Chapter 2: Neonatal Resuscitation (ToPEM)
advertisement
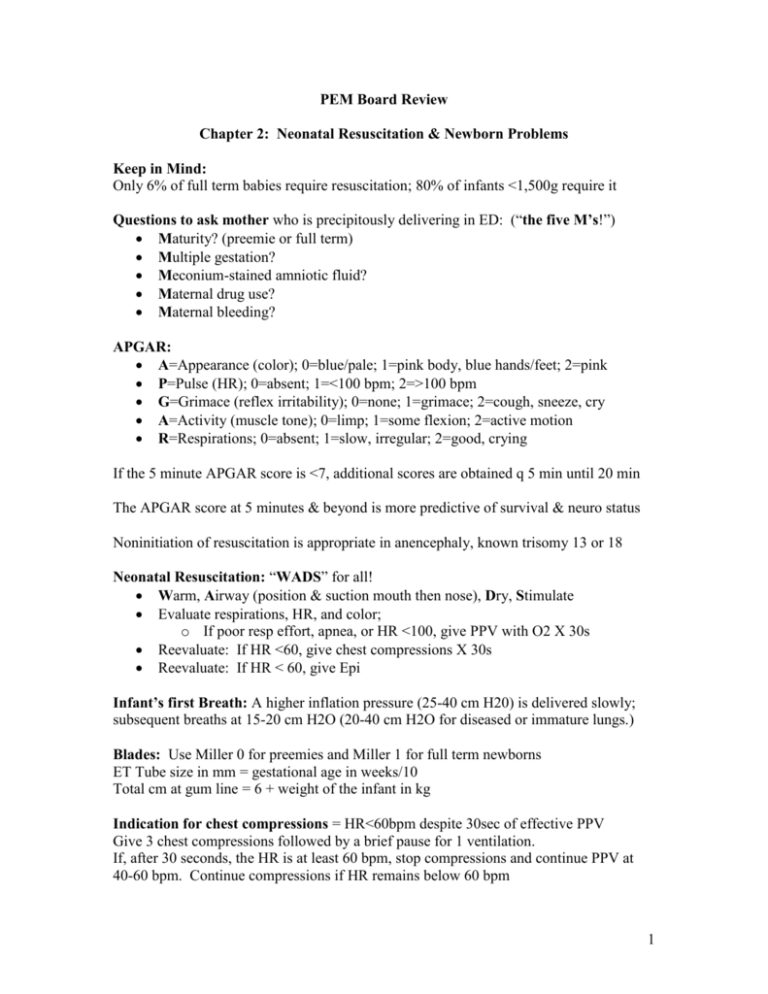
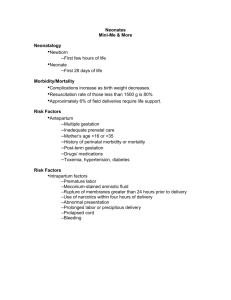
PEM Board Review Chapter 2: Neonatal Resuscitation & Newborn Problems Keep in Mind: Only 6% of full term babies require resuscitation; 80% of infants <1,500g require it Questions to ask mother who is precipitously delivering in ED: (“the five M’s!”) Maturity? (preemie or full term) Multiple gestation? Meconium-stained amniotic fluid? Maternal drug use? Maternal bleeding? APGAR: A=Appearance (color); 0=blue/pale; 1=pink body, blue hands/feet; 2=pink P=Pulse (HR); 0=absent; 1=<100 bpm; 2=>100 bpm G=Grimace (reflex irritability); 0=none; 1=grimace; 2=cough, sneeze, cry A=Activity (muscle tone); 0=limp; 1=some flexion; 2=active motion R=Respirations; 0=absent; 1=slow, irregular; 2=good, crying If the 5 minute APGAR score is <7, additional scores are obtained q 5 min until 20 min The APGAR score at 5 minutes & beyond is more predictive of survival & neuro status Noninitiation of resuscitation is appropriate in anencephaly, known trisomy 13 or 18 Neonatal Resuscitation: “WADS” for all! Warm, Airway (position & suction mouth then nose), Dry, Stimulate Evaluate respirations, HR, and color; o If poor resp effort, apnea, or HR <100, give PPV with O2 X 30s Reevaluate: If HR <60, give chest compressions X 30s Reevaluate: If HR < 60, give Epi Infant’s first Breath: A higher inflation pressure (25-40 cm H20) is delivered slowly; subsequent breaths at 15-20 cm H2O (20-40 cm H2O for diseased or immature lungs.) Blades: Use Miller 0 for preemies and Miller 1 for full term newborns ET Tube size in mm = gestational age in weeks/10 Total cm at gum line = 6 + weight of the infant in kg Indication for chest compressions = HR<60bpm despite 30sec of effective PPV Give 3 chest compressions followed by a brief pause for 1 ventilation. If, after 30 seconds, the HR is at least 60 bpm, stop compressions and continue PPV at 40-60 bpm. Continue compressions if HR remains below 60 bpm 1 NaHCO3: 1-2mEq/kg slow IVP with good ventilation; only use for documented metabolic acidosis in prolonged resuscitation or hyperkalemia. Narcan is 0.1mg/kg IVP; use in infants displaying signs of respiratory depression after PPV has restored a normal HR and color, and for infants whose mothers have received narcotics within the 4 hours prior to delivery; may need multiple doses; do NOT give to infants of mothers who are narcotic addicted. Hypoglycemia: Give D10W @ 2cc/kg IVP Meds that can be given via ETT: LEAN (Lido, Epi, Atropine, Narcan) Epi indicated: when the newborn’s HR remains < 60 bpm despite 30 s of effective PPV with 100% O2 and another 30 s of chest compressions with ventilation. If Epi via ETT, dilute with 2 ml saline; give as push every 5 minutes followed by 1 cc NS flush Volume expanders (NS, LR, PRBC): 10 cc/kg IV over 10 minutes Meconium staining of amniotic fluid complicates 10-20% of all deliveries; risk increases to 30% in infants born after 42 weeks gestation; 2% of those infants have MAS; In Meconium stained fluid birth, suction mouth, pharynx, and nose as soon as head is delivered using a 12-14F catheter or bulb suction; Then, if baby is depressed (poor respirations, depressed muscle tone, HR <100) direct suction the trachea until clear right AFTER the infant is placed in a warm environment. Once initial resuscitation is done, then insert OG tube to empty stomach contents. Pneumothorax is more common is Premature infants and in infants with MAS; signs and symptoms include grunting respirations, intercostal, sternal, and substernal retractions, increased RR and tachycardia followed by bradycardia and hypotension; may decreased breath sounds and distant heart tones (may see increased light transmission on the side of the PTX during transillumination); If PTX suspected, decompress using 20 g needle, three way stopcock, and large syringe; go into second interspace of midclavicular line. Diaphragmatic Hernia: suspect when tachypnea, asymmetric chest wall motion, and scaphoid abdomen; CXR shows bowel gas within the thorax; Promptly place NG tube to decompress the stomach and avoid excessive air in the bowel in the thorax Omphalocele is covered by a thin layer of amnion that may be intact or broken. These are associated with CV abnormalities Gastroschisis: abdominal contents are free floating in amniotic fluid. In both cases, cover the eviscerated bowel with warm saline-soaked gauze and place abdominal contents in a plastic bag for a gastroschisis (keep infant warm and dry); place an NG tube in both cases. 2 Prostaglandin E1: Short 1/2 life; therefore need continuous infusion; Intubate first due to side effect of apnea. Use with ductal dependent lesions (TGA, Coarct, TAT, etc.) presenting in shock (day 2-21); #1 side effect: apnea; #2 side effect: hypotension Newborn chest compressions: deliver on the lower third of the sternum to a depth of approximately 1/3 of the AP diameter of the chest. 120 events per minute (90 compressions and 30 breaths in a 3:1 ratio) Salt-wasting congenital adrenal hyperplasia (CAH): due to a deficiency of 21hydroxylase; therefore cortisol can’t be produced, therefore, ACTH levels high causing adrenal cortex to have hyperplasia, thus causing steroid precusors to accumulate and are metabolized to androgens (which is why females are caught with virulization in the nursery and males are more likely to present in shock to the ED at 1-2 weeks of life); Initial Lytes: Na: low, K: high, Cl: low, HCO3: low, Glucose: low. Early signs of adrenal crisis: lethargy, poor appetite, FTT, and weight loss. Treatmenet: fluid resuscitation first, correct hypoglycemia (if present), and then administer glucocorticoids. (hydrocortisone 25mg IV x1); Minealocorticoid, bicarb, and correction of hyperkalemia is rarely necessary if the above is done. ETT Sizes: Tube Size 2.5 3.0 3.5 4.0 Weight (g) <1000 1000-2000 2000-3000 >3000 GA (weeks) <28 28-34 34-38 >38 In cardiac arrest, immediate IO access (above any other access—central line, UVC, cutdown, PIV) is recommended if no other IV access is already in place Hypoglycemia in newborns: glucose concentration less than or equal to 35 within the first few hours of birth or less than or equal to 45 at 24 hours of age. Congenital cataracts: seen in galactosemia and congenital hypoparathyroidism but not other inborn errors of metabolism. Incidence of PDA increases in premature infants. PDA murmur is a continuous or “machine type” murmur in the upper left sternal border or left infraclavicular area. Signs: tachypnea, tachycardia, and CHF. Cyanotic Heart Lesions: TOGV, TAT, TAPVR, and TOF Jaundice: Jaundice within the first 24 hours of life is pathologic. Physiologic jaundice of the newborn: starts day 2-3, peaks day 5, resolves by day 14. 3 Rh disease occurs when mom is Rh-negative and baby is Rh-positive. ABO incompatibility occurs when mom is O and baby is A, B, or AB. Jaundice from biliary atresia: develops at 2 weeks of age or later. Direct Bili > 2. Infants with G6PD deficiency: at risk for nonimmune hemolytic anemia with early unconjugated hyperbilirubinemia; X-linked (affects males) Risk factors for renal vein thrombosis: dehydration, hypotension, hyperviscosity, perinatal asphyxia, and a UVC. Classic clinical triad: a flank mass, hematuria, and thrombocytopenia. Study of choice is the renal ultrasound with Doppler. You feel a palpable bladder: think lower urinary tract obstruction. Most common cause in male infants: posterior urethral valves. Immediate treatment: place a foley catheter. Polycythemia: central venous hematocrit greater than 65%. Increased risk of this in infants of diabetic mothers. Most common problem: CNS issues (lethargy, irritability, jitteriness, tremors, seizures, and CVA’s); may also have cardiopulmonary problems: respiratory distress, tachypnea, cyanosis, apnea, and CHF. #1 Metabolic problem: hypoglycemia; #2 metabolic problem: hypocalcemia. Partial exchange transfusion only indicated for symptomatic patients and for those with crits > 75% on repeated measurements. Asymptomatic patients: cardiorespiratory monitoring and monitoring of hematocrit and glucose levels every 6 hours. Disseminated neonatal herpes: High mortality; presents at 9-11 days of age but may present up to 4 weeks of age. may involve any organs but mostly the liver, adrenal glands, and lungs. DIC is common. Periventricular hemorrhage (PVH) and Intraventricular Hemorrhage (IVH): greatest risk in preemies at or less than 32 weeks of age. Occur within the first week of life. Vary in presentation from asymptomatic to a full fontanelle, decreased feeding, apnea, anemia, acidosis, posturing, or seizures. Study of choice: Ultrasound of Head Indomethacin: may decrease the risk of PVH-IVH in preemies. Hemorrhagic Disease of the Newborn (HDN): higher risk in breastfed infants, especially if vitamin K not administered immediately after birth. Appears 2-7 days of life. Vitamin K required for II, VII, IX, and X production therefore shortage initially leads to prolonged PT. In severe cases, PTT may also be prolonged. Neonatal Conditions Presenting with Bilious Vomiting: Duodenal atresia, Malrotation with midgut volvulus, Meconium Ileus, NEC Duodenal atresia: “double-bubble” sign (a paucity of gas in the abdomen and 2 air bubbles—one in the stomach and one in the duodenum); typically develop bilious vomiting in the first 24 hours of life. 4 Malrotation with midgut volvulus: infants may be well-appearing with a non-distended abdomen; however, if the bowel is already necrotic, they may present in shock; Study of choice: an upper GI series (shows the small bowel rotated to the right side of the abdomen and with contrast narrowing at the site of obstruction –“cork-screwing”); an ultrasound may show spiraling of the small bowel about the SMA; If you suspect this, treat with fluid resuscitation, triple antibiotics, NG tube and consult surgery prior to studies; infants will usually have bilious vomiting Meconium ileus: presents as a small bowel obstruction; X-rays reveal multiple dilated loops of bowel. Coarse, granular appearance of air within the inspisated meconium seen; presents with bilious vomiting, distended tender abdomen with palpable thickened loops of bowel; 95% of these infants have CF Necrotizing Enterocolitis (NEC): usually in preemies, can be seen in term infants in the first 10 days of life; history of anoxic event or stress at birth; appear ill with lethargy, irritability, anorexia, distended abdomen, bilious vomiting and bloody stools. X-Rays: pneumatosis intestinalis, may also see air in portal vein and free air if already perforated; Treatment: NG Tube, triple antibiotics; Surgical Consult Pyloric stenosis: presents as non-bilious vomiting in the 2nd to 6th weeks of life. Hourly maintenance fluid rate in pediatric patients: 4 cc/kg/hr for first 10 kg 2cc/kg/hr for the next 10 kg 1cc/kg/hr for the remainder of the weight in kg. For preemies, their mean arterial pressure is approximated by gestational age in weeks Stridor is inspiratory with supraglottic disorders (laryngomalacia) Stridor is biphasic with glottic and subglottic disorders (vocal cord disease, subglottic stenosis) Stridor is expiratory with tracheal disease (tracheomalacia) Laryngomalacia=most common cause of stridor in neonates; onset in first 2-4 weeks; stridor is worse with crying and agitation and is relieved by lying prone. Second most common cause of stridor in neonates is vocal cord paralysis Neonates with new onset stridor require admission for layngoscopy/bronchoscopy Early onset pneumonia within first 7 days of life is most commonly due to GBS—can produce rapid respiratory distress, hypotension, sepsis, meningitis; CXR shows bilateral patchy infiltrates with occasional pleural effusions. 5 Chlamydia pneumonia presents at 3 weeks or older; onset is insidious, fever is uncommon, and conjunctivitis is present in 50% of cases; CXR shows bilateral interstitial infiltrates and hyperinflation; any conjunctival discharge in a neonate with pneumonia should be tested for Chlamydia via DFA or ELISA. Congenital cardiac lesions will present in the neonatal period in one of three ways: Cyanosis, with or without CHF—but unresponsive to O2: due to right to left shunting (TOF; TAT, TOGV, TAPVR) Shock: due to outflow obstruction (mimics sepsis; hypoplastic left heart, coarctation of the aorta, interrupted aortic arch; critical aortic stenosis) CHF, with or without cyanosis—but responsive to O2: due to left to right shunting (VSD, ASD, PDA) The hyperoxia test is a useful bedside way to differentiate between cardiac and pulmonary etiologies for central cyanosis (use right upper extremity to avoid falsely depressed values cause by a right to left ductal shunt.); a PaO2 that remains < 50 despite 100% O2 is suggestive of cyanotic congenital heart disease. Treat all shocky neontaes as septic until proven otherwise; then add PGE1 if presents in shock or cyanotic, until cardiac lesion is ruled out.; then also consider CAH and check STAT electolytes for hyponatremia, hyperkalemia, and metabolic acidosis., hypoglycemia may also be present. Use acyclovir to cover HSV if: WBC’s or high protein in CSF but no organisms seen CSF pleocytosis is present with vesicular rash on infant, focal neurologic signs, pneumonitis or hepatitis, or a maternal history of herpes Elevated RBC’s in CSF Focal seizures can be caused by metabolic disorders in neonates and do not necessarily imply a focal CNS lesion. Seizures in the first 48 hours are usually due to: Birth trauma Pyridoxine dependency Hypoxic encephalopathy Hypoglycemia Benign Familial neonatal seizures begin on day 2-3 of life and resolve by 1-6 months. Infants who present at 4-7 days may be hypocalcemic due to high phosphate load from formula; hypocalcemia accounts for 33% of all neonatal seizures; is defined as plasma calcium < 7; clinical signs include jitteriness and poor feeding, tetany, twitching, vomiting, carpal-pedal spasm, clonus, laryngospasm, or stridor (or a weak cry like a baby lamb); QTc interval > 0.44 supports the diagnosis; Infuse calcium gluconate 60mg/kg 6 slowly to prevent bradycardia; Hypomagnesemia can be treated with 25-50 mg/kg IV or IM magnesium sulfate. Benign idiopathic “fifth day fits” start on the 5th day of life and cease by day 15. Seizures that present after day 7 of life are more likely to be due to infection. Opiate withdrawal seizures may present any time in the neonatal period. If child is bottle fed, poor mixing may lead to hyponatremic seizures For treatment of seizures, think about possible cause, check d-stick and lytes, and start treating as indicated with Na 3cc/kg of 3% saline, Glucose 5cc/kg of D10 H20, calcium gluconate 60mg/kg, ativan 0.05mg/kg, vitamin B 6 (pyridoxine) 100mg IV—B6 is a cofactor needed by synthesis of the inhibitory neurotransmitter GABA—infants whose mothers are in INH are at risk for vitamin B6 deficiency! ALTE is “an episode that is frightening to the observer and that is characterized by some combination of apnea, color change, change in muscle tone, choking, or gagging. In some cases the observer fears that the infant has died.” Normally, infants are soothed when rocked. Paradoxical irritability is present when an infant appears to be more comfortable when lying still than when gently rocked—this occurs in conditions like meningitis as the inflamed meninges are aggravated by motion. Healthy neonates need 110 cal/kg/day; overfed infants are given > 150cal/kg/day; calculate by knowing regular formula has 20 cal/oz (30cc). Overfed babies have more frequent stools and regurgitation/vomiting. Early introduction of solid foods prior to 4 months may increase spitting up. Renal stones or UPJ obstruction may manifest through cyclic vomiting. Vomiting associated with colicky pain and hematuria is suggestive of this diagnosis Narcotic withdrawal in an infant may be manifested by irritability and vomiting. For healthy term newborns, a loss of 5-10% from birthweight (BW) is normal. They should regain their BW in 2 weeks. They then should double their birthweight by 6 months and triple their birthweight by 1 year. During the first 3 months, an infant should gain 30g (1 ounce) per day. Child’s height should double by 4 years of age. Failure to thrive (FTT) should be considered if the weight of the infant is <3rd% or if the infant’s weight drops and crosses two percentile lines in less than 6 months. 7 Vaginal bleeding during the first week of life is most likely benign and due to the withdrawal of maternal hormones. For digit tourniquets, do longitudinal incisions at the 3 and 9 o’clock positions to avoid neurovascular and tendon structures. For tourniquets involving the genitals, consult urology. In treating infant oral thrush in the breastfeeding child, you must treat both the child and the mother. A rise in total serum bilirubin by >0.5 per hour is suggestive of hemolytic disease A history of dark urine and light stools is suggestive of cholestatic jaundice (biliary atresia). A history of prolonged jaundice (>3 weeks) is suggestive of cholestatic jaundice Age based minimum bilirubin for phototherapy in low risk infants (subtract 4 if high risk) 24 hrs old = 12 48 hrs old = 15 72 hrs old = 18 96+ hrs old = 20 High risk criteria include: prematurity, isoimmune hemolytic disease, G6PD Deficiency, asphyxia, lethargy, temperature instability, sepsis, acidosis, albumin <0.3 Breast enlargement (hypertrophy) is common in newborns and is due to stimulation of breast tissue by transplacental transfer of maternal hormones. can be asymmetric, and sometimes is associated with a whitish nipple discharge, termed “witch's milk.” Resolves spontaneously, give reassurance and advice against manipulation of the breast tissue. Neonatal mastitis or infection of the breast tissue is a less common condition that occurs within the first 5 postnatal weeks in term infants. Girls are twice as likely to be affected as boys, and in most cases, the condition is unilateral. Patients may present with signs of infection in the form of erythema, induration, tenderness, warmth, and nipple discharge. Infants who have neonatal mastitis should have complete blood cell counts measured and blood cultures performed. Nipple discharge should be sent for Gram stain and culture. IV antibiotics are recommended as initial therapy. Unless a Gram stain of purulent discharge is available to direct ABX therapy, an antistaphylococcal antibiotic and cefotaxime should be used. I&D by a surgeon should be reserved for cases that do not resolve with antibiotics or when a fluctuant mass suggestive of a breast abscess is palpable. 8