Vaccination uptake s..
advertisement
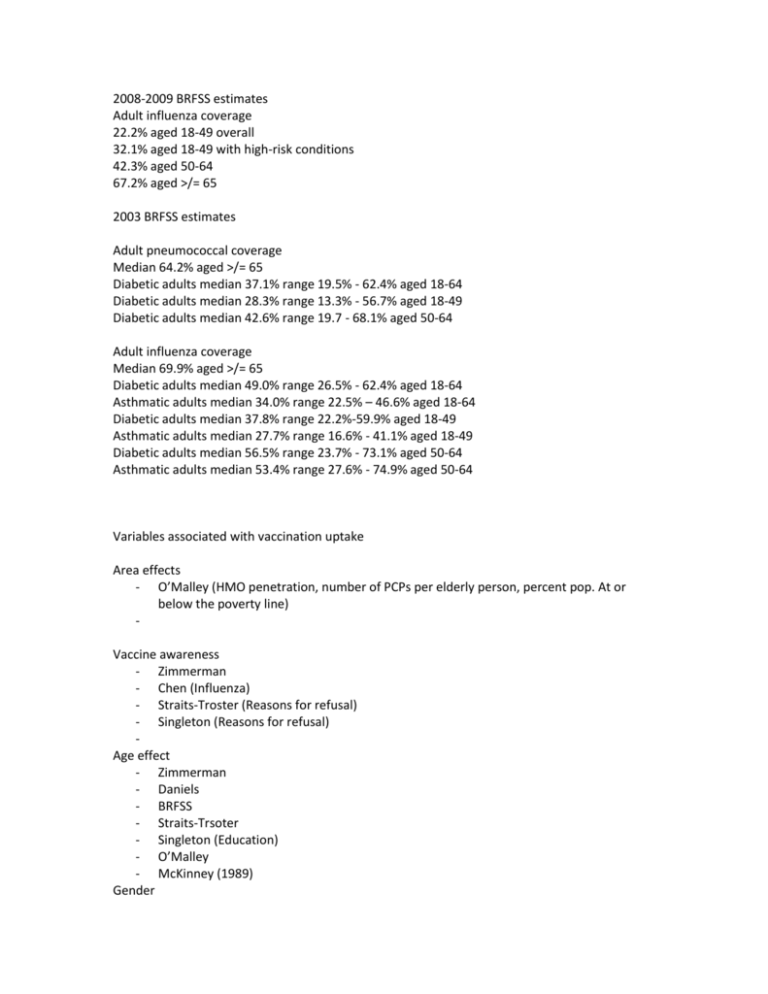
2008-2009 BRFSS estimates Adult influenza coverage 22.2% aged 18-49 overall 32.1% aged 18-49 with high-risk conditions 42.3% aged 50-64 67.2% aged >/= 65 2003 BRFSS estimates Adult pneumococcal coverage Median 64.2% aged >/= 65 Diabetic adults median 37.1% range 19.5% - 62.4% aged 18-64 Diabetic adults median 28.3% range 13.3% - 56.7% aged 18-49 Diabetic adults median 42.6% range 19.7 - 68.1% aged 50-64 Adult influenza coverage Median 69.9% aged >/= 65 Diabetic adults median 49.0% range 26.5% - 62.4% aged 18-64 Asthmatic adults median 34.0% range 22.5% – 46.6% aged 18-64 Diabetic adults median 37.8% range 22.2%-59.9% aged 18-49 Asthmatic adults median 27.7% range 16.6% - 41.1% aged 18-49 Diabetic adults median 56.5% range 23.7% - 73.1% aged 50-64 Asthmatic adults median 53.4% range 27.6% - 74.9% aged 50-64 Variables associated with vaccination uptake Area effects - O’Malley (HMO penetration, number of PCPs per elderly person, percent pop. At or below the poverty line) Vaccine awareness - Zimmerman - Chen (Influenza) - Straits-Troster (Reasons for refusal) - Singleton (Reasons for refusal) Age effect - Zimmerman - Daniels - BRFSS - Straits-Trsoter - Singleton (Education) - O’Malley - McKinney (1989) Gender - Daniels – Females more likely. (Influenza and PPV) - Straits-Troster - O’Malley - McKinney (1989) - Kamal Other Demographic - Straits Troster - Nichol? - Singleton (Education) - O’Malley (Urban/rural) - Kamal (Marriage, education, employment). Physician’s recommendation - Nichol – best because they examined an interaction effect. - Zimmerman (PPV) - Lindley - Straits-Troster (Reasons for vaccination) - Singleton – Reasons for refusal. - CDC 1988 –Nichol 1995 and CDC 1988 are often cited together Physician characteristics - O’Malley (specialty, accessibility, quality of care, continuity of care). Quality of care was measured in six unique dimensions based on factor analysis of MCBS data – only two factors (accessibility and information giving) were related to vaccination. Also physician density (primary care) positive influence on vaccination. - Zimmerman 2004 o Physician smoking status, other vaccination (Td) practices. No correlation with patient’s own vaccination behavior. - Santibanez o Physician self-report of vaccination behavior accurate o Predisposing factors (personal vaccination, sources of information, etc.) not related to PPV rates. o Environmental factors (reimbursement concern (not associated), vaccine outreferral (inversely associated)). o Satisfaction with management aspect of physician jobs (associated), stress (associated!!) - Nichol (2001) – male, generalist (PPV), physician’s own influenza vaccination status. Provides good data on prevalence of QI. Also see list of factors physicians feel are important. - Szilagyi (2005) – Rural vs urban, academic vs non-academic, group practice - Gemson – physicians treating minority patients o Physician characteristics (IMG, literature time, subscriptions, training) o Practice volume, Medicaid patients. Physician KAB - Zimmerman 2004 (Agreement helps, awareness, oddly, was counter-productive – maybe too much “awareness”) - McKinney - Nichol (2001) - Patient risk and vaccine cost-effectiveness high OR for influenza and PPV. Also see list of factors physicians feel are important. Szilagyi – Appears to support McKinneys point. Gemson – Physician attitude not found to be a factor. Educational background (No direct measurement of knowledge) explained some of the white-black gap. Other QI sorts of things - Straits-Troster (Reasons among vaccinees) - Zimmerman 2004 – Reinforcing factors, enabling factors (prevalence of QI interventions reported). Also environmental factors – access to nurse or PA helps. Also VA > inner city > rural > suburban. - Santibanez – o Enabling and environmental factors (Immunization clinics, reminder/registry systems) - Nichol (2001) – Tracking systems, CPGs (PPV only), number of vaccination QI strategies (PPV only). - Szilagyi o List of barriers perceived by physicians including practical barriers, education, concerns about vaccine. Barriers differed for influenza and PPV. o Prevalence of QI strategies o Physician practice accessibility - Zimmerman 2004 Physician reimbursement - Zimmerman 2004 – those concerned about adequate reimbursement and who would out-refer a Medicaid individual for vaccination had lower vaccination rates. - Santibanez – As above. - Nichol (2001) – See list of factors physicians feel are important, reimbursement does not rank high. - Szilagyi – Inadequate reimbursement as a physician-reported barrier. Third most common. Frequency and type of primary care visits - e.g.: Zimmerman – PPV vaccinations – more common among patients who had a complete physical examination in the past 2 years. - Nichol? - Daniels – recent checkup associated among whites. - Hebert – (Medicare claims) – access to primary care and whether vax is a primary reason for visit. Whites over 5 times more likely vs AAs to have a vaccination – initiated visit. - Straits Troster - Singleton - O’Malley - McKinney (1989) – frequency of visits and usual/new provider. - Kamal (visit in the last year vs no visit) Attitudes towards PCP - Nichol - Straits Troster - O’Malley Physician “busy-ness” - Hebert – number/$value of procedures at each visit as a metric, not found to be associated with vax though minorities have busier visits. - Zimmerman 2004 – High or low emphasis on urgencies was related to lower vaccination rates. - Santibanez – Time spent on management activities not related to patient vaccination rates. - Nichol (2001) – PPV only. Also see list of factors physicians feel are important. - Gemson – Time physician spent with each patient explained part of the white-black gap. Physician discrimination - Hebert – no evidence of physician discrimination. Whites receive more vaccinations on visits were vax was an adjunct concern, but this was not the case where the set was restricted only to those providers whites and blacks/ hispanics had in common. Minorities may frequent providers that provide fewer vaccinations. - Gemson – physicians treating minority patients – outcome = recommendation, not actual vaccination, so definitely supports Hebert’s point. Susceptibility (HBM) – disease - Nichol (Influenza and PPV) - Chen (racial strata) - Lindley - Singleton (Reasons for refusal) - Kamal (those who perceived their health as being poor) Severity (HBM) – disease - Nichol (Influenza and PPV) - Lindley - Chen (racial strata) Benefits (HBM) – intervention - Nichol (Influenza and PPV) - Chen (racial strata) - Lindley - Zimmerman (2004) – but only significant predictors in a multivariable model estimated, may be underpowered. Barriers/ fears (HBM) – intervention - Nichol (Influenza and PPV) - Chen (racial strata) - Lindley (Influenza) - Hebert - Singleton (reasons for refusal) - Szilagyi – Physician perceptions that this matters General Attitude - Lindley - Nichol (Influenza and PPV) - Hebert (From MCBS reasons for refusal of influenza vaccination) - Straits-Troster (Reasons for refusal) Previous vaccination - McKinney (1989) Race - Daniels – Showed racial disparities. Vietnamese Americans significantly different from Asian Americans. - Chen - Lindley – shows enduring race effect, evidence for mediation by attitudes but not completely explanatory. Exists also within strata of attitude and provider recommendation. - Hebert - Straits-Troster – Unaccounted mechanisms. - Singleton – This study purports to account for racial differences, noting interaction between education and race. - O’Malley – great study suggesting unaccounted mechanisms. No KAB-data among patients. - CDC 1988 - Gemson – physicians treating minority patients – outcome = recommendation, not actual vaccination, so definitely supports Hebert’s point. o Physician characteristics (IMG, literature time, subscriptions, training) o Practice volume o Vaccination practices - Kamal Chronic diseases - BRFSS - Straits-Troster (Chronic disease) Insurance / financing - Chen (latinos) - O’Malley - Kamal (household income, third party health care coverage) – notably, income effect reversed at higher incomes, but only for pts 50-65. Inconvenience / logistics / access - Chen (reasons for refusing) - Hebert (Medicare claims) Missed opportunities - Hebert - Singleton Social influences - Zimmerman 2005 - Patient factors are important in explaining racial disparities (e.g.: reasons for refusal, resistance to vaccination, presentation to medical care), but are not sufficient. Missed opportunities are huge, and Hebert suggests that they may be more important. PPV – more likely to have refused vaccinations due to non-awareness. Side effect concerns may be uncommon (Singleton). System-level characteristics – O’Malley good stuff. Problem in the literature – lack of interactions with comprehensive data. (See discussion in O’Malley, and results in Singleton). Need communications / interpersonal continuity data. Health literacy. Neighborhood. Low uptake is not purely a patient phenomenon, although patient factors contribute. Low uptake is not purely a provider phenomenon, although provider factors contribute. Low uptake is a complex, situated issue. While OR can point out causal factors, make sure you take a look at straight prevalence. E.g.: MMWR often cites Nichol et al. 1995 showing that a large proportion of physicians do not strongly recommend vaccination.