Pap SOAP Note Name: Jane Doe DOB: xx-xx
advertisement
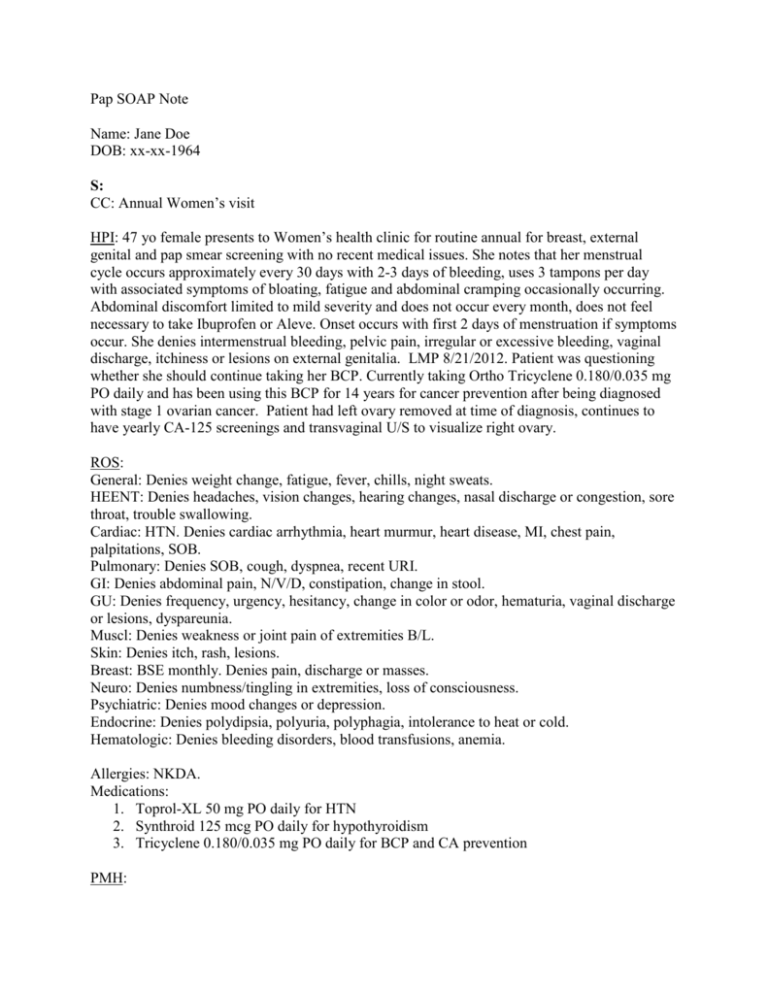
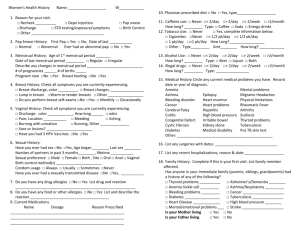
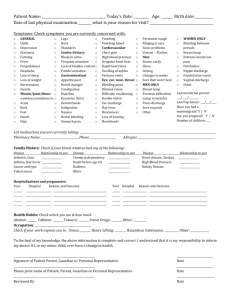
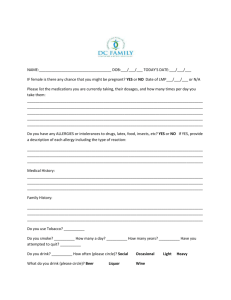
Pap SOAP Note Name: Jane Doe DOB: xx-xx-1964 S: CC: Annual Women’s visit HPI: 47 yo female presents to Women’s health clinic for routine annual for breast, external genital and pap smear screening with no recent medical issues. She notes that her menstrual cycle occurs approximately every 30 days with 2-3 days of bleeding, uses 3 tampons per day with associated symptoms of bloating, fatigue and abdominal cramping occasionally occurring. Abdominal discomfort limited to mild severity and does not occur every month, does not feel necessary to take Ibuprofen or Aleve. Onset occurs with first 2 days of menstruation if symptoms occur. She denies intermenstrual bleeding, pelvic pain, irregular or excessive bleeding, vaginal discharge, itchiness or lesions on external genitalia. LMP 8/21/2012. Patient was questioning whether she should continue taking her BCP. Currently taking Ortho Tricyclene 0.180/0.035 mg PO daily and has been using this BCP for 14 years for cancer prevention after being diagnosed with stage 1 ovarian cancer. Patient had left ovary removed at time of diagnosis, continues to have yearly CA-125 screenings and transvaginal U/S to visualize right ovary. ROS: General: Denies weight change, fatigue, fever, chills, night sweats. HEENT: Denies headaches, vision changes, hearing changes, nasal discharge or congestion, sore throat, trouble swallowing. Cardiac: HTN. Denies cardiac arrhythmia, heart murmur, heart disease, MI, chest pain, palpitations, SOB. Pulmonary: Denies SOB, cough, dyspnea, recent URI. GI: Denies abdominal pain, N/V/D, constipation, change in stool. GU: Denies frequency, urgency, hesitancy, change in color or odor, hematuria, vaginal discharge or lesions, dyspareunia. Muscl: Denies weakness or joint pain of extremities B/L. Skin: Denies itch, rash, lesions. Breast: BSE monthly. Denies pain, discharge or masses. Neuro: Denies numbness/tingling in extremities, loss of consciousness. Psychiatric: Denies mood changes or depression. Endocrine: Denies polydipsia, polyuria, polyphagia, intolerance to heat or cold. Hematologic: Denies bleeding disorders, blood transfusions, anemia. Allergies: NKDA. Medications: 1. Toprol-XL 50 mg PO daily for HTN 2. Synthroid 125 mcg PO daily for hypothyroidism 3. Tricyclene 0.180/0.035 mg PO daily for BCP and CA prevention PMH: Menstrual history: LMP 8/21/2012, menstruation started at age 14. OB history: 2-0-2-2. Vaginal deliveries =2, cesarean section deliveries = 0. 2 daughters ages 17 and 18. Gynecological history: Last pap smear 7/20/2011. Last MMG 10/14/2011. Patient was diagnosed with stage 1 ovarian cancer in 9/1998. General History: Hypothyroidism, HTN, 2 miscarriages. Surgical History: Serous cystadenocarcinoma removal, pelvic and para-aortic lymphatic dissection and omental biopsy in 1998. Cervical cerclage in 1995. Genetic history: BRCA 1 & 2 negative Family History: Mother had kidney CA, both parents have HTN. Denies heart disease, MI, CVA, seizures. Social History: Patient is married, employed as high school teacher, never smoked, no alcohol or drug use, exercises sporadically. Sexual history: onset of coitus age 19, 1 partner, sexually active 6x/month. O: Physical Exam: Vitals: 130/82 BP, 66 pulse, 98.2 F, 5’5”, 144 lbs, 98% PO2 on room air. General: Well-nourished, well-developed individual, NAD. Skin: no rashes or lesions. HEENT: Normocephalic, white sclera, no conjunctival injection, PERRLA, pearly gray TM B/L, no nasal discharge, nasal septum midline, throat without lesions or exudates, MMM, clean dentition. Neck: Trachea midline. Thyroid midline, equally rises and falls, no enlargement, asymmetry, masses, nodules or tenderness appreciated on palpation. Cardiac: RRR, S1 and S2 identified, no M/G/R or S3, S4 on auscultation. Pulmonary: Symmetric chest lift, CTA B/L, no wheezes, rhonchi, rales on auscultation. GI: Active bowel sounds x4 quadrants, soft, NTND abdomen, mildly obese, no hepatosplenomegaly. Breast/Genital: Breast – Medium sized breasts, pendulus, nipples symmetrical, No skin changes, nipple discharge, retraction, lesions, masses or tenderness appreciated on exam. No lympadenopathy in axillary region bilaterally. External genitalia – Mons pubis – triangular patch of dark hair, no lesions. Vulva/Labia Majora – no rashes, lesions, irritation or piercings. Bartholin glands – no masses, inflammation, or discharge. Skene glands – no masses, inflammation, or discharge. Clitoris – no enlargement, piercings, non-tender. Urethra – No prolapsed, discharge, non-tender. Bladder – unappreciated on exam. Vagina – Rugated pink vaginal walls, no lesions, no discharge or blood, strong muscular tone. Cervix – Squamocolumnar junction identified on exam, 12 cm in diameter. No erythema, discharge, or lesions appreciated on exam. Uterus – Small, midline, firm, smooth, mobile, non-tender with movement. Adnexae – small, no masses, non-tender bilaterally. Rectal – patient deferred rectal exam at this time. Lymphatics: No pre/post-auricular, ant/posterior cervical chain, occipital, sub-mandibular, submental, supraclavicular, infraclavicular, axillary, inguinal node lymphadenopathy. Extremities: no deformities, ambulates with no weakness bilaterally on inspection, no varicosities, no cyanosis or edema. Neuro: AAOx3, pleasant affect. Medical procedure: Patient prepared for screening Pap smear. Previous pap screening had no significant findings on 7/20/2011. With female chaperone present, patient verbally consented to gynecological exam. Patient educated about mild spotting of blood and vaginal discomfort after procedure for 1-2 days. Advised to wear panty liner for spotting. After consent, patient placed in lithotomy position. External genitalia was inspected with no lesions or rash noted. Lubricated plastic speculum was inserted into female vagina to visualize vaginal wall and cervix. Cervix was visualized, no discoloration, lesions, infection, or discharge noted on exam. Approximate size of squamocolumnar junction 12 mm in diameter. Brush was used to remove cervical cell sample from squamocolumnar junction. Another sample was taken of vaginal wall with spatula. Samples were placed in separate specimen containers and sent to lab for further microscopic evaluation and culture. Bimanual exam was then performed, uterus was found to be midline, freely mobile, smooth, non-tender, no adnexal masses or tenderness. Procedure did not detect any palpable masses or tenderness on examination. A: Diagnosis: Annual woman’s health exam and gynecological exam P: 1. Diagnostic labs & studies a. Orders placed for Pap smear screening. i. Vaginal culture. ii. Thin Prep Pap test. b. Patient scheduled for Mammogram on 10/16/2012. 2. Treatment/Medications a. Continue Toprol-XL 50 mg PO daily, Synthroid 125 mcg PO daily as directed by PCP. i. Side effects of Toprol-XL – hypotension, dizziness, diarrhea, constipation. ii. Side effects of Synthroid – weight loss, insomnia, increased appetite, hypertension. b. Continue Ortho Tricyclene 0.180/0.035 mg PO daily for BCP and CA prevention i. Side effects – nausea, vomiting, weight change, intermenstrual bleeding, breast tenderness, allergic reaction. c. Recommended patient consider changing type of birth control to IUD to reduce bleeding during menstrual cycles i. Side effects – intermenstral bleeding, perforation of uterus from IUD device, no protection against STIs, expulsion from uterus which allows pregnancy to occur. 3. Patient Education a. Discussed several types of IUD including Paraguard and Mirena. i. Benefits of IUDs 1. Educated patient that IUD would allow for 5 year birth control coverage using Mirena and 10 year coverage with ParaGard. ii. Risks of IUDs 1. Mirena – intermenstrual bleeding, perforation, expulsion. 2. ParaGard – may increase menstrual bleeding, abdominal cramps, intermenstrual bleeding. 3. Reminded patient that IUDs do not protect against STIs and HIV transmission. Recommend condom use if concerned with risk of STI or HIV. 4. Follow up: 1 month a. Will discuss decision to continue Ortho Tricyclene or discuss other option such as IUD. b. Will call patients with laboratory results from Pap smear. c. Patient is to call office with any pelvic pain, irregular bleeding, discharge or other issues or concerns. d. Patient advised if severe pain or significant bleeding go to emergency department. Alyson Wattai, PA-S