with a large multispecialty orthopedic practice located on the Eastern Shore of Maryland. Objectives were to: 1. Decrease the number of surgical cancellations; 2. Reduce the amount of missed charges due to surgical cancellations from October 1, 2014 and December 31, 2015 when compared to October 1, 2013 and December 2013; and 3. Increase preoperative care coordination for patients undergoing orthopedic surgery. Introduction OR Rationale: 51.4 million inpatient and 34.7 million outpatient surgical procedures are performed each year in the U.S. Clinical practice guidelines recommend a preoperative evaluation prior to any procedure because all surgical procedures are associated with risk. Preoperative care is often uncoordinated, costly, and lacks standardization leading to unnecessary surgical cancellations. NPMPECs facilitate timely preoperative evaluations and ancillary testing in one convenient location. Methods: A convenience sample of patients scheduled for surgery between October 1, 2014 and December 31, 2014. Patients were evaluated by an orthopedic surgeon and a decision for surgery was made; preoperative testing was completed using evidence-based practice guidelines; preoperative evaluations were performed by a NP; additional testing and referrals were initiated as needed; and finally a surgical clearance decision was made. Throughout the process, real-time care coordination occurred between the patient, NP, surgeon, and surgical coordinator. Surgical cancellations and missed charges were compared to the previous year. Results OR Practice Implications: Analysis revealed that cancellations attributed to the NPMPEC were lower than primary care providers, 0.8% (n=112) versus 7.7% (n=450), respectively. Lost revenue from 36 surgical cancellations during the study was $184,480; whereas lost revenue in the previous year from 77 surgical cancellations was $386,033. The relationship between the preoperative care provider and surgical cancellation rates was statistically significant, x2 (1, N=571) = 7.15, p<0.01. Conclusions: NPs are well poised to lead interdisciplinary teams and improve preoperative care coordination. NPled preoperative care can reduce surgical cancellation rates by increasing the number of patients medically optimized for surgery. NPs can provide additional revenue for surgical practices from both a micro and macro perspective and as such, surgical practices should consider the addition of NPs to coordinate preoperative care. Finally, preoperative care should be coordinated in real time. Offering preoperative testing and evaluations in one convenient location can further reduce surgical cancellation rates. References: Please see attached document. Funding Source: None