GMEC Minutes 12-18-2014 - University of South Carolina
advertisement
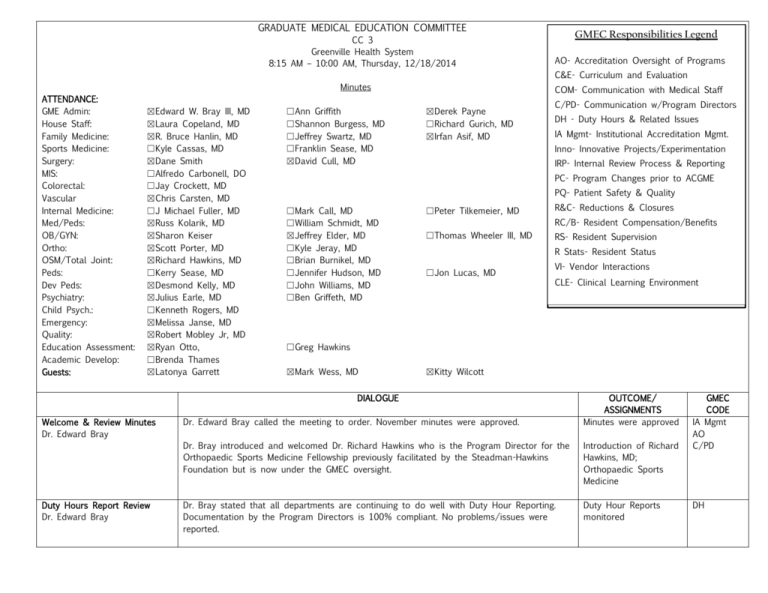
GRADUATE MEDICAL EDUCATION COMMITTEE CC 3 Greenville Health System 8:15 AM – 10:00 AM, Thursday, 12/18/2014 GMEC Responsibilities Legend AO- Accreditation Oversight of Programs C&E- Curriculum and Evaluation Minutes ATTENDANCE: GME Admin: House Staff: Family Medicine: Sports Medicine: Surgery: MIS: Colorectal: Vascular Internal Medicine: Med/Peds: OB/GYN: Ortho: OSM/Total Joint: Peds: Dev Peds: Psychiatry: Child Psych.: Emergency: Quality: Education Assessment: Academic Develop: Guests: ☒Edward W. Bray III, MD ☒Laura Copeland, MD ☒R. Bruce Hanlin, MD ☐Kyle Cassas, MD ☒Dane Smith ☐Alfredo Carbonell, DO ☐Jay Crockett, MD ☒Chris Carsten, MD ☐J Michael Fuller, MD ☒Russ Kolarik, MD ☒Sharon Keiser ☒Scott Porter, MD ☒Richard Hawkins, MD ☐Kerry Sease, MD ☒Desmond Kelly, MD ☒Julius Earle, MD ☐Kenneth Rogers, MD ☒Melissa Janse, MD ☒Robert Mobley Jr, MD ☒Ryan Otto, ☐Brenda Thames ☒Latonya Garrett ☐Ann Griffith ☐Shannon Burgess, MD ☐Jeffrey Swartz, MD ☐Franklin Sease, MD ☒David Cull, MD COM- Communication with Medical Staff ☒Derek Payne ☐Richard Gurich, MD ☒Irfan Asif, MD C/PD- Communication w/Program Directors DH - Duty Hours & Related Issues IA Mgmt- Institutional Accreditation Mgmt. Inno- Innovative Projects/Experimentation IRP- Internal Review Process & Reporting PC- Program Changes prior to ACGME PQ- Patient Safety & Quality ☐Mark Call, MD ☐William Schmidt, MD ☒Jeffrey Elder, MD ☐Kyle Jeray, MD ☐Brian Burnikel, MD ☐Jennifer Hudson, MD ☐John Williams, MD ☐Ben Griffeth, MD ☐Peter Tilkemeier, MD R&C- Reductions & Closures RC/B- Resident Compensation/Benefits ☐Thomas Wheeler III, MD RS- Resident Supervision R Stats- Resident Status ☐Jon Lucas, MD VI- Vendor Interactions CLE- Clinical Learning Environment ☐Greg Hawkins ☒Mark Wess, MD ☒Kitty Wilcott DIALOGUE Welcome & Review Minutes Dr. Edward Bray Duty Hours Report Review Dr. Edward Bray Dr. Edward Bray called the meeting to order. November minutes were approved. OUTCOME/ ASSIGNMENTS Minutes were approved Dr. Bray introduced and welcomed Dr. Richard Hawkins who is the Program Director for the Orthopaedic Sports Medicine Fellowship previously facilitated by the Steadman-Hawkins Foundation but is now under the GMEC oversight. Introduction of Richard Hawkins, MD; Orthopaedic Sports Medicine Dr. Bray stated that all departments are continuing to do well with Duty Hour Reporting. Documentation by the Program Directors is 100% compliant. No problems/issues were reported. Duty Hour Reports monitored GMEC CODE IA Mgmt AO C/PD DH House Senate Report Dr. Laura Copeland Dr. Laura Copeland reported that the resident food drive was successful. A competition that involved residents from each department raised 1400lbs of food that was donated to charity. Dr. Copeland also stated that the residents are looking to start more projects in the future. IA Mgmt AO C/PD PQ Dr. Copeland reported that during the last House Staff meeting the GHS Lab Department’s Dr. Knight and Ginger Smith attended to discuss dropped or missed lab orders. Various lab processing improvements were discussed and the lab was very supportive of improving processes and the residents’ concern regarding patient safety. Dr. Bray stated that he would like for the financial consultant regarding a specialty disability insurance proposal to present their information to the House Senate Leadership. Dr. Bray stated that this is the best unisex policy rate that he has seen offered and that it is highly competitive in the market. Dr. Bray reported that HR has approved the proposal and other institutions have taken part in this program, (i.e. MUSC and Wake Forrest). ACGME Communications Dr. Edward Bray PQ HR approved offering the specialty disability insurance policy. Information will be presented to the House Senate. RC/B Dr. Scott Porter stated that this policy is attractive and agrees that the proposal should be presented to the House Senate. In addition, he adds that the company also has a desire to address the House Staff as a whole with unbiased financial planning as part of the Business in Medicine curriculum. Dr. Julius Earle agreed with Dr. Porter regarding the need to provide these topics to graduating residents within the business in medicine curriculum. C&E Dr. Bray asked if any department had any direct communication with ACGME that need to be reported. No one reported any communications. Dr. Bray stated that there was an ecommunication sent out on December 1st regarding Phase I Site delay. The communication is noted on the GMEC SharePoint. IA Mgmt AO Dr. Bray also reminded the Program Directors of the deadline to update contact information with in the ADS system. Dr. Bray reiterated that the accounts in ADS are how the ACGME contacts a specific department. C/PD Dr. Julius Earle reported one resident has been placed on remediation to address professionalism competencies and inappropriate communication. A medical student reported that the resident had used nicknames in addressing them and did not stop in spite of being asked to discontinue the behavior. It was also reported that a medical student felt the resident did not monitor or intervene appropriately during an interview with a hypersexual. The School of Medicine and GHS Human Resources have been notified. The PGYIII resident will be assigned to additional training on professionalism and appropriate communication. Dr. Earle reported that the residents have rapport and a level of comfort with each other but this behavior should not have been assumed appropriate for any concerned. Dr. Earle reported that he does not think there was any egregious intent and that the incident has been taken seriously and has been addressed. PGY III Psychiatry resident being remediated on professionalism and appropriate interpersonal communication/ teaching RS R Stats 2 ACGME CommunicationsCont’d. Dr. Edward Bray EPIC and eCW Orientation Training Needs Dr. Mark Wess Dr. Asif reported a PGYII female was placed on remediation for rotation standards not being met. Despite continued improvement efforts and feedback this PGYII was still not meeting standards. The CCC met after her semi-annual evaluation and a decision was made put her on probation. A meeting was held with the resident and all of her options/appeal process was discussed. The next day the resident decided to resign. Dr. Bray introduced and welcomed Dr. Mark Wess, Chief Medical Information Officer. Dr. Bray stated that Dr. Wess will further explain what the needs are regarding eCW and upcoming EPIC training and responsibilities. Dr. Bray stated that the system change from eCW to EPIC is slated for July 16th. The residents start on July 1st which presents a problematic training issue. The question posed was, “How much time do we spend during orientation with these trainings when eCW will be used only 2 weeks prior to the go live date for EPIC?” Family Medicine PGY II resignation R Stats Dr. Wess discussed resident EMR training needs for new residents with the go live implementation of EPIC C&E C/PD Dr. Wess stated that EPIC training will roll out in many phases. Dr. Wess reported a go live pilot for EPIC on June 4th which includes 33 providers/practice sites. Ambulatory users go live is scheduled for July 16th. Other hospital satellite facilities will go live in 2016. Dr. Wess further stated that there is an EPIC Center link on GHS website that detail the go live dates. EPIC training requires 4-7 hours of Computer Based Training (CBT) and 1 full ½ day of instructor-led training. Dr. Wess stated that there is an inpatient component as well that some departments will also have to complete that will take place in January/February 2016. Dr. Wess stated that for the 10 business days prior to go live a determining factor could be whether or not a resident is scheduled for clinic. Dr. Wess reiterated that access to EPIC will not be granted to residents who do not complete the training and pass a test. Dr. Wess opened the discussion for questions. Dr. Scott Porter questioned why they chose to implement the go live during a time of high turnover with residents. Dr. Wess answered that the dates are flexible; however, moving the date back has a cost involved. Dr. Wess also stated that upper management felt this timeframe was the best. Dr. Irfan Asif asked how much time an intern will need to be proficient. Dr. Wess answered stating that 4-7 hours of CBT could be completed in during clinical service downtime in 30 minute increments. In addition, residents would have to attend a full ½ day (4 ½ hour) of instructor-led hands-on training and pass a test. In summary, Dr. Wess stated that an intern could complete the training and test in 2-3 days. Dr. Chris Carson asked about the class size capacity. in the class were ideal with 30 being the maximum. Dr. Wess stated that 15-30 people Dr. Sharon Keiser asked if this training could be added into the Orientation schedule for incoming house staff? Dr. Wess stated that he has spoken with Ann Griffith, Manager of the Graduate Medical Education (GME) Program, whom stated that the Orientation schedule was already full and the addition was probably not possible. 3 EPIC and eCW Orientation Training Needs-Cont’d. Dr. Mark Wess Dr. Russ Kolarik inquired if existing house staff could complete training in June and the new house staff complete in July? Dr. Wess answered yes existing house staff will be scheduled. C&E C/PD Dr. Scott Porter asked if the training counts against the 80 hour work week. Dr. Wess answered yes. Dr. Wess stated that acute facilities will go live in February 2016. Dr. Bray asked that each residency department to report back to Dr. Wess regarding their need for eCW training during orientation and to contact Margaret Durham who is the training coordinator for the EPIC training schedule for the existing residents? Dr. Scott Porter asked how we are to know as to whether a resident can omit eCW training. Dr. Wess answered if you expect an incoming resident to document in eCW previous to July then they will need training. If they are just utilizing view print, shadowing or learning the process then no training is required. In addition, Dr. Wess stated that omitting the use of eCW could cause data integrity problems. Dr. Wess stated that if the expectation is for an intern/resident to document in eCW within the first 2 weeks in July then they would need eCW training. Dr. Sharon Keiser inquired about a new resident or intern that already had training in EPIC. Dr. Wess stated that they would have a fast track available but some training would be necessary. Dr. Bray stated that some residents must have eCW but not all. He further understands that problems arise when they transfer into other departments where eCW is being utilized. Dr. Bray asked that the Program Directors report their resident training needs to Dr. Wess and Ms. Durham. 3-Year GME Expansion Plans Dr. Edward Bray Program Directors are to report back to Dr. Wess regarding their need for eCW training during orientation and to contact Margaret Durham who is the training coordinator for the EPIC training schedule for the existing residents training. Dr. Bray reminded Program Directors that the 3-Year Expansion Plans are due by the end of the month. Dr. Bray stated that GME Expansion Reviews are scheduled for the January GMEC Meeting. 4 new residency/fellowships (Joint Peds Genetic, Maternal-Fetal Medicine, Internal Medicine Fellowships-Gastroenterology, Infectious Disease and Cardiology) have been submitted. Dr. Bray stated that Emergency Medicine had previously been approved by GMEC; but, the Resource Council (RC) has requested revision in the financial plan. The EM revised 3-year projected budget has been submitted for AC review. In addition, EM needed a Department Chair in place. They have now met all of those requirements and will not have to re-visited by GMEC until funding approval by AC. Dr. Bray added that the remaining proposals are on SharePoint and should be read prior to GMEC presentations. Program Directors are asked to ensure familiarity of each proposal in preparation for voting during the next meeting. IA Mgmt AO Program Directors must review proposed new residency/fellowship programs applications prior to the next GMEC Meeting. 4 Academic Council Update Derek Payne Derek Payne stated that the Academic Council discussed scholarly publications during it meeting earlier this morning and reported that the council is looking at quality and not quantity goals when it comes to publications and how they are chosen. Mr. Payne stated that a press conference earlier stated GHS was starting a Physician Assistant (PA) program. The council is still reviewing the financials around this implementation and is close to making a decision within the next few weeks. In addition, the number of students’ experiences at the organization is starting to strain the institution. As a result Dr. Youkey is putting a group together to review the capacity issues. Due to the implementation of EPIC in July, budgetary questions and deadlines will begin in February or March IA Mgmt C/PD Com Mr. Payne stated that those with Clemson appointments will have access to Clemson resources. An email will be sent out with specific instructions at a later date. Dates for EPIC happen in the summer and because that is typically when budgeting occurs, finance has been asked to have the budget process completed by June 1 st. As a result or the rescheduling, the budget process will begin in February or March; communications will forthcoming for budgetary questions and deadlines. Resident Salary Comparison Kitty Wilcott Kitty Wilcott presented recommended raises for PGYI, PGYII and PGYIII. Ms. Wilcott stated that according to the national compensation rates from AHEC that GHS salaries are lower than average. As a result, a 1.35% pay increase is proposed. Dr. Scott Porter asked if the total benefit package was taken into consideration in comparison (i.e. free food, iPhone, iPad etc.). Dr. Bray answered stating that the residents look at pay, other benefits are important but that everyone has an array of benefits and that but this information is not available to us. Dr. Bray further explained that the information provided is salary. If GMEC doesn’t feel we need to have a cost of living increase, then we do not have to approve. Kitty Wilcott will provide Program Directors with the Resident/Faculty Benefit Survey which includes more benefit information in addition to salary. IA Mgmt AO C/PD RC/B Dr. Robert Hanlin stated that this will affect Family Medicine existing residents as well. Mr. Payne interjected that from a budget standpoint this proposal would align within the 2015-2016 budget. Mr. Payne stated typically they do 2% range when setting the budget. Dr. Spence Taylor, Senior Assoc. Dean for Academic Affairs and President, GHS Clinical University is in support of the increase. Dr. Bray asked if there was a motion to approve. Dr. Porter asked if we could get the other benefit information he previously mentioned. Mrs. Wilcott stated that she did pull a Resident/Faculty Benefits Survey and it does list some of the benefits offered by other institutions and would forward the information to Program Directors. GMEC deferred voting to next month and after review of the additional information. GMEC deferred voting to next month and after review of the additional information. 5 CLER Moment: Subcommittee Update: Dr. David Cull Dr. David Cull presented an update regarding the CLER Sub-committee on Professionalism and Supervision and how they have addressed the reported CLER issues. The committee has reviewed: a) b) c) d) IA Mgmt AO Current professionalism and supervision policies and their importance What are we doing to promote professionalism and good supervision What is the ideal Clinical Learning Environment regarding supervision and professionalism How are we doing as it relates to ACGME site survey and what should we do next Dr. Cull stated that he had reviewed all of the program’s PIFs (Program Information Form) and was pleased that most include policies regarding professionalism and supervision. He stated that there is no need to write more policies. Dr. Cull stated that Family Medicine and Peds had good examples of best practice pertaining to professionalism. Dr. Cull stated that Surgery and Orthopaedics have good supervision policies in place. He gave an example of their procedure log used to ensure residents had documented experience before practice through simulation. Dr. Cull stated that his presentation and surveys were located in SharePoint for review. Dr. Cull addressed some of the vulnerabilities identified by CLER survey, specific instances to be targeted by GMEC and improved: 1. Does Leadership periodically assess/monitor for the culture of professionalism of medical staff/residency? Dr. Cull interpreted this to mean does the institution have monitoring in place to promote a culture of professionalism. Proper supervision will be addressed by the program directors implementing change over time. 2. The hospital does not have a procedure/policy in place for nursing staff to identify resident’s competency. Dr. Bray is currently working on this issue. 3. Patient awareness as it relates to their care. Dr. Cull explained that they wanted to know if the patient was aware of the roles of those who were directly providing care. 4. Residents polled 11-16% felt pressured to compromise their integrity to do what the attending asked them to do or document. Dr. Bray responded in the scope of how many patient interactions they have over the course of 1 month (thousands) the percentage isn’t as bad as it would appear. Also the resident may not understand the reasoning behind the attending’s decision. Dr. Bray stated that he had presented the end-of-the-year report (AIR) to the Board of Trustees and that it was well received but one of the board members did question the 11% integrity. Dr. Cull stated that GMEC needs to make some recommendations for monitoring. Dr. Cull stated in summary that there were no serious red flags for professionalism and supervision. Dr. Cull stated that the committee recommends that the GME Office should utilize a targeted annual survey of faculty, residents and patients to show if we are establishing a culture of professionalism. The committee also recommended that IT is monitored to ensure proper usage. Recommendation: GME Office annually survey faculty, residents and patients and monitor each departments training activities to assess the culture of professionalism and supervision. C/PD C&E 6 CLER Moment: Subcommittee Update- Cont’d.: Dr. David Cull It was also suggested that the GME Office obtain information from program directors regarding specific activities/training that are being done for professionalism and supervision. Dr. Bray stated that the ACGME doesn’t recognize the title fellow, they say PGYVI or PGYVII resident thus all of the consent forms use resident. Annual Reports Dr. Desmond Kelly Dr. Russ Kolarik Dr. Desmond Kelly presented the Pediatrics Annual Report stating that the board pass rate was 100%. One third of the graduates are going into fellowship training. Scholarly activity has been successful with 19 Peer reviews, 21 book/book chapter published, 10 poster presentations presented and one of which the National Meeting is publishing. Dr. Desmond Kelly presented the Developmental Pediatrics Annual Report stating that they have a new program coordinator - Melinda Lavallee-Turner (1.6 FTE shared with the residency program). Did not have board exams last year as they are every other year, but have been above average. Dr. Kelly reported the program ranked number one in the Match and the caliber of applicants has improved tremendously. Dr. Kelly will provide a response to CLER at a later time. Dr. Fuller was absent and his portion of the CLER is postponed as well. GMEC approved the Annual Reports for the following programs: Pediatrics Developmental Peds Combined Med/Peds IA Mgmt IRP AO Dr. Russ Kolarik presented the Combined Internal Medicine/Pediatrics Annual Report stating that the program was operating at full capacity of 5 residents. Dr. Kolarik reported that the program has received national exposure due to their website; especially, in response to resident testimonials. This attention has caused applicant interest to improve. This year 50 candidates are on the Med Peds waiting list. Dr. Kolarik reported all of their graduates stayed in the area of primary care and 2 were faculty hires. He reported that board pass rates are slightly above average. The goal is to improve board pass rates even more. The next site visit is scheduled for 2018. In addition, the residents have done well in AAP/ACP awards for scholarly activity. Dates to Remember Dr. Edward Bray 3-Year Plans and Expansion Requests are Due Dec. 30th ACGME Milestone Evaluations Due: January 9, 2015 - to date the DIO has received notice of any program milestones have been submitted. The following programs reports are due to ADS: (Internal Medicine, Ob/Gyn, Family Medicine, Orthopaedic Surgery, Surgery, Peds, Dev. Peds and Psychiatry) Program Directors are to submit milestone reports to ADS in a timely manner. C/PD AO IA Mgmt Match Deadlines: Jan 31 11:59 pm Quota Change/Rank Order List Feb. 25 ACGME Annual Mtg: Feb 26- March 1, 2015 held in San Diego, CA AHME Institute National Meeting: May 13-15, 2015 7 Other Business Dr. Edward Bray Dr. Bray asked if there were other business items. IA Mgmt R Stats Dr. Irfan Asif questioned the group regarding fatigue issues. Dr. Asif explained that a resident has been complaining of fatigue due to rotation schedules. Drs. Scott Porter and Chris Carsten stated that the resident should be urged to utilize the 5 weeks of vacation/PTO. Dr. Elder stated to have good communication to ensure there are no other issues like depression. Adjourn Dr. Edward Bray There being no further business, the meeting adjourned at 9:45 AM. Next Meeting: 1/22/2015; 8:00 AM in CC3. AO IA Mgmt C/PD 8