Drug Information Group
advertisement

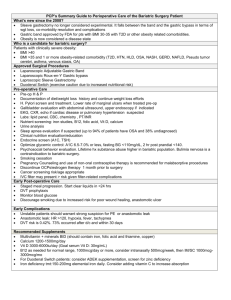
Frequently Asked Questions How is drug absorption altered by bariatric surgery Introduction With more than 30 million Americans considered clinically obese, obesity has become a very serious he contributes to approximately 6% of all health care expenditures.1 Aside from its financial impact, obesity of as many as 300,000 patients annually. The prevalence of obesity has greatly increased over the past related health effects, continues to grow.2 Obesity is associated with an increased risk for the developm cardiovascular disorders, and leads to poorer outcomes of co-morbid disease states. Due to the fact tha United States is obese, it may become more common for pharmacists to interact with morbidly obese pa procedure to facilitate weight loss. Although the number of bariatric surgical procedures performed cont addressing drug absorption and other medication concerns remains limited. It is essential that pharmaci order to guide medication therapy in this patient population. Treatment of obesity Approaches to weight management include diet, exercise, behavior modification, pharmacologic therapy treatment options may reduce weight, they do so at a modest rate of 2% to 10% after 1 year.3 Surgery is for obesity. However, since surgical procedures come with their own set of risks, this option is usually re defined as having a body mass index (BMI) > 40 kg/m2 or a BMI > 35 kg/m2 with comorbidity.2 Approxim surgery in the United States in 2008.4 This number is only expected to rise in the upcoming years. Surge stomach volume. However, by doing so, this causes a reduction in gastrointestinal (GI) surface area, wh alteration of the GI tract that occurs with bariatric surgery is likely to alter not only the absorption of vitam orally administered medications. As pharmacists, we rely on normal conditions for drug absorption; how drugs warrant special consideration. Types of bariatric surgical techniques Bariatric surgery can be described as surgical procedure that aims to limit caloric intake, decrease nutrie major types of bariatric surgery being used in the United States for the management of obesity.1 These gastroplasty, adjustable gastric banding, and conventional Roux-en-Y gastric bypass. Each of these pro malabsorption, restricting gastric volume, or a combination of these mechanisms.4 Each procedure com as unique drug administration concerns. Vertical-banded gastroplasty and adjustable gastric banding utilize restrictive (reduction of caloric intake vertical-banded gastroplasty, a portion of the stomach is stapled to form a small pouch, reducing stomac now usually done laparoscopically, involves inserting a silicone band lined with an inflatable balloon aro cm below the gastroesophageal junction.4 This creates a 30-mL upper gastric pouch, which limits food in controlled by adjusting the level of balloon inflation. This procedure is purely restrictive and thus, reduce procedures were historically performed in the United States; however, while they result in fewer postope replaced by combination restrictive and malabsorptive (reduction of the absorptive capacity of the intest The Roux-en-Y gastric bypass is most commonly performed in the United States and produces a more other two methods.2,5 This procedure uses a combined restrictive and malabsorptive approach to induce mL portion of the stomach is sectioned off in an effort to limit food intake. The small intestine is then cut intestine is connected to the pouch at the top of the stomach. The narrow opening to the small intestine a sensation of early satiety.6 By circumventing the lower portion of the stomach (90% to 95%) and much part of the proximal jejunum), the surface area for absorption is greatly decreased and malabsorption ca Drug absorption and bariatric surgery The mechanism of altered drug absorption depends partly on the type of procedure done-restrictive or m affected by drug disintegration and solubility and the surface area available for absorption, all of which c Disintegration of the dosage form is the first step needed for drug absorption. The smaller volume of the adequate tablet or capsule disintegration due to reduced gastric mixing.7 Solubility of a drug is depende pH are absorbed in the stomach, while those that are soluble in more basic environments are absorbed volume after bariatric surgery result in a decrease in gastric acid production and a higher pH compared may cause a decrease in the absorption of medications that rely on an acidic pH for solubility or absorpt stomach may further decrease drug bioavailability. These changes may be especially important for drug release formulations. Use of liquid formulations or chewing or crushing solid dosage forms (if appropriat Malabsorptive procedures bypass much of the small intestine.7 This technique not only decreases intes drugs and alters intestinal transit time. Mixing of highly lipid soluble drugs with bile acids may be reduce decreased absorption. In addition to drug absorption, drug distribution can also be affected following bariatric surgery.8 Obesity distribution include increased blood volume, cardiac output, lean body mass, organ size, and adipose m expected to change and, therefore, may necessitate drug dosing adjustments. Literature Summary Management of medications after bariatric surgery presents unique challenges and is often only guided surgery on drug absorption has not been widely investigated.4 The quality of data are often poor and pu bariatric surgery is usually limited to case reports and data from small studies. In addition, data from old techniques and procedures that are no longer in use. Table 1 summarizes recent case reports describin surgery. Table 1. Reports of Alterations in Drug Absorption Following Bariatric Surgery. Drug/usual absorption Bariatric procedure Study description and oral bioavailability O Antibiotics Amoxicillin9 Well absorbed; exact site of absorption not specified10 89% oral bioavailability12 Amoxicillin/clavulanate9 Well absorbed; exact site of absorption not specified10 Oral bioavailability unknown Nitrofurantoin9 Absorbed in proximal small intestine 87% oral bioavailability10 Antineoplastic agents Roux-en-Y gastric bypass Case report: 29-year-old pregnant female with history of bariatric surgery for morbid obesity given oral antibiotics a urinary tract infection. Despite sensitivity and compliance with 3 different regimens (amoxicillin, nitrofurantoin, and amoxicillin/clavulanate), infection progressed to pyelonephritis. Th tre fo W w Imatinib11 Likely absorbed in stomach proximal duodenum 98% oral bioavailability Sleeve gastrectomya Case report: 36-year-old obese female with chronic myeloid leukemia who received imatinib 400 mg/day for 4 years prior to sleeve gastrectomy. Plasma imatinib concentrations were measure before and on 4 occasions after the procedure. M co 40 va 65 62 da H co ye Th se un su im Tamoxifen12 Case series: 3 female patients with a history of bariatric surgery, treated with tamoxifen 20 mg/day for breast cancer. All patients had been taking tamoxifen for at least 3 months. Serum tamoxifen concentrations were measured to assess absorption. In co th (th m re di Fo 52 20 se (th ng Roux-en-Y gastric bypass Case report: 52-year-old male diagnosed with glioblastoma multiforme 3 months after gastric bypass. After a craniotomy, temozolomide was given at 75 mg/m2 with radiation, followed by a cycle of temolozomide monotherapy. Examination for persistent symptoms revealed tumor progression, and a second surgery was performed. P se te to lit Th te ad su Laparoscopic Rouxen-Y gastric bypass Prospective, nonrandomized pharmacokinetic study: 12 morbidly obese patients treated with atorvastatin S (A po pa Well absorbed from the GI tract; exact site of absorption not specified10 Oral bioavailability unknown Temozolomide13 Roux-en-Y gastric bypass Exact site of absorption not specified 100% oral bioavailability Cardiovascular agents Atorvastatin14 Absorbed in the proximal small intestine and metabolized by CYP enzymes in the small intestine 14% oral bioavailability15 before and after gastric bypass. de ba Th re su ef Immunosuppressive agents Mycophenolic acid6 Roux-en-Y gastric bypass Rapidly absorbed; exact site of absorption not specified16 94% oral bioavailability18 Pharmacokinetic study: 4 C dialysis and 2 renal transplant al recipients pa co Th m of ad im Sirolimus6 Majority of absorption occurs in proximal duodenum 27% oral bioavailability17 Tacrolimus6 Majority of absorption occurs in proximal duodenum 14% to 32% oral bioavailability18 Antithrombotic agents Warfarin19 Complete gastrectomy and Roux-en-Y Absorbed from stomach and proximal esophagojejunostomy duodenum 100% oral bioavailability20 a Procedure Case report: 71-year-old female with history of chronic atrial fibrillation with stable INR prior to surgery, requiring 5 to 6 mg/day. After surgery, patient experienced resistance to warfarin, requiring up to 20 mg/day in order to reach therapeutic INR. A w tit la pu on w IN fo where a portion of the stomach is removed surgically. Abbreviations: AUC, area under CYP, cytochrome; GI, gastrointestinal; INR, international normalized ratio; IV, intravenous; T max, tim In addition to the case reports described in Table 1, Padwal and colleagues published a systematic revi surgery.7 The authors identified 15 case reports and 11 controlled trials describing the effects of bariatric reports, evidence supporting decreased absorption was found for phenytoin, ethosuximide, rifampin, am and thyroxine. In general dose increases were needed, due to low serum concentrations of the drug. It i decreases in the drug dose after reversal of the bariatric procedure. Seaman and colleagues conducted an in vitro study to assess changes in the dissolution of various psy anxiolytics, and antipsychotics.21 The post-bypass test environment had a pH of 6.8 and was compared pH). Of 22 medications tested, 12 had different dissolution characteristics in the 2 environments. Dissolu compared with the control environment for amitriptyline, fluoxetine, paroxetine, sertraline, clonazepam, c and ziprasidone. Two medications-bupropion and lithium carbonate-had better dissolution in the test en noted two limitations to the trial: bioavailability was not studied and the tablets for the post-bypass enviro done for patients following bariatric surgery. Conclusion Many patients are able to discontinue medications for chronic conditions, such as diabetes and hyperten therapy is often needed for conditions unrelated to or not improved by weight loss. To better manage th changes in the anatomy and physiology of the GI tract following bariatric surgery. Consider crushing all release formulations to immediate-release dosage forms, when appropriate. Alternative dosage formula will circumvent the need for tablet or capsule dissolution should also be considered. Ultimately, frequent implemented in order to ensure correct dosing and to minimize side effects. References 1. Jacobs D and Robinson M. Morbid obesity and operations for morbid obesity. In: Zinner MJ and Ashl 11th ed. http://www.accesssurgery.com/content. aspx?aID=128173. 2. St. Peter J and Billington C. Obesity. In: DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey approach. 7th ed. New York, NY: Mc-Graw-Hill; 2008:2437-2453. 3. Salameh B, Khoukaz M, Bell R. Metabolic and nutritional changes after bariatric surgery. Expert Rev 4. Chan L. Drug therapy-related issues in patients who received bariatric surgery (part I). Pract Gastroe 5. Miller A and Smith K. Medication and nutrient administration considerations after bariatric surgery. Am 6. Rogers C. Alloway R, Alexander J, Cardi M, Trofe J, Vinks A. Pharmacokinetics of mycophenolic acid surgery in end-stage renal disease and transplant patients: a pilot study. Clin Transplant. 2008;22(3):28 7. Padwal R, Brocks D, Sharma A. A systematic review of drug absorption following bariatric surgery an 2010;11(1):41-50. 8. Macgregor A and Boggs L. Drug distribution in obesity and following bariatric surgery: A literature rev 9. Magee S, Shih G, Hume A. Malabsorption of oral antibiotics in pregnancy after gastric bypass surger 10. Micromedex® Healthcare Series [Internet database]. Greenwood Village, Colo: Thomson Reuters (H 11. Pavlovsky C, Egorin M, Shah D, Beumer J, Rogel S, Pavlovsky S. Imatinib mesylate pharmacokinet morbidly obese patients with chronic myeloid leukemia. Pharmacotherapy. 2009;29(9):1152-1156. 12. Wills S, Zekman R, Bestul D, Kuwajerwala N, Decker D. Tamoxifen malabsorption after Roux-en-Y the literature. Pharmacotherapy. 2010;30(2):86e-90e. 13. Park D, Shah D, Egorin M, Beumer J. Disposition of temozolomide in a patient with glioblastoma mu Neurooncol. 2009;93(2):279-283. 14. Skottheim I, Stormark K, Christensen H, et al. Significantly altered systemic exposure to atorvastatin obese patients. Clin Pharmacol Ther. 2009;86(3):311-318. 15. Lipitor. [package insert]. Dublin, Ireland; Pfizer Ireland Pharmaceuticals; 2009. 16. Cellcept. [package insert]. San Francisco, CA; Genentech USA Inc.; 2010. 17. Rapamune. [package insert]. Philadelphia, PA; Wyeth Pharmaceuticals Inc.; 2010. 18. Prograf. [package insert]. Deerfield, IL; Astellas Pharma US, Inc.; 2009. 19. Sobierag D, Wang F, Kirton O. Warfarin resistance after total gastrectomy and Roux-en-Y esophago 2008;28(12):1537-1541. 20. Coumadin. [package insert]. Princeton, NJ; Bristol-Myers Squibb; 2010. 21. Seaman J, Bowers ST, Dixon P, Schindler L. Dissolution of common psychiatric medications in a Ro 2005;46(3):250-253. Tatyana Lawrecki, Pharm D College of Pharmacy | Student Affairs | Academic Affairs | Continuing Education | Office of the Dean | Information Technology UIC Home | College Phonebook | Course Catalog | Site Map | Contact the College Copyright © 2007 The Board of Trustees of the University of Illinois | Web Privacy Notice