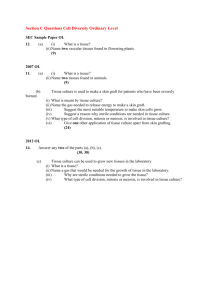
Case Study Questions and Answers - NC-NET
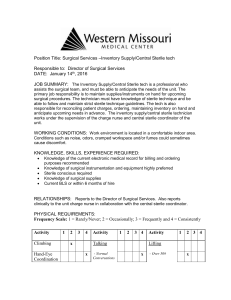
advertisement

Inflammation: Appendicitis Case Study Slide 4: What is the priority concern based on this information? Language barrier Cultural factors – Hispanic population Slide 8: Does this clinical picture coincide with a diagnosis of appendicitis? Are vital signs normal for a child this age? Why the changes? Yes They are elevated – he is in pain increasing BP, HR, & RR. Temperature & WBC are indicative of infection. Pain is consistent with appendicitis (initiates in the periumbilical region and then to McBurney’s point). Jose’s pain suddenly stops what is your priority? Notify the MD this is likely indicating a rupture of the appendix Slide 10: SBAR report from the ED nurse to the pediatric nurse to prepare Jose for surgery. How do you get the consent signed? By whom? In what language? Jose’s parents sign a consent that is in Spanish and English. The procedure description should be given to them using a medical translator. Often in these situations patients prefer to use family members to translate however that is inappropriate as they often do not know or understand fully the medical terminology and information is miscommunicated. Discuss issues/concerns regarding the use of translators – what is appropriate & what is not? Slide 12: What should be sent with Jose or communicated to the OR/holding room nurse? History & Phyiscal, CT abdomen result, laboratory results, nursing assessment, vital signs, consent, last pain medication given, last oral intake, need for a translator What is the role of the holding room/OR nurse? Verify patient identity, make sure IV is patent, answer any questions, explain to patient and family OR process, begin the antibiotics, obtain vital signs, verify correct documentation is on the chart/with the patient Slide 14: Have students role play a time out protocol. Correct patient identity, correct site, correct procedure to be performed verified by 2 members of the procedural team immediately prior to the surgery What type of anesthesia is used for this procedure? General anesthesia How should the anesthesia be administered to Jose? He should be given a preoperative sedative (the Versed) taken into the operating room suite and then administered IV inhaled or intravenous general anesthesia. If Jose did not already have an IV started then the inhaled anesthetic should be given first and then the IV line started (it is less traumatizing to a child this way). Why would other types be inappropriate? Jose is a child who would be frightened if he was awake or had memories of the procedure taking place. It is an abdominal procedure therefore local or regional anesthesia would be inappropriate. Slide 15: As the circulating nurse what would your duties include during this procedure? Non-sterile, assist with positioning, patient safety, verify consent, manage environment (team members, temperature, lighting, additional personnel – xray, lab), time-out procedure, documentation, gather additional supplies if needed, assist with the count at the end of the procedure, As the scrub nurse what would your duties include during this procedure? Review sterile technique Sterile, setting up sterile field, preparing sutures, assisting the surgeon/surgical assistants as necessary, count needles, sponges, instruments, label any specimens obtained What are the principles of surgical asepsis? All objects in contact with wound or within sterile field must be sterile Surgical team member gowns are sterile from chest to level of sterile field Only sterile drapes are used to create a sterile field Dispense items onto a sterile field maintaining sterility Scrubbed team members only may contact sterile field Sterile fields must be kept in view during movement Maintain a 1 ft distance from the sterile field to contamination during movement If a sterile barrier is breached the area is considered contaminated, if a drape tears it is unsterile & must be replaced Slide 17: The scoring method may have to be modified depending on the scoring system your textbook or facilities use. What are the priority assessments that should be completed in PACU? Airway, respiratory function, cardiovascular function, skin color, vital signs, level of consciousness, ability to respond, surgical site, monitoring lines (IV, catheter, etc.), pain, nausea/vomiting What patient/family teaching should occur at this time? Discussing what is being done for Jose, what the equipment is for (IV lines, monitors, etc), that he can have pain medication, when he will be able to leave PACU Slide 19: Based on this information is Jose ready to leave PACU? Yes, typically an Aldrete score of 8 or above is satisfactory for discharge. Aldrete looks at: Activing, Respiration, Circulation, Consciousness, & O2 Saturation – each category ranges from 0 to 2 with a total possible points value of 10 What information should be passed on in report from the PACU RN to the Pediatric RN? Have students utilize SBAR for the reporting procedure Patient information (Name, Age, MD), procedure, type of anesthesia, vital signs, history, allergies, medications (&time of admission) given in OR or PACU, blood loss, I&O’s, other pertinent data about the patients – in this case that neither he nor his parents speak English. Slide 22: What other assessment data should the nurse monitor? Why? Labs… Temperature, I&Os, Labs – WBC (infection) Later in postoperative period – elimination status, nutrition Priority nursing diagnoses Acute pain Dysfunctional GI motility Risk for infection (if not already present) Risk for fluid volume deficit Potential complications? How do you assess for them? Peritonitis – fever, abdominal rigidity, increased HR Abscess – fever, diarrhea, abdominal pain Ileus – bowel sounds If Jose’s appendix had ruptured how would his care be different – what additional assessment findings should be seen? He would likely have a drain in his abdomen to remove purulent drainage, an NGT could be in place to provide GI rest, his procedure couldn’t be done laparoscopically, his incision could be left open to allow for drainage & be a packed wound, he would have a fever, higher WBC count, increased pain, more significant changes in VS, dehydration could be present Slide 24: How is this postoperative teaching completed? Using a medical translator educate both Jose & his parents His diet is slowly progressed to prevent nausea/vomiting given the abdominal surgery, also the ambulation will help to stimulate the GI tract and will enable his diet to be advanced At Jose’s age teach him to use an IS (its like drinking through a straw) – for smaller child you can have them blow bubbles or pretend like they are blowing up a balloon to encourage them to take deep breaths Also teach him to splint his abdomen with a pillow Surgical dressing changes are typically done at physician preference Antibiotics are being continued because his appendix was significantly inflamed and they are to treat the infection that was likely present Have students practice/role play the teaching process with rationale to Jose & his parents. Anything else that needs to be taught?? Slide 26: What teaching needs to be included at discharge? New medications Activity – Showering, lifting, restrictions, Incision Care When to call the physician – fever, severe pain, foul drainage, excessive drainage, bleeding