Ocular trauma fact sheet
advertisement
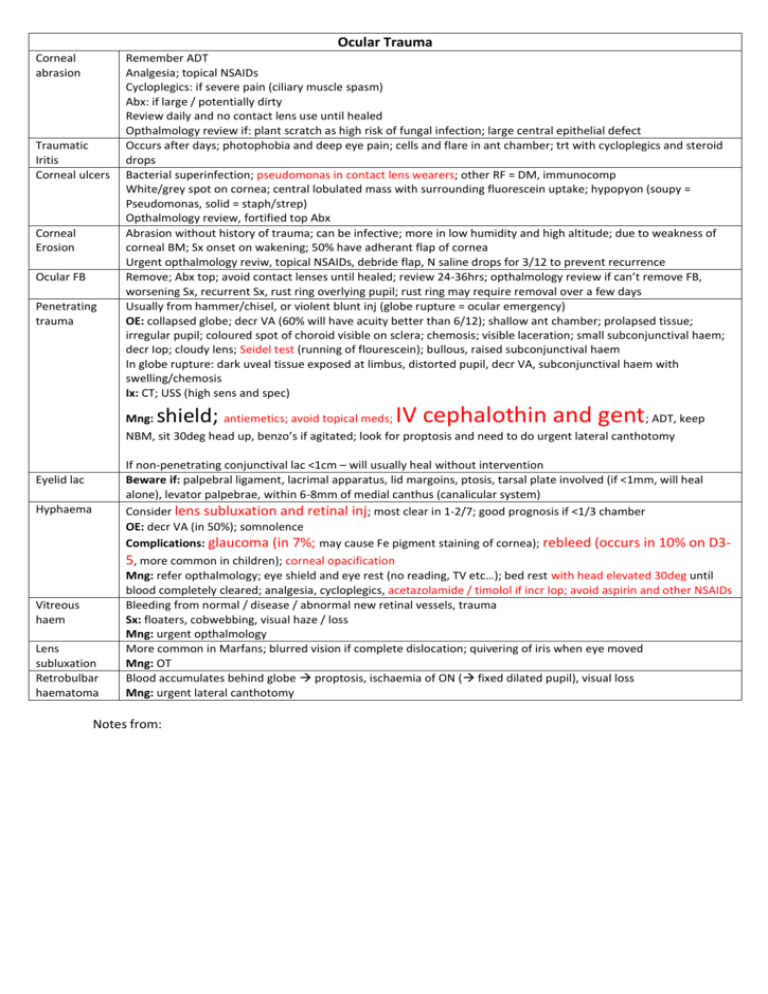
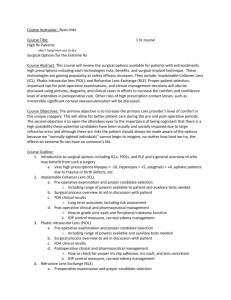
Ocular Trauma Corneal abrasion Traumatic Iritis Corneal ulcers Corneal Erosion Ocular FB Penetrating trauma Remember ADT Analgesia; topical NSAIDs Cycloplegics: if severe pain (ciliary muscle spasm) Abx: if large / potentially dirty Review daily and no contact lens use until healed Opthalmology review if: plant scratch as high risk of fungal infection; large central epithelial defect Occurs after days; photophobia and deep eye pain; cells and flare in ant chamber; trt with cycloplegics and steroid drops Bacterial superinfection; pseudomonas in contact lens wearers; other RF = DM, immunocomp White/grey spot on cornea; central lobulated mass with surrounding fluorescein uptake; hypopyon (soupy = Pseudomonas, solid = staph/strep) Opthalmology review, fortified top Abx Abrasion without history of trauma; can be infective; more in low humidity and high altitude; due to weakness of corneal BM; Sx onset on wakening; 50% have adherant flap of cornea Urgent opthalmology reviw, topical NSAIDs, debride flap, N saline drops for 3/12 to prevent recurrence Remove; Abx top; avoid contact lenses until healed; review 24-36hrs; opthalmology review if can’t remove FB, worsening Sx, recurrent Sx, rust ring overlying pupil; rust ring may require removal over a few days Usually from hammer/chisel, or violent blunt inj (globe rupture = ocular emergency) OE: collapsed globe; decr VA (60% will have acuity better than 6/12); shallow ant chamber; prolapsed tissue; irregular pupil; coloured spot of choroid visible on sclera; chemosis; visible laceration; small subconjunctival haem; decr Iop; cloudy lens; Seidel test (running of flourescein); bullous, raised subconjunctival haem In globe rupture: dark uveal tissue exposed at limbus, distorted pupil, decr VA, subconjunctival haem with swelling/chemosis Ix: CT; USS (high sens and spec) shield; IV cephalothin and gent Mng: antiemetics; avoid topical meds; ; ADT, keep NBM, sit 30deg head up, benzo’s if agitated; look for proptosis and need to do urgent lateral canthotomy Eyelid lac Hyphaema Vitreous haem Lens subluxation Retrobulbar haematoma If non-penetrating conjunctival lac <1cm – will usually heal without intervention Beware if: palpebral ligament, lacrimal apparatus, lid margoins, ptosis, tarsal plate involved (if <1mm, will heal alone), levator palpebrae, within 6-8mm of medial canthus (canalicular system) Consider lens subluxation and retinal inj; most clear in 1-2/7; good prognosis if <1/3 chamber OE: decr VA (in 50%); somnolence Complications: glaucoma (in 7%; may cause Fe pigment staining of cornea); rebleed (occurs in 10% on D35, more common in children); corneal opacification Mng: refer opthalmology; eye shield and eye rest (no reading, TV etc…); bed rest with head elevated 30deg until blood completely cleared; analgesia, cycloplegics, acetazolamide / timolol if incr Iop; avoid aspirin and other NSAIDs Bleeding from normal / disease / abnormal new retinal vessels, trauma Sx: floaters, cobwebbing, visual haze / loss Mng: urgent opthalmology More common in Marfans; blurred vision if complete dislocation; quivering of iris when eye moved Mng: OT Blood accumulates behind globe proptosis, ischaemia of ON ( fixed dilated pupil), visual loss Mng: urgent lateral canthotomy Notes from: