2014 AVW First Aid Policy - Ascot Vale West Primary School
advertisement

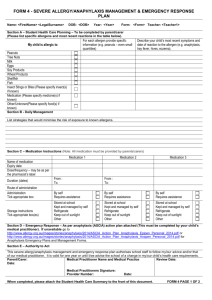
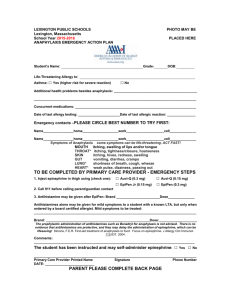
Ascot Vale West Primary School The School strives to ensure that our students will become responsible, motivated, life-long learners who can confidently face future challenges. First Aid Policy and Procedures 1. Introduction The school has procedures for supporting student health for students with identified health needs (see Care Arrangements for Ill Students Policy) and will provide a basic first aid response as set out in the procedure below to ill or injured students due to unforeseen circumstances and requiring emergency assistance. These procedures have been communicated to all staff and are available for reference from the school office. 2. First Aid Officers Consistent with the Department’s First Aid Policy and Procedures, the school will allocate staff member/s as First Aid Officer/s. The names and details of First Aid Officers, including their level of first aid and first aid expiry dates is kept on file in the office and displayed in the staffroom and First Aid room. 2.1 First Aid Officer Duties The First Aid Officer/s is required to undertake a coordinating role maintaining standard medical service provision, student medical records and parent notifications. Their specific duties include: Participating in the risk management process within the school as part of the school’s OHS team. This may include contributing to risk management solutions and providing feedback on injury reports and first aid register data to identify persistent or serious hazards Providing first aid emergency awareness training for staff including emergency notification processes, a list of responsible officers and provision of emergency phone numbers. Coordinating first aid duty rosters and maintaining first aid room and first aid kits Providing first aid services commensurate with competency and training. This may include all or some of emergency life support including response to life threatening conditions which may occur in the school (e.g. cardiac arrest or respiratory difficulties associated with asthma), management of severe bleeding, basic wound care, fractures, soft tissue injury Recording all first aid treatment. A copy of treatment provided shall be forwarded with the patient where further assistance is sought. The first aider should respect the confidential nature of any information given Providing input on first aid requirements for excursions and camps The First Aid Officer/s will be available at the school during normal working hours and at other times when authorised Department programs are being conducted Where possible, only staff with first aid qualifications will provide first aid. However, in an emergency other staff may be required to help within their level of competency. 3. Procedures for Medical Treatment In the event of a student requiring medical attention, an attempt will be made to contact the parents/guardians before calling for medical attention except in an extreme emergency In serious cases, parents/guardians will always be informed as quickly as possible of their child’s condition and of the actions taken by the school All accidents and injuries will be recorded on the Department’s injury management system on CASES21 A Record of First Aid Treatment will be kept in the Sick Bay and information recorded for all students treated in the Sick Bay. A proforma will be filled in and sent home with the student indicating date and time of attendance in the Sick Bay, the treatment given and the person administering the first aid. Duplicate copy is kept as a record It is the policy of the school that all injuries to the head are reported to a Leadership Team, Member in charge of First Aid and that parents/emergency contacts are contacted regarding the injury noting who was spoken to and the time of call First aid kits will be available for all groups that leave the school on excursions. The content of these kits will be dependent on the nature of the activities, the number of students and staff, and the location of the excursion Portable first aid kits will be available for staff on yard duty. These kits will contain: o a pair of single use plastic gloves o a bottle of sterile eye solution o gauze and band-aids o record book & pen. 4. Assessment and First Aid Treatment of an Asthma attack If a student develops signs of what appears to be an asthma attack, appropriate care must be given immediately. 4.1 Assessing the severity of an asthma attack Asthma attacks can be: Mild - this may involve coughing, a soft wheeze, minor difficulty in breathing and no difficulty speaking in sentences Moderate - this may involve a persistent cough, loud wheeze, obvious difficulty in breathing and ability to speak only in short sentences Severe - the student is often very distressed and anxious, gasping for breath, unable to speak more than a few words, pale and sweaty and may have blue lips. All students judged to be having a severe asthma attack require emergency medical assistance. Actions for severe asthma attack: Call an ambulance (dial 000) – state clearly that the student is having ‘breathing difficulties’ Notify the student’s emergency contact Follow the ‘4 Step Asthma First Aid Plan’ while waiting for the ambulance to arrive. The ambulance service will give priority to a person suffering extreme shortness of breath. Regardless of whether an attack of asthma has been assessed as mild, moderate or severe, Asthma First Aid (as detailed below) must commence immediately. The danger in any asthma situation is delay. Delay may increase the severity of the attack and ultimately risk the student’s life. 4.2 Asthma First Aid If the student has an Asthma Action Plan, follow the first aid procedure immediately. If no, Asthma Action Plan is available the steps outlined below should be taken immediately. The 4 Step Asthma First Aid Plan (displayed in Sick Bay and classrooms): Step 1 Sit the student down in as quiet an atmosphere as possible. Breathing is easier sitting rather than lying down. Be calm and reassuring. Do not leave the student alone. Step 2 Without delay give 4 separate puffs of a blue reliever medication (Airomir, Asmol, Epaq or Ventolin). The medication is best given one puff at a time via a spacer device. If a spacer device is not available, simply use the puffer on its own. Ask the person to take 4 breaths from the spacer after each puff of medication Step 3 Wait 4 minutes. If there is little or no improvement repeat steps 2 and 3. Step 4 If there is still little or no improvement; call an ambulance immediately (dial 000). State clearly that a student is having ‘breathing difficulties.’ Continuously repeat steps 2 and 3 while waiting for the ambulance. 5. Assessment and First Aid Treatment of Anaphylaxis What is anaphylaxis? Anaphylaxis is a severe, rapidly progressive allergic reaction that is potentially life threatening. Although allergic reactions are common in children, severe life threatening allergic reactions are uncommon and deaths are rare. However, deaths have occurred and anaphylaxis is therefore regarded as a medical emergency that requires a rapid response. Signs and symptoms The symptoms of a mild to moderate allergic reaction can include: o swelling of the lips, face and eyes o hives or welts o abdominal pain and/or vomiting. Symptoms of anaphylaxis (a severe allergic reaction) can include: o difficulty breathing or noisy breathing o swelling of the tongue o swelling/tightness in the throat o difficulty talking and/or a hoarse voice o wheezing or persistent coughing o loss of consciousness and/or collapse o young children may appear pale and floppy. Symptoms usually develop within 10 minutes to one hour of exposure to an allergen but can appear within a few minutes. The role and responsibilities of the principal The principal or nominee has overall responsibility for implementing strategies and processes for ensuring a safe and supporting environment for students at risk of anaphylaxis. The principal will: Actively seek information to identify students with severe life threatening allergies at enrolment Conduct a risk assessment of the potential for accidental exposure to allergens while the student is in the care of the school Meet with parents/carers to develop an Anaphylaxis Management Plan for the student. This includes documenting practical strategies for in-school and out-of-school settings to minimise the risk of exposure to allergens, and nominating staff who are responsible for their implementation Request that parents provide an ASCIA (Australasian Society of Clinical Immunology and Allergy) Action Plan that has been signed by the student’s medical practitioner and has an up to date photograph of the student Ensure that parents provide the student’s EpiPen® and that it is not out of date Ensure that staff obtain training in how to recognise and respond to an anaphylactic reaction, including administering an EpiPen® Develop a communication plan to raise student, staff and parent awareness about severe allergies and the school’s policies Provide information to all staff so that they are aware of students who are at risk of anaphylaxis, the student’s allergies, the school’s management strategies and first aid procedures. This can include providing copies or displaying the student’s ASCIA Action Plan in canteens, classrooms and staff rooms, noting privacy considerations Ensure that there are procedures in place for informing casual relief teachers of students at risk of anaphylaxis and the steps required for prevention and emergency response Ensure that any external canteen provider can demonstrate satisfactory training in the area of anaphylaxis and its implications on food handling practices Allocate time, such as during staff meetings, to discuss, practise and review the school’s management strategies for students at risk of anaphylaxis. Practise using the trainer EpiPen® regularly. Encourage ongoing communication between parents/carers and staff about the current status of the student’s allergies, the school’s policies and their implementation. Review the student’s Anaphylaxis Management Plan annually or if the student’s circumstances change, in consultation with parents. The role and responsibilities of all school staff who are responsible for the care of students at risk of anaphylaxis School staff who are responsible for the care of students at risk of anaphylaxis have a duty to take steps to protect students from risks of injury that are reasonably foreseeable. This may include administrators, canteen staff, casual relief staff, and volunteers. Members of staff are expected to: Know the identity of students who are at risk of anaphylaxis Understand the causes, symptoms, and treatment of anaphylaxis Obtain training in how to recognise and respond to an anaphylactic reaction, including administering an EpiPen® Know the school’s first aid emergency procedures and what your role is in relation to responding to an anaphylactic reaction Keep a copy of the student’s ASCIA Action Plan (or know where to find one quickly) and follow it in the event of an allergic reaction Know where the student’s EpiPen® is kept. Remember that the EpiPen® is designed so that anyone can administer it in an emergency Know and follow the prevention strategies in the student’s Anaphylaxis Management Plan Plan ahead for special class activities or special occasions such as excursions, incursions, sport days, camps and parties. Work with parents/carers to provide appropriate food for the student Be aware of the possibility of hidden allergens in foods and of traces of allergens when using items such as egg or milk cartons in art or cooking classes Be careful of the risk of cross-contamination when preparing, handling and displaying food. Make sure that tables and surfaces are wiped down regularly and that students wash their hands after handling food Raise student awareness about severe allergies and the importance of their role in fostering a school environment that is safe and supportive for their peers. Individual Anaphylaxis Management Plans Every student who has been diagnosed as at risk of anaphylaxis will have an individual Anaphylaxis Management Plan. (see Care Arrangements for Ill Students Policy). The student’s Anaphylaxis Management Plan will clearly set out: the type of allergy or allergies the student’s emergency contact details practical strategies to minimise the risk of exposure to allergens for in-school and out of class settings, including: o during classroom activities o in canteens or during lunch or snack times o before and after school, in the yard and during breaks o for special events such as incursions, sport days or class parties o for excursions and camps the name of the person/s responsible for implementing the strategies information on where the EpiPen® will be stored. The Anaphylaxis Management Plan will also include an individual ASCIA Action Plan, which sets out the emergency procedures to be taken in the event of an allergic reaction. (ASCIA, the Australasian Society of Clinical Immunology and Allergy, is the peak body of immunologists and allergists in Australia). It is the responsibility of parents/carers to complete an ASCIA Action Plan, in consultation with their child’s medical practitioner, and provide a copy to the school. The ASCIA Action Plan must be signed by the student’s medical practitioner, and have an up to date photograph of the student. As a student’s allergies may change with time, our school will ensure that the student’s Anaphylaxis Management Plan and ASCIA Action Plan are kept current and reviewed annually with the student’s parents/carers. When reviewed, parents will be expected to provide an updated photo of the child for the ASCIA Action Plan. See Appendix D: Anaphylaxis Management Plan Cover Sheet 6. First Aid Kit Contents Consistent with the Department’s First Aid Policy and Procedures the school will maintain a First Aid Kit that includes the following items: an up-to-date first aid book – examples include: o First aid: Responding to Emergencies, Australian Red Cross o Australian First Aid, St John Ambulance Australia (current edition) o Staying Alive, St John Ambulance Australia, (current edition) wound cleaning equipment o gauze swabs: 100 of 7.5 cm x 7.5 cm divided into small individual packets of five o sterile saline ampoules: 12 x 15 ml and 12 x 30 ml o disposable towels for cleaning dirt from skin surrounding a wound wound dressing equipment o sterile, non-adhesive dressings, individually packed: eight 5 cm x 5 cm, four 7.5 m x 7.5 m, four 10 cm x 10 cm for larger wounds o combine pads: twelve 10 cm x 10 cm for bleeding wounds o non-allergenic plain adhesive strips, without antiseptic on the dressing, for smaller cuts and grazes o steri-strips for holding deep cuts together in preparation for stitching o non-allergenic paper type tape, width 2.5 cm–5 cm, for attaching dressings o conforming bandages for attaching dressings in the absence of tape or in the case of extremely sensitive skin o six sterile eye pads, individually packed bandages o triangular bandages, for slings, pads for bleeding or attaching dressings, splints, etc o conforming bandages: two of 2.5 cm, two of 5 cm, six of 7.5 cm and two of 10 cm – these may be used to hold dressings in place or for support in the case of soft tissue injuries lotions and ointments o cuts and abrasions should be cleaned initially under running water followed by deeper and more serious wounds being cleaned with sterile saline prior to dressing. Antiseptics are not recommended o any sun screen, with a sun protection factor of approximately 15+ o single use sterile saline ampoules for the irrigation of eyes o creams and lotions, other than those in aqueous or gel form, are not recommended in the first aid treatment of wounds or burns o asthma equipment (which should be in all portable kits) o blue reliever puffer (e.g. Ventolin) that is in date o spacer device o alcohol wipes Other equipment may include: single use gloves – these are essential for all kits and should be available for teachers to carry with them, particularly while on yard duty blood spill kits vomit spill kits medicine measure for use with prescribed medications are brought by children on a needs basis disposable cups one pair of scissors (medium size) disposable splinter probes and a sharps container for waste disposable hand towels pen-like torch, to measure eye-pupil reaction two gel packs, kept in the refrigerator, for sprains, strains and bruises or disposable ice packs for portable kits adhesive sanitary pads, as a backup for personal supplies flexible ‘sam’ splints for fractured limbs (in case of ambulance delay) additional 7.5 m conforming bandages and safety pins to attach splints blanket and sheet, including a thermal accident blanket for portable kits germicidal soap and nail brush for hand-cleaning only one box of paper tissues paper towel for wiping up blood spills in conjunction with blood spill kit single use plastic rubbish bags that can be sealed, for used swabs and a separate waste disposal bin suitable for taking biohazard waste (note: Biohazard waste should be burnt and there are several companies that will handle bulk biohazard waste) ice cream containers or emesis bags for vomit. 7. Emergency Telephone Numbers Poisons Information Service Ambulance 13 11 26 000 This policy was ratified by school council Oct 2014