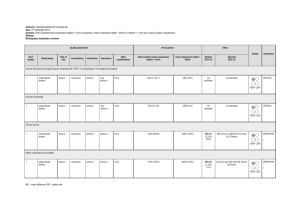
PEA-management
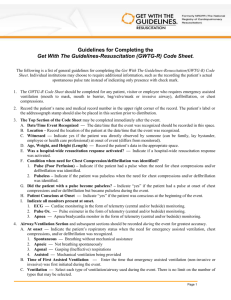
advertisement
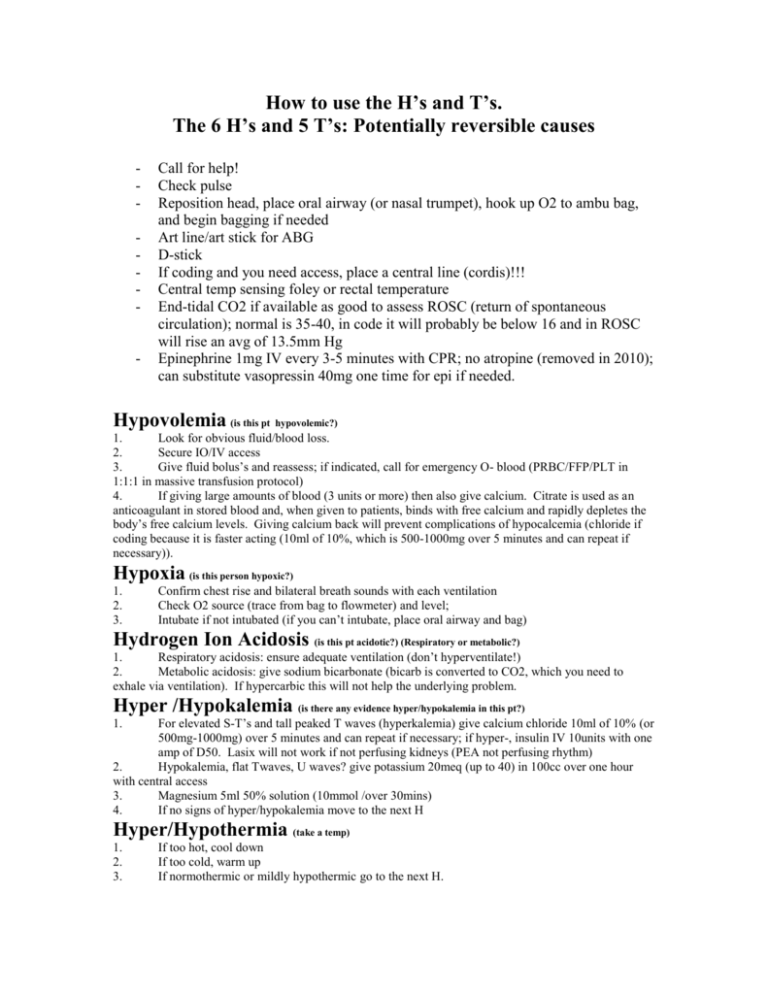
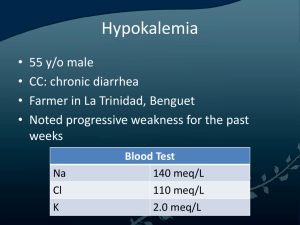
How to use the H’s and T’s. The 6 H’s and 5 T’s: Potentially reversible causes - - Call for help! Check pulse Reposition head, place oral airway (or nasal trumpet), hook up O2 to ambu bag, and begin bagging if needed Art line/art stick for ABG D-stick If coding and you need access, place a central line (cordis)!!! Central temp sensing foley or rectal temperature End-tidal CO2 if available as good to assess ROSC (return of spontaneous circulation); normal is 35-40, in code it will probably be below 16 and in ROSC will rise an avg of 13.5mm Hg Epinephrine 1mg IV every 3-5 minutes with CPR; no atropine (removed in 2010); can substitute vasopressin 40mg one time for epi if needed. Hypovolemia (is this pt hypovolemic?) 1. Look for obvious fluid/blood loss. 2. Secure IO/IV access 3. Give fluid bolus’s and reassess; if indicated, call for emergency O- blood (PRBC/FFP/PLT in 1:1:1 in massive transfusion protocol) 4. If giving large amounts of blood (3 units or more) then also give calcium. Citrate is used as an anticoagulant in stored blood and, when given to patients, binds with free calcium and rapidly depletes the body’s free calcium levels. Giving calcium back will prevent complications of hypocalcemia (chloride if coding because it is faster acting (10ml of 10%, which is 500-1000mg over 5 minutes and can repeat if necessary)). Hypoxia (is this person hypoxic?) 1. 2. 3. Confirm chest rise and bilateral breath sounds with each ventilation Check O2 source (trace from bag to flowmeter) and level; Intubate if not intubated (if you can’t intubate, place oral airway and bag) Hydrogen Ion Acidosis (is this pt acidotic?) (Respiratory or metabolic?) 1. Respiratory acidosis: ensure adequate ventilation (don’t hyperventilate!) 2. Metabolic acidosis: give sodium bicarbonate (bicarb is converted to CO2, which you need to exhale via ventilation). If hypercarbic this will not help the underlying problem. Hyper /Hypokalemia (is there any evidence hyper/hypokalemia in this pt?) For elevated S-T’s and tall peaked T waves (hyperkalemia) give calcium chloride 10ml of 10% (or 500mg-1000mg) over 5 minutes and can repeat if necessary; if hyper-, insulin IV 10units with one amp of D50. Lasix will not work if not perfusing kidneys (PEA not perfusing rhythm) 2. Hypokalemia, flat Twaves, U waves? give potassium 20meq (up to 40) in 100cc over one hour with central access 3. Magnesium 5ml 50% solution (10mmol /over 30mins) 4. If no signs of hyper/hypokalemia move to the next H 1. Hyper/Hypothermia (take a temp) 1. 2. 3. If too hot, cool down If too cold, warm up If normothermic or mildly hypothermic go to the next H. Hypo/Hyperglycemia 1. Accu-check and correct if needed. If hyperglycemic, probably NOT in DKA; probably in hyperglycemic, hyperosmolar, non-ketotic state and are profoundly hypovolemic. Tablets (drug OD, accidents) 1. 2. 3. Support circulation while you find an antidote or reverse drug if one is suspected. (poison control) Give NARCAN if found down If no drug OD suspected, move on to the next T. Tamponade (chest trauma, chest malignancy, recent central line insertion, JVD, narrow pulse pressure, electrical alternans etc…). Pulse pressure may have been narrowing rapidly prior to PEA. 1. Pericardial centesis 2. If no history or ruled out move on to the next T. Tension Pneumothorax (chestasymmetry, tympani, diminished breath sounds, high peak pressures, JVD, tracheal deviation, severe respiratory distress etc…) 1. Vent tension in chest (“nobody dies without a needle in their chest”); needle the chest with a 14g catheter at least 2 inches in length 2. Support ventilation and oxygenation with BVM and intubate if necessary 3. If no history or ruled out move on to the next T. Thrombosis (coronary or pulmonary) 1. 2. 3. Consider fibrinolysis for suspected coronary or pulmonary embolus. CPR is not an absolute contraindication for fibrinolysis. If no history or ruled out move on to the next T. Trauma 1. Inspect body completely. Remove all clothes. 2. Secure airway 3. Control external bleeding with tamponade while concurrently delivering volume with isotonic crystalloids and blood products (LR is less acidodic than NS but you cannot give blood with LR). 4. FAST exam: look for internal bleeding (tap the abdomen if suspicious for internal bleed)and take to OR within a couple of minutes. 5. If no history or ruled out move on to the next check mark for trauma 6. Instead of starting compressions, consider bilateral chest tubes, aggressive fluids, and aggressive blood product infusion 1. Compressions won’t help because there is no volume in their system 2. Compressions will likely come from direct cardiac massage 7. If you will add massive transfusion in trauma, be sure to add tourniquets where you can; otherwise you are transfusing the floor.