SC AHEC CE Council - University of South Carolina School of
advertisement

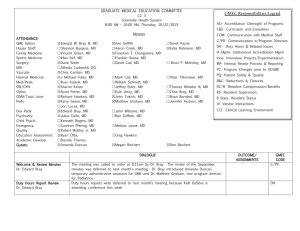
GRADUATE MEDICAL EDUCATION COMMITTEE GMEC Responsibilities Legend CC 3 Greenville Memorial Hospital 8:09 AM – 10:20 AM, Thursday, 1/23/2014 Minutes ATTENDANCE: GME Admin: Family Medicine: Internal Medicine: Med/Peds: OB/GYN: Ortho: Peds: Psychiatry: Surgery: MIS: Vascular: Dev Peds: Sports Medicine: Emergency: House Staff: Quality: Academic Development: Guest: ☒Edward W. Bray III, MD ☒Bruce Hanlin, MD ☒J. Michael Fuller, MD ☒Russell Kolarik, MD ☒David Forstein, DO ☒Scott Porter, MD ☒Kerry Sease, MD ☒Julius Earle Jr., MD ☒Dane Smith, MD ☐William Cobb IV, MD ☒Chris Carsten, MD ☒Desmond Kelly, MD ☒Kyle Cassas, MD ☐Melissa Janse, MD ☐Lyle Jackson, MD ☐Robert Mobley Jr, MD ☐Brenda Thames ☒Karin Matheson ☒Tom Blackwell, MD ☒Erik Buzby, MD ☒Jim Freeman ☐Sean Bryan, MD ☒Ann Griffith ☐Sharon Keiser, MD ☒Kyle Jeray, MD ☒Kenneth Rogers, MD ☒David Cull, MD ☒Alfie Carbonell, MD ☐Joshua Knott, MD ☐Lauren Leffler, MD ☒Jay Crockett, MD ☐James Davis, MD ☒Kitty Wolcott ☒Marty Lutz, MD ☒Charles Marguet, MD DIALOGUE Welcome & Review Minutes Dr. Edward Bray AO - Accreditation Oversight of Programs C&E – Curriculum and Evaluation Com – Communication with Medical Staff C/PD – Communication w/Program Directors DH – Duty Hours and Related Issues IA Mgmt –Institutional Accreditation Mgmt. Inno – Innovative Projects/Experimentation IRP – Internal Review Process & Reporting PC – Program Changes prior to ACGME PQ – Patient Safety and Quality R & C - Reductions & Closures RC/B – Resident Compensation/Benefits RS – Resident Supervision R Stats – Resident Status VI – Vendor Interactions Dr. Edward Bray called the meeting to order and minutes were approved. OUTCOME/ ASSIGNMENTS Minutes were approved GMEC CODE IA Mgmt AO ACGME Communications CLER Moment Dr. Edward Bray GME Expansion Reviews Dr. Edward Bray CLER Debrief & Oral Report Dr. Bray reported that the CLER field officers gave us “significant kudos” and were very impressed with our faculty, nursing staff, residents & PDs. The meeting went better than he expected, based on the field officer’s statement that “CEO types don’t accept what we have to say.” The final meeting went very well. They had a number of suggestions and reminded us that they weren’t here to tell us what to do but rather to look at our information, observe facts as they saw them, and compare them to what we said. Dr. Bray said that he has every reason to believe the written report will match the oral report, which was read to us from their computer. Field Officers commented that the Clinical University was very unique, it was notable that senior leadership used clinical learning environment beyond GME, and they planned to put that in report. They liked the Academic Council. Residents were very positive overall about their education and nurses were very supportive. 80-90% of residents reported safety. Most residents were not familiar with safety/quality terminology. Reporting for safety was consistent, but they noted that residents submitted very few event reports. Expectation going forward is documentation that residents and attendings are participating in event reporting. It was notable that M&M processes with VC of Quality. They commented that hand hygiene was priority. Most residents participate in QI projects. Most residents, PDs and faculty reported access to quality data. TOC 90% reported participating in hand off sessions and there is a culture of close supervision. On floors, there is no document for nurses to identify competency of residents. They work with residents based on familiarity with them. The same issue exists with attendings on floors. Dr. Hanlin noted that there is a list of privileges for attendings online. 30% of PD have seen problems with supervision in regard to patient care. No difficulty with duty hours. Professionalism – nearly all residents reported positive culture. Most nurses were very positive regarding professional interaction. FO reported that this was a very rewarding visit. They gave us an A+ for the logistics of the visit. Proposal Presentation / Q&A IA Mgmt AO IRP AO IA Mgmt 2 Kenneth Rogers, MD Child Psychiatry In SC there is critical need of child psychiatrists & adult psychiatrists. There should be twice the number in Greenville for the population. Having a fellowship makes a much more competitive general psychiatry program. Q: (Sease) Does it make it more attractive to have triple board option w/pediatrics? A: Only way to get triple board is to have all three in place first. Q: (Porter) How long after starting program would it take to be triple board certified, because that is very attractive? A: At least one class cycled through both programs. A. (Kelly) It would bring synergy with developmental peds fellowship. Faculty resources would be shared. Q: (Jeray) Is there an issue regarding accreditation with how long we’ve had the general psychiatry program? A: They function independently. Q: (Bray) How would you see this program progressing? Would you expect 50% of general psychiatry residents to transition to child psychiatry? Do they usually go into child psychiatry after 3rd year or do all four years of general and then move into fellowship? A: In Columbia, about 30% of residents have gone into child psych, which filled about half of their spots. I would expect 1-2 per year to go into child psych. Most will start child psych as PGY4. Department of Mental Health will fund half of the PGY5 spots each year. Q: (Forstein) How do you anticipate having time to be PD of this program along with other responsibilities? A: Goal is by 2017 we will have recruited someone in to be PD. Dr. Earle can assist with those duties. Q: (Freeman) Regarding accrediting an additional residency program when you’re halfway finished with the first year of another residency program: is that typical across the country? How dependent are you on the timeline that was projected? Are you as a chair comfortable and are you aware of other programs that have started a second residency program halfway through the first year of another program? Are there any significant physical facility adjustments that would need to be made to add the child psych program? A: No. The issue for us/timeline is how do you begin to prepare a system for population health management. There is no way of taking care of the number of kids out there. Without having a program in place to take care of. If we wait 4 years when we graduate first class, we’ll be behind the eight ball with regard to turning out more child psychiatrists to meet needs in area. We’ve expanded current facilities to W. Georgia Rd, so most second years wouldn’t be on GMMC. In renovation of MIP, there is additional space allocated for additional residents. Q: (Sease) Would anciliary providers need to be expanded (e.g. child psychologist, etc). Can be partnered with Developmental Peds. A: (Kelly) We’ve had those for years funded out of the psychology budget. Q: (Jeray) If child psychiatrists are in demand, why are most in practice focused on adults? A: Most see adults as well as children because treating children is a grueling process, so they want variety. Most programs around country are closing because psych reimbursements aren’t adequate so the system decides to discontinue the program. 3 Q: (Cull) Is there no operational challenge with adding a second accredited program? A: That is correct. 4 Jay Crockett, MD Colorectal Surgery The hospital’s mission is to teach innovatively. The community expects it. We need to keep focused on teaching in this institution. Our community is growing & aging. There are no colorectal training program in the Carolinas. There is one in Atlanta, a few in Florida, and none in Alabama. Why do we need to train more? Data supports that colorectal surgeons do surgery at lower cost with better mortality than general surgeons. There are only 56 programs in the country (approx. 100 positions/year). Patients want specialists and residents want specialized training. Residents look forward to being on colorectal service, and they have a history of keeping up with paperwork, etc. Why should we have a colorectal program over other programs? It’s our turn; we’ve been working on adding this program for three years. The program would be cheap – we only need one resident; everything else is already in place (no staff, no call rooms, etc). We already have two general surgery residents who want to start in the colorectal program. Q: (Freeman) Would you be required to have a PD & PC? A: Yes, I’ve been Associate PD for two years. Q: (Forstein) What is the impact of having residents working under fellows? A: We have the approval of the Department of General Surgery. Cull – When you bring a fellow onboard, it raises the quality of the General Surgery residency and the applicant pool. Q: (Forstein) Regarding academic productivity, how much is coming out of the colorectal division? A: Some members are more active than others (2-3 papers per year). A colorectal resident would be expected to add at least one paper per year. Q: In your application, several questions were answered with “TBD.” A: The comleted application is due in August. Q: (Porter) How many residents are on your service? Will the format be a mentorship model? A: We have two residents and six attendings. There will be no specific rotation; the resident will go to colorectal clinic and will be free to choose the cases that he wants each week. The resident will rotate through each faculty member a month at a time. Q: (Freeman) What percentage of time will you allot to Program Director’s duties? Reimbursement will come from teaching buy-back? A: I’ll set aside one afternoon a week for administrative duties. (Bray) If we add another resident to any department, it will change the balance from other departments. Cull – Regarding questions answered with “TBD,” the process of submitting the application has been going on for over two years. During that time, the process changed within hospital and residency requirements. The final modifications have been put on hold pending approval. Carbonell – This is exactly how they started their fellowship. There have been missed opportunity for trainees to have 1 in 7 cases covered and not have the ability to train someone. 5 Tom Blackwell, MD Marty Lutz, MD Erik Busby, MD Dates to Remember Dr. Edward Bray Adjourn Emergency Medicine Q: (Sease) I have concerns about space; we’re already limiting the number of peds residents rotating in the ER. Peds volume decreases after 2 AM. Are there enough cases to support overnight peds rotation? A: The current renovations will take out a wall to provide more space. Q: (Forstein) You have 28 hours/week for core faculty? A: Q: (Cull) – The case you’ve made is to add a residency program to add to the quality of the ER. That is the reverse of what seems typical. A: Q: (Jeray) How do you fund this? Why go for 10 at once? Residents slow down treatment. A: Residents aren’t in Emergency Department all year; they’re rotating on other services. They’re 24/7; not on call. In my years of experience, having residents in the ER does improve efficiency. They’re looking at volume and acuity in this geographic area. Q: (Cull) Could this program be based centrally in Greer so it’s not counted in our numbers/budget? A: It’s been part of the consideration. Urology Q: (Freeman) Where would program be located? What are physical facility needs? A: The program would be located in the Department of Surgery. Closed GMEC Review / Next Steps February 5, 2014, 7:00 PM – 8:00 PM Enhancing Your Medical Career with a Public Health Experience (location TBD) AAMC-CDC Cooperative Agreement Webinar Series http://tinyurl.com/orhrgfm February 3-5, 2014, 8:30 AM – 4:30 PM Professional Grant Development Workshop: CU/Fee $595 (866-704-7268) February 24, 2014 – Writing Your Specific Aims Workshop (866-704-7268) March 7, 2014, 12:00 PM – 2:00 PM - Ethics Faculty Training (HSEB Learning Studio 105) There being no further business, the meeting adjourned at 10:20 AM. Next Meeting: 2/27/2014; 8:00 AM in CC3. C/PD AO IA Mgmt wider or/Near Miss Reporting AO IA Mgmt C/PD 6