supervised clinical attachment
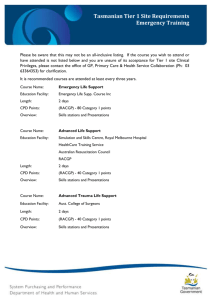
advertisement

Supervised Clinical Attachment Supervised Clinical Attachments (SCAs) are designed to provide an individualised learning experience and are an active, hands-on mode of learning, where the examples, scenarios and problems are real cases. Checklist The supervisor was a health professional with highly developed skills in a specific area Minimum of 10 hours of contact with the supervisor Name and details of the supervisor have been recorded Has between 3 and 5 clear and measurable learning outcomes At least 1 learning outcome addresses a systems based approach to patient safety Mapped to the Curriculum and Domains of general practice Individual quality improvement reflection response has been completed Further information Please contact your Program Coordinator in your local faculty or refer to the QI&CPD Program Handbook for further information regarding: supervised clinical attachments quality improvement RACGP Curriculum and Domains of general practice specific requirements training grants. Please email or mail the completed form to your state faculty QI&CPD unit. Address details can be found at Your RACGP or log in to My CPD on the RACGP website. SUPERVISED CLINICAL ATTACHMENT Name: RACGP QI&CPD number: Phone: Activity title: Total hours of educational content: Activity must be a minimum of 10 hours. Activity start date: Activity completion date: E-learning URL Delivery mode: Blended learning URL Face to face Please indicate the post code or mark if attended overseas Post code Overseas Other (please explain) Please attach any other information that is relevant to the assessment of the application ACTIVITY SUMMARY Describe your activity ACTIVITY MOTIVATION What motivated you to participate in this activity? Build on my existing knowledge and/or skills in this area This is a new area in my practice Near miss analysis Feedback from patients To meet legislative requirement Review of existing systems Improve safety strategies for staff and patients in practice Other (please explain) LEARNING OUTCOMES AND REFLECTION What did you hope to gain as a result of participating in this activity? List 3–5 learning outcomes that you want to take back to your practice as a result of this activity, with at least one that addresses systems based patient safety. Reflection: Reflecting on each learning outcome, what did you achieve, how will this impact on your practise? Systems based patient safety learning outcome SESSION SUMMARIES, or attach details of sessions Date Key features of presentation Key Learning ACTIVITY IMPROVEMENT In what ways could this activity have been improved? QUALITY IMPROVEMENT REFLECTION CHANGES IN YOUR PRACTICE What changes did you implement in your practice as a result of this activity? You may like to think about: Updated medical software to better manage patients’ records (referrals, recalls etc) Reviewed patients’ data using an audit tool Coordinated team care approach with a range of health, community and disability services to plan and facilitate optimal patient care (The RACGP Standards for general practices (4th edition) Standard 1.6 – criterion 1.6.1) Introduced clinical risk management systems to enhance the quality and safety of patient care (The RACGP Standards for general practices (4th edition) Standard 3.1 – criterion 3.1.2) MONITORING THESE CHANGES How do you monitor these changes? You may like to think about: Conduct regular practice staff meetings to gather information and updates on the outcomes of these changes Create a monitoring guideline (including a template) and staff roster for recording the outcomes of these changes Develop roles and responsibilities for practice staff that includes monitoring and recording the outcomes of these changes EVALUATION What evaluation process do you use to measure these changes? You may like to think about: Review the outcomes regularly against the set standards or targeted outcomes Seek and respond to patients’ feedback on their experience of our/my practice (The RACGP Standards for general practices (4th edition) Standard 2.1 – criterion 2.1.2) Measure changes using an appropriate checklist Compare ‘before and after’ patient data using audit tools Conduct regular updates and case-based discussions during team meeting CURRICULUM MATRIX Please mark the curriculum area(s) relevant to the activity mapped against the educational domain(s) Domains Curriculum Statements General statements Common training outcomes Philosophy and foundation of general practice People and their populations Aboriginal and Torres Strait Islander health Communication skills and the patient-doctor relationship Applied professional knowledge and skills Population health and the context of general practice Professional and ethical role Organisational and legal dimensions Aged care Children and young people’s health Disability Doctor’s health Genetics Men’s health Multicultural health Population health and public health Rural general practice Women’s health Domains Curriculum Statements Communication skills and the patient-doctor relationship Applied professional knowledge and skills Population health and the context of general practice Professional and ethical role Organisational and legal dimensions Applied professional knowledge and skills Population health and the context of general practice Professional and ethical role Organisational and legal dimensions Presentations Acute serious illness and trauma Chronic conditions Dermatology Drug and alcohol medicine Eye and ear medicine Mental health Musculoskeletal medicine Occupational medicine Oncology Pain management Palliative care Sexual health Sports medicine Domains Curriculum Statements Communication skills and the patient-doctor relationship Processes of general practice Critical thinking and research Undifferentiated conditions E-health Multidisciplinary care Integrative medicine Quality and safety Practice management Procedural skills Quality use of medicines Teaching, mentoring and leadership in general practice Other: please supply further information SPECIFIC REQUIREMENTS To be eligible as a Specific requirement Accredited Activity, content must represent more than 50% of the total activity Anaesthetics Focussed psychological strategy skills training Acupuncture Focussed psychological strategy CPD Breast medicine Mental health skills training Surgery Mental health CPD Cultural safety training Mental health core module Cultural awareness training Mental health clinical enhancement module Women’s health Radiology Please attach evidence documentation TRAINING GRANT ELIGIBILITY To be eligible for a training grant the activity must be a minimum of 6 hours Not applicable Anaesthetic grant Obstetric grant Surgery grant Emergency grant Please attach evidence documentation CPR CPR skill training must form a minimum of 1 hour of the education and be consistent with the ARC guidelines. Did the activity include CPR? Yes No Please attach evidence documentation GP DECLARATION I declare to the RACGP: I have completed this activity, and to the best of my knowledge it has been conducted and completed in accordance with the relevant RACGP QI&CPD Program requirements, educational standards and criteria. The information I have provided in this document is accurate and correct. I understand and acknowledge that the RACGP reserves the right to withdraw recognition of the activity if in the opinion of the RACGP the activity does not meet the QI&CPD program requirements, educational standards and criteria. Signed: Date: