How to Deliver Twins?
advertisement
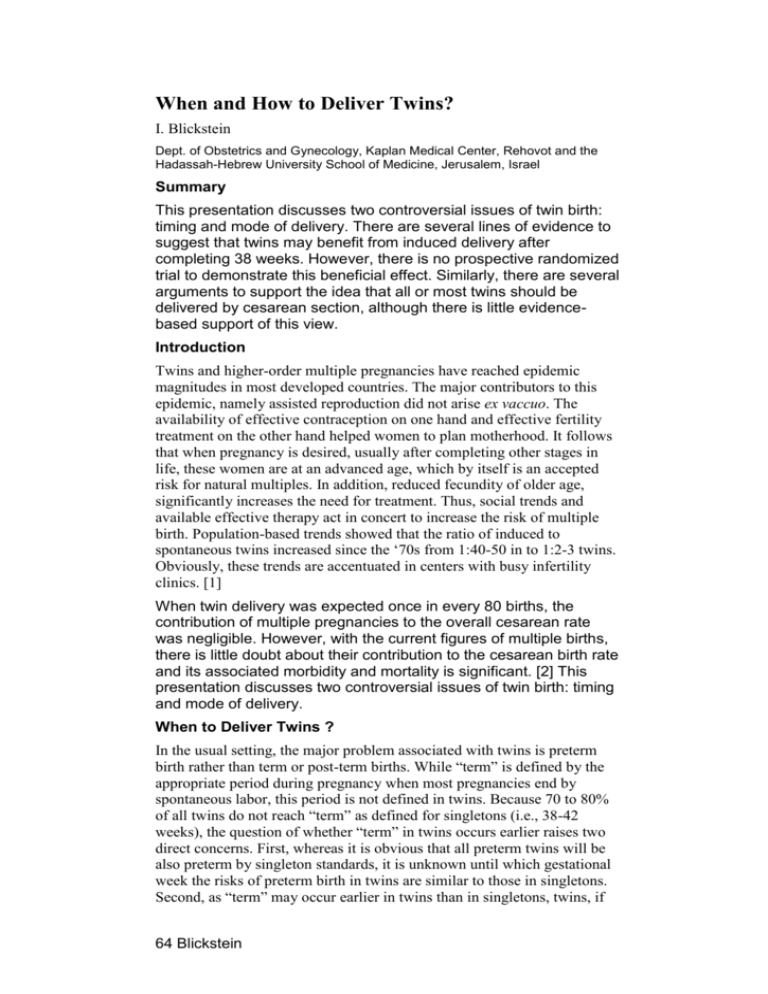
When and How to Deliver Twins? I. Blickstein Dept. of Obstetrics and Gynecology, Kaplan Medical Center, Rehovot and the Hadassah-Hebrew University School of Medicine, Jerusalem, Israel Summary This presentation discusses two controversial issues of twin birth: timing and mode of delivery. There are several lines of evidence to suggest that twins may benefit from induced delivery after completing 38 weeks. However, there is no prospective randomized trial to demonstrate this beneficial effect. Similarly, there are several arguments to support the idea that all or most twins should be delivered by cesarean section, although there is little evidencebased support of this view. Introduction Twins and higher-order multiple pregnancies have reached epidemic magnitudes in most developed countries. The major contributors to this epidemic, namely assisted reproduction did not arise ex vaccuo. The availability of effective contraception on one hand and effective fertility treatment on the other hand helped women to plan motherhood. It follows that when pregnancy is desired, usually after completing other stages in life, these women are at an advanced age, which by itself is an accepted risk for natural multiples. In addition, reduced fecundity of older age, significantly increases the need for treatment. Thus, social trends and available effective therapy act in concert to increase the risk of multiple birth. Population-based trends showed that the ratio of induced to spontaneous twins increased since the ‘70s from 1:40-50 in to 1:2-3 twins. Obviously, these trends are accentuated in centers with busy infertility clinics. [1] When twin delivery was expected once in every 80 births, the contribution of multiple pregnancies to the overall cesarean rate was negligible. However, with the current figures of multiple births, there is little doubt about their contribution to the cesarean birth rate and its associated morbidity and mortality is significant. [2] This presentation discusses two controversial issues of twin birth: timing and mode of delivery. When to Deliver Twins ? In the usual setting, the major problem associated with twins is preterm birth rather than term or post-term births. While “term” is defined by the appropriate period during pregnancy when most pregnancies end by spontaneous labor, this period is not defined in twins. Because 70 to 80% of all twins do not reach “term” as defined for singletons (i.e., 38-42 weeks), the question of whether “term” in twins occurs earlier raises two direct concerns. First, whereas it is obvious that all preterm twins will be also preterm by singleton standards, it is unknown until which gestational week the risks of preterm birth in twins are similar to those in singletons. Second, as “term” may occur earlier in twins than in singletons, twins, if 64 Blickstein carried to the singleton-“term”, may be exposed to unnecessary risks of post-“term” pregnancy. There are several lines of evidence to support the concept that “term” in twins occurs before 38 weeks’ gestation. Statistical The distribution of twin births by gestational age is almost identical to that of singletons, but shifted towards a lower gestational age. The ‘tails’ of the distribution, which correspond to deliveries before and after the mean gestational age at birth of singletons, should also correspond to those in twins. Data from the USA suggest that this is indeed the case: 18% of singletons and 18% of twins were delivered after 40 and 37 weeks, respectively. [3] It is expected that pathologies related to the period defined by the upper ‘tail’ in singletons will be at least similarly frequent in twins. Growth Normal twin growth patterns show accelerated growth before deceleration begins towards the end of gestation. Comparison between growth patterns of twins and singletons suggests that incremental growth reaches a plateau earlier in twin pregnancies. This pattern suggests that any additional week(s) beyond a, at about 37-38 week’s gestation does not significantly increase birth weight. Morbidity Luke et al. [4] compared total birth costs in twins and in carefully matched singleton controls to assess the overall morbidity associated with plurality and gestational age. Preterm births rather than plurality characterized the predominant cost factor. Compared with singletons, twins experienced increased morbidity and associated costs after 38 week’s gestation. Several studies stratify the frequency of cerebral palsy in twins versus singletons by gestational age. The most significant risk of cerebral palsy in all babies was prematurity. However, whereas the risk of cerebral palsy in singletons and in twins decreases steadily until 36-37 weeks, the risk of cerebral palsy in singletons continues to decrease but that for twins increases once again after 37 weeks’ gestation. [5] Mortality Minakami and Sato [6] as well as others, showed that the incidence of perinatal death in multifetal pregnancies (predominantly twins) gradually declines until 37 to 38 weeks' gestation and then increases again, as compared with 39 weeks' gestation in singletons. The lowest incidence of perinatal death seen at 38 weeks' gestation in multifetal pregnancies was similar to that seen at 43 weeks in singletons. These authors concluded that fetuses of multifetal pregnancies are at an increased risk of death after 3738 weeks. These lines of evidence are sufficient to indicate that “term” occurs earlier in twins than in singletons. Accordingly, limiting the estimated date of delivery to 37 - 38 weeks may be appropriate in twin pregnancies. It follows that there is some merit in delivering twins who completed 38 weeks. Regrettably, there are only few 64 Blickstein published series on this issue. One recent study [7] tried to determine the gestational age at delivery associated with the lowest rates of perinatal mortality, respiratory distress syndrome, and long hospital stays among twins. The nadirs of perinatal mortality rate, respiratory distress syndrome incidence, and long hospital stay rate were seen at delivery dates of 39, 40, and 38 weeks' gestation, respectively. Pairs delivered vaginally without the induction of labor had the lowest perinatal mortality rate at 37 weeks' gestation. The authors concluded that induction of labor should be routinely considered for twins at 37 to 38 weeks' gestation. The overdistended uterus of twin gestation, however, is a relative contraindication for labor induction and therefore pregnancy is often terminated by cesarean birth. Recent studies have suggested that pre-induction ripening of the cervix is both effective and safe. [8-9] Unfavorable cervical conditions seem to be no longer an obstacle for vaginal birth in appropriate candidates. Nevertheless, labor in twin gestations that was induced, rather than spontaneous, required more time, more oxytocin, and was associated with a higher cesarean delivery rate. [10] It should be stressed that if 38 weeks or more for twins represent “post-term”, it does not mean that 36-37 weeks are equivalent to term in singletons. Although twins probably gain neurological maturity at this age, the risk of respiratory distress is not eliminated. Indeed, twins with respiratory disorders were more likely to have been delivered by cesarean section between 36 and 38 weeks' gestation. [11] The authors concluded that without a clear indication for delivery, waiting until labor or until after 38 weeks' gestation should be considered. How to Deliver Twins? Assuming that about half of the twins are delivered anyway by cesarean section, the contribution of twins to the overall cesarean rate can be estimated. With increasing cesarean rates, the contribution of twin to that rate becomes negligible. Performing a cesarean for all twins is expected to increase the overall rate by 10% in a service with an overall 10% cesarean rate but will add only 3.3% to a service with an overall rate of 30%. [2] Any decision about the mode of delivery that includes probability estimation is prone to serious confounding. An incomplete list of confounding variables in deciding about the mode of delivery in twins is shown in Table 1. It seems that one may find an indication for cesarean birth in almost every twin pregnancy. However, research has not quantified the attributed risk of most of the confounding variables listed in Table 1 and has taken the easy way, by focusing on presentation and size to deal with the optimal mode of twin birth. Vertex-vertex pairs are unanimously considered appropriate candidates for vaginal birth, with few exceptions related to size 64 Blickstein and/or gestational age. Vertex-nonvertex are considered conceivable candidates for vaginal birth, with many exceptions related to size and/or gestational age. [12] The common exceptions include small second-breech and dorso-inferior transverse lying second twin. These situations demonstrate the skills of the accoucheur to chose between external and internal versions. Bedside sonography will guide the operator and minimize needless blind ‘explorative’ interventions. Nonvertex-vertex and nonvertex-nonvertex are generally considered as an indication for abdominal birth. Recently, we conducted a multi-center collaboration of a large sample of breechfirst twin pairs delivered in 13 European centers. [13] The data indicated that when breech-first twin twins weighed <1500 g, there was a 2.4-times higher risk of depressed (<7) 5-min Apgar scores and a 9.5-times risk for neonatal mortality in vaginal compared with cesarean birth. However, cesarean birth did not improve outcome when breech-first twin weighed >1500 g. Importantly, no case of “locked twins” has been encountered. The simple rule-of-thumb indicates that the same criteria for singleton breech delivery should be applied for twin breech delivery. Conclusions The current epidemic dimensions of multiple pregnancies translate into true challenges for the obstetrician. Some are undoubtedly controversial and represent clinical dilemmas. There are several lines of evidence to suggest that twins should be delivered after completing 38 weeks. Yet, there is no prospective randomized trial that clearly demonstrate the anticipated beneficial effect. Similarly, there are several arguments to support the idea that all twins should be delivered by cesarean section, although there is little evidencebased support of this view. References 1. BLICKSTEIN I, KEITH LG. The epidemic of multiple pregnancies. Postgrad Obstet Gynecol; 21:1-7; 2001. 2. BLICKSTEIN I. Cesarean section for all twins ? J Perinat Med; 28: 169-174; 2000. 3. ALEXANDER GR, KOGAN M, MARTIN J, PAPIERNIK E. What are the fetal growth patterns of singletons, twins, and triplets in the United States? Clin Obstet Gynecol 41:114-25; 1998. 4. LUKE B, BIGGER HR, LEURGANS S, SIETSEMA D. The cost of prematurity: a case-control study of twins vs singletons. Am J Public Health 1996; 86:809-14. 5. BLICKSTEIN I. Cerebral palsy in multifetal pregnancies: Facts and hypotheses. In: Fetal medicine: The clinical care of the fetus as a patient. Chervenak FA, Kurjak A, (eds), Parthenon Publishing, Lancs, 1999: 368-73. 64 Blickstein 6. MINAKAMI H, SATO I. Reestimating date of delivery in multifetal pregnancies. JAMA 1996; 275: 1432-4. 7. HARTLEY RS, EMANUEL I, HITTI J. Perinatal mortality and neonatal morbidity rates among twin pairs at different gestational ages: optimal delivery timing at 37 to 38 weeks' gestation. Am J Obstet Gynecol 184:451-8; 2001. 8. MANOR M, BLICKSTEIN I, BEN-ARIE A, WEISSMAN A, HAGAY Z. Case series of labor induction in twin gestations with an intrauterine balloon catheter. Gynecol Obstet Invest 47:244-6; 1999 9. SIMOES T, CONDECO P, CAETANO P, DIAS E, NOGUEIRA I, GONCALVES A, FARELO A. Labor induction in twins. Isr J Obstet Gynecol 10:159-161; 1999. 10. CELNICK C, RAYBURN W, GONZALEZ JL, GILSON G, RAPPAPORT V, CURET L. Comparison of induced versus spontaneous labor in twins. Obstet Gyneco l97:S35; 2001. 11. CHASEN ST, MADDEN A, CHERVENAK FA. Cesarean delivery of twins and neonatal respiratory disorders. Am J Obstet Gynecol 181:1052-6; 1999. 12. BLICKSTEIN I, SCHWARTZ Z, LANCET M, BORENSTEIN R. Vaginal delivery of the second twin in breech presentation. Obstet Gynecol 69:774-6; 1987. 13. BLICKSTEIN I, GOLDMAN RD, KUPERMINC M. Delivery of breech-first twins: a multicenter retrospective study. Obstet Gynecol 95:37-43; 2000. Table 1. Confounding variables in the decision for a cesarean birth in twin pregnancies. 64 Blickstein