Appendix 1 The objective of the “Randomized controlled trial to
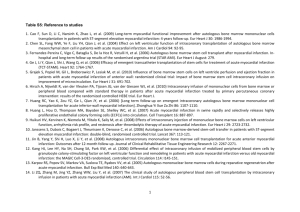
advertisement

Appendix 1 The objective of the “Randomized controlled trial to compare the effects of single versus repeated intracoronary application of autologous bone marrow-derived progenitor cells on allcause and SHFM-predicted mortality in patients with chronic post-infarction heart failure” (REpetitive Progenitor cEll therapy in Advanced chronic hearT failure -REPEAT trial) trial is to investigate whether mononuclear cells, isolated from bone marrow the same way as in REPAIR-AMI 1, may improve clinical outcome when reinfused into the previous-infarctrelated coronary artery. Study design The REPEAT trial (NCT 01693042) is an investigator-initiated, open-label, randomized, controlled, multicenter clinical trial. The design of the study is shown in Figure 1. A total of 668 patients who suffer from chronic post-infarction heart failure due to an at least 3 months old myocardial infarction will be randomized to receive either one or two sequential applications of mononuclear cells within 4 months via intracoronary infusion into the open previously infarct-related artery. End points The single primary endpoint of the REPEAT trial is all-cause mortality at 2 years after the first intracoronary application of autologous BM-MNC. All secondary endpoints are listed in supplemental table 2. Of note, a secondary endpoint is the comparison between observed and SHFM-predicted mortality in the repeated treatment group. Patient population Patients with chronic post-infarction heart failure are eligible for trial inclusion if their most recent myocardial infarction is older than 3 months, they have an open coronary vessel or bypass supplying the most recent infarcted area, are stable functional NYHA class equal or greater than 2 under constant optimal heart failure-directed medication with a LV ejection fraction equal or smaller than 45% on routine echocardiography, and are above 18 years old with a life expectancy of at least 1 year. In addition, participants have to provide written informed consent. Major exclusion criteria are clinically significant renal failure and hemodynamically relevant valvular disease. The complete list of exclusion criteria are provided in supplemental table 2. 1 Bone marrow aspiration and cell preparation Bone marrow aspiration will be performed the same way as in the REPAIR-AMI 1 and BAMI trial. Randomization Patients will be randomized centrally by the cell processing center in a 1:1 ratio to the single or repeated treatment group, by means of a sealed randomization list. Intracoronary cell application Intracoronary infusion of the isolated autologous bone marrow-derived cells will be performed within 48 hours from the time of bone marrow aspiration, in order to ensure full functionality of the isolated cells. Cells will be infused using the “stop-flow-techniques” with either a conventional over-the-wire balloon or a specific cell infusion catheter. The final cell product suspension will be infused in three portions of 3.3 ml each, with 3 min occlusion time for each infusion. After the first portion of the cell suspension has been administered, the balloon will be deflated for 3 min before reocclusion, to avoid extensive ischemia. Balloon occlusion is intended to enhance the adhesion and migration of the infused cells in the infarct area. Importantly, only the use of bivalirudin is allowed for anticoagulation during the cell infusion catheter procedure 2. Statistics The primary statistical aim is to compare survival until 2 years follow-up between the two treatment arms with Kaplan-Meier analysis and a two-sided log-rank test. The global significance level is set to =5%. For sample size calculation, we assume survival rates of 85 and 92%, respectively, after 2 years and a lost-to-follow-up rate of 5%, according to the registry data (see above). Applying a group sequential Wang and Tsiatis design with boundary shape parameter Delta=0.3, we need 334 patients in each treatment arm and have to include n=668 patients overall to achieve a statistical power of 80% when comparing treatment arms. The log-rank test of the final analysis will be performed at a two-sided significance level =4.34%. This corresponds to a critical bound of the log-rank test statistic of 2.021. A global significance level of 5% is assured by this procedure. 2 References 1. Schächinger V, Erbs S, Elsässer A, Haberbosch W, Hambrecht R, Holschermann H, Yu J, Corti R, Mathey DG, Hamm CW, Süselbeck T, Assmus B, Tonn T, Dimmeler S, Zeiher AM. Intracoronary bone marrow-derived progenitor cells in acute myocardial infarction. N Engl J Med 2006;355(12):1210-21. 2. Seeger FH, Rasper T, Fischer A, Muhly-Reinholz M, Hergenreider E, Leistner DM, Sommer K, Manavski Y, Henschler R, Chavakis E, Assmus B, Zeiher AM, Dimmeler S. Heparin disrupts the CXCR4/SDF-1 axis and impairs the functional capacity of bone marrowderived mononuclear cells used for cardiovascular repair. Circ Res 2012;111(7):854-62. Appendix Table 1 Secondary efficacy endpoints Comparison between observed and SHFM-predicted mortality in the repeated treatment group Comparison between the 2 treatment groups at 2-year and 5-year follow-up Cardiac mortality, cardiovascular mortality Rehospitalization for heart failure Ischemic cardiac events (STEMI, NSTEMI, ACS) Coronary revascularisations (PCI / CABG) Heart transplantation, Assist-device implantation New resynchronization therapy, ICD implantation NYHA-Status, NT-proBNP serum levels Minnesota Living with Heart Failure Questionnaire Prespecified combined clinical endpoints: o Death and rehospitalisation for heart failure o Cardiac Death and rehospitalisation for heart failure o Cardiac and Cardiovascular Death and infarction and rehospitalisation for heart failure o Death and myocardial infarction o Death and myocardial rehospitalisation for heart failure o Secondary safety endpoints Death and any cardiovascular event All in-hospital events (during hospitalization for cell therapy) Life-threatening arrhythmias (sustained ventricular tachycardia; ventricular fibrillation and cardiopulmonary resuscitation) Any new malignant disease 3 Bleeding events Safety of intracoronary application of autologous bone marrow-derived cells (procedural complications, adverse events at 30 days, SAEs at 4 months after each cell application) Appendix Table 2 Exclusion criteria Non-ischemic cardiomyopathy Foreseeable necessity for revascularization in other vessel than the infarct vessel at the time of study therapy Hemodynamic relevant severe valvular disease / indication for operative / interventional revision Heart failure with preserved ejection fraction (diastolic heart failure), LVEF > 45% Unstable Angina Severe peripheral artery occlusive disease (≥ Fontaine stadium III) Active infection (C-reactive protein > 10 mg/dl), any chronic inflammatory disease, Neoplastic disease without documented remission in the last 5 years Stroke ≤ 3 months Impaired renal function (Serum creatinine > 2,5 mg/dl or eGFR [MDRD] ≤ 30 ml/min) at the time of study inclusion Relevant liver disease (GOT > 2x upper normal limit, spontaneous INR > 1,5). Diseases of hematopoetic system, anemia (Hemoglobin < 8.5 mg/dl), thrombocytopenia < 100.000/µl) Splenomegaly Allergy or intolerance of clopidogrel, prasugrel, ticagrelor, heparin, bivalirudin History of bleeding disorder Gastrointestinal bleeding ≤ 3 months Major surgery or trauma ≤ 3 months Uncontrolled hypertension Pregnancy, lactation period Mental retardation Previous cardiac cell therapy within last 12 months Participation in another clinical trial ≤ 30 days 4 REPEAT Flowchart 5