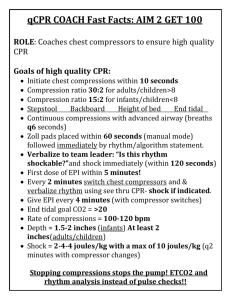
Team Focused CPR
advertisement
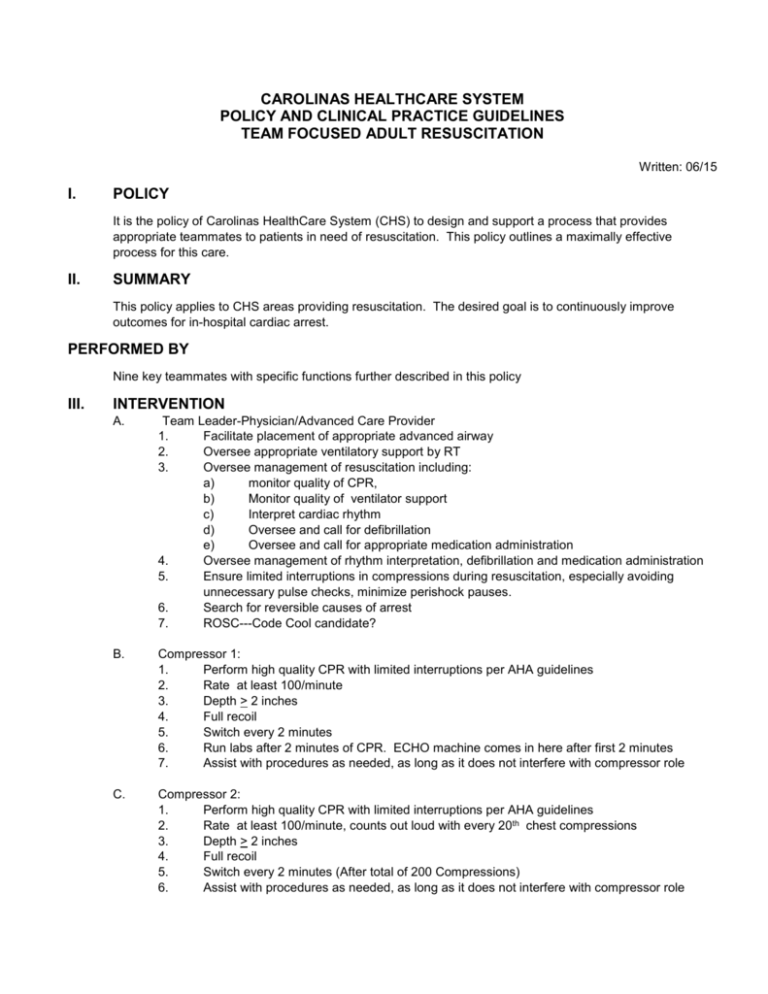
CAROLINAS HEALTHCARE SYSTEM POLICY AND CLINICAL PRACTICE GUIDELINES TEAM FOCUSED ADULT RESUSCITATION Written: 06/15 I. POLICY It is the policy of Carolinas HealthCare System (CHS) to design and support a process that provides appropriate teammates to patients in need of resuscitation. This policy outlines a maximally effective process for this care. II. SUMMARY This policy applies to CHS areas providing resuscitation. The desired goal is to continuously improve outcomes for in-hospital cardiac arrest. PERFORMED BY Nine key teammates with specific functions further described in this policy III. INTERVENTION A. Team Leader-Physician/Advanced Care Provider 1. Facilitate placement of appropriate advanced airway 2. Oversee appropriate ventilatory support by RT 3. Oversee management of resuscitation including: a) monitor quality of CPR, b) Monitor quality of ventilator support c) Interpret cardiac rhythm d) Oversee and call for defibrillation e) Oversee and call for appropriate medication administration 4. Oversee management of rhythm interpretation, defibrillation and medication administration 5. Ensure limited interruptions in compressions during resuscitation, especially avoiding unnecessary pulse checks, minimize perishock pauses. 6. Search for reversible causes of arrest 7. ROSC---Code Cool candidate? B. Compressor 1: 1. Perform high quality CPR with limited interruptions per AHA guidelines 2. Rate at least 100/minute 3. Depth > 2 inches 4. Full recoil 5. Switch every 2 minutes 6. Run labs after 2 minutes of CPR. ECHO machine comes in here after first 2 minutes 7. Assist with procedures as needed, as long as it does not interfere with compressor role C. Compressor 2: 1. Perform high quality CPR with limited interruptions per AHA guidelines 2. Rate at least 100/minute, counts out loud with every 20th chest compressions 3. Depth > 2 inches 4. Full recoil 5. Switch every 2 minutes (After total of 200 Compressions) 6. Assist with procedures as needed, as long as it does not interfere with compressor role D. E. Compressor 3: 1. Perform high quality CPR with limited interruptions per AHA guidelines 2. Rate at least 100/minute, counts out loud with every 20th chest compressions 3. Depth > 2 inches 4. Full recoil 5. Switch every 2 minutes (After total of 200 Compressions) 6. Assist with procedures as needed, as long as it does not interfere with compressor role. RN 2 (Code Cart RN): 1. Assist with rhythm interpretation 2. Operate defibrillator as ordered/needed, charges defibrillator at compressors count of 180, delivers shock if indicated after 200 compressions complete and rhythm is analyzed. 3. Deliver medications from Code Cart, mix and deliver all stat drips 4. Ensure adequate IV/IO access 5. Send runner for medications not in Code Cart 6. Ensure team leader and recorder are aware of all treatments F. RN 3 (Bedside RN): 1. Assist with compressions as needed 2. Obtain specimens and additional IV access as ordered/needed 3. Prepares stat drips of medications not on Code Cart, checks dosages with Recorder/CPR Quality Monitor or Code Cart RN 4. Ensure team leader and recorder are aware of all medications administered 5. Ensure team leader and recorder are aware of all procedures performed on patient G. Respiratory Therapy: 1. Obtain/Maintain appropriate airway 2. Provide appropriate ventilations—Do not hyperventilate 3. Breaths <12/minute with minimal chest rise, gives a breath with every 20th chest compression 4. Monitor ETCO2 H. Recorder RN 1: 1. Records resuscitation efforts on appropriate Code Sheet 2. Monitors and records times of CPR cycles, medication administration and other procedures as performed 3. Prompts team leader when CPR cycles are about to be completed, providers information to team leader as requested I. Manager, Nursing Supervisor, Clinical Supervisor or Charge Nurse 1. Manage personnel and visitors 2. Provides family support, if needed 3. Obtain medications and supplies not available at bedside J. Family Support Facilitator 1. Provide information, explanations and general support to family present during resuscitation 2. Provide updates to family not present at bedside Maintain/Obtain appropriate airway Team Resuscitation Positions Provide appropriate ventilations--Do not hyperventilate. Breaths<12/minute with minimal chest rise, give breath with every 20 chest compression Counts out loud with every 20th chest compression (Switch after 200 compressions) Compressor 3 Monitor ETCO2 Depth > 2 inches Respiratory Therapist Counts out loud with every 20th compression (Switch after 200 compressions) Full recoil Run labs after 2 minutes of CPR. US machine comes in here after first 2 minutes Depth >2 inches Compressor 2 Assist with compressions as needed Compressor 1 Full recoil RN Obtain specimens and additional IV access as ordered/needed RN 3 2 Prepares stat drips of medications not on Code Cart, checks dosages with Recorder/CPR Quality Monitor or Code Cart RN Charges Defib at Compression count 180, delivers shock if indicated after 200 compressions complete and rhythm is analyzed Ensure team leader and recorder are aware of all medications administered Ensure team leader and recorder are aware of all procedures performed on patient Assist with Rhythm interpretation Physician CODE CART Deliver medications from Code Cart, mix and deliver all stat drips 1 Monitor/Defib Ensure team leader and recorder are aware of all treatments Facilitate placement of appropriate advanced airway Oversee appropriate ventilator support by RT Recorder RN 1 Physician Records resuscitation efforts on appropriate Code Sheet Monitors and records times of CPR cycles, medication administration and other procedures as performed Prompts team leader when CPR cycles are about to be completed, provides information to team leader as requested Monitors compressions and resuscitation process Provide information, explanations and general support to family present during Family resuscitation Support Facilitator Provide updates to family not present at bedside 2 Oversee management of resuscitation-monitoring quality of CPR, ventilations etc. (Physician 1 feels for pulse at compression count of 160, at count 200 analyze rhythm for possible shock) Oversee management of rhythm interpretation, defibrillation and medication administration Ensure limited interruptions in compressions during resuscitation, especially avoiding unnecessary pulse checks, minimize perishock pauses Search for reversible causes of arrest Manager/Nursing Supervisor/Charge RN/Clinical Supervisor Manage personnel and visitors Provides family support if needed Obtains medications and supplies not at bedside Team Resuscitation Positions Respiratory Therapist Compressor 3 Compressor 2 Compressor 1 RN RN 3 2 Recorder/ RN 1 CODE CART Monitor/Defib Physician 1 Physician 2 Family Support Facilitator Manager/Nursing Supervisor/Charge RN/Clinical Supervisor TFCPR Resuscitation Immediate Debrief Tool Task Yes No Comments/Intervention (If No Why?) Team Structure & Dynamics All roles were assigned/managed Team leader easily identified Appropriate personnel available Was noise limited & teammate instructions easily heard? Observers kept to a minimum/observed from doorway? Mechanisms to determine quality of compressions used: ETCO2 CPR Monitoring Device Defibrillator monitor feedback Team leader monitoring & feedback Minimally-interrupted chest compression/high-quality CPR performance CPR initiated within 10 seconds of arrest All compression cycles (2 minutes or 200 compressions) performed to completion Compressions continued during IV/IO access Compressions continued during airway management (BVM, KingLT, ETI) Interruptions limited to < 10 seconds when no return of circulation identified Vast majority of compressions were of high-quality (appropriate rate, depth, full recoil)? Compressors rotate every 2 minutes Ventilation given every 20 compressions Early defibrillation Charging defibrillator occurred at 180 compressions every cycle Post-arrest care Code Cool Initiated? Other comments: Teammate name debriefing_________________Signature: ______________ Date: _______ Location: ________ Teammate’s names (participating in cardiac arrest resuscitation): RT: ______________________________________ Compressor 1: ________________________________ Compressor 2: _____________________________Compressor 3: ________________________________ RN 1: _________________________________________ RN 2: _________________________________________ RN 3: _________________________________________ Physician 1: _________________________________ Physician 2: ____________________________________ Family Support Facilitor: __________________________