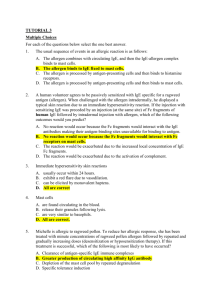
Immunology Ch 11 207-223 [4-20
advertisement
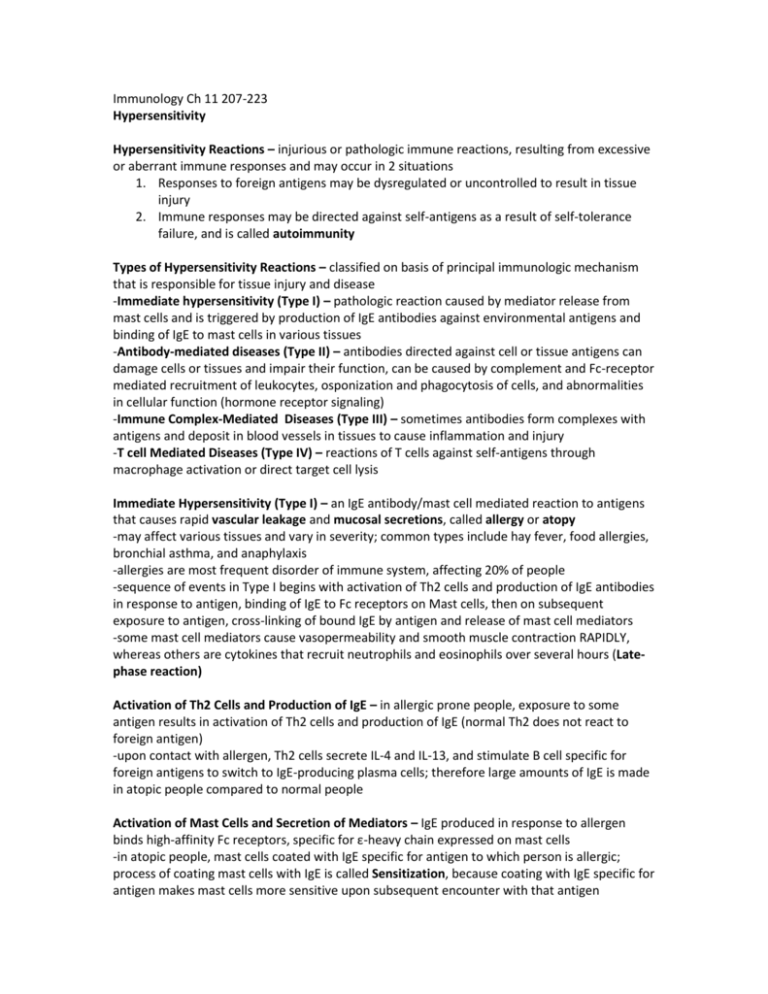
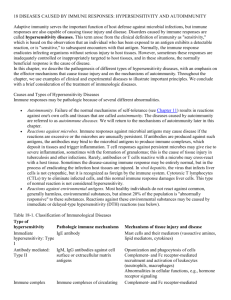
Immunology Ch 11 207-223 Hypersensitivity Hypersensitivity Reactions – injurious or pathologic immune reactions, resulting from excessive or aberrant immune responses and may occur in 2 situations 1. Responses to foreign antigens may be dysregulated or uncontrolled to result in tissue injury 2. Immune responses may be directed against self-antigens as a result of self-tolerance failure, and is called autoimmunity Types of Hypersensitivity Reactions – classified on basis of principal immunologic mechanism that is responsible for tissue injury and disease -Immediate hypersensitivity (Type I) – pathologic reaction caused by mediator release from mast cells and is triggered by production of IgE antibodies against environmental antigens and binding of IgE to mast cells in various tissues -Antibody-mediated diseases (Type II) – antibodies directed against cell or tissue antigens can damage cells or tissues and impair their function, can be caused by complement and Fc-receptor mediated recruitment of leukocytes, osponization and phagocytosis of cells, and abnormalities in cellular function (hormone receptor signaling) -Immune Complex-Mediated Diseases (Type III) – sometimes antibodies form complexes with antigens and deposit in blood vessels in tissues to cause inflammation and injury -T cell Mediated Diseases (Type IV) – reactions of T cells against self-antigens through macrophage activation or direct target cell lysis Immediate Hypersensitivity (Type I) – an IgE antibody/mast cell mediated reaction to antigens that causes rapid vascular leakage and mucosal secretions, called allergy or atopy -may affect various tissues and vary in severity; common types include hay fever, food allergies, bronchial asthma, and anaphylaxis -allergies are most frequent disorder of immune system, affecting 20% of people -sequence of events in Type I begins with activation of Th2 cells and production of IgE antibodies in response to antigen, binding of IgE to Fc receptors on Mast cells, then on subsequent exposure to antigen, cross-linking of bound IgE by antigen and release of mast cell mediators -some mast cell mediators cause vasopermeability and smooth muscle contraction RAPIDLY, whereas others are cytokines that recruit neutrophils and eosinophils over several hours (Latephase reaction) Activation of Th2 Cells and Production of IgE – in allergic prone people, exposure to some antigen results in activation of Th2 cells and production of IgE (normal Th2 does not react to foreign antigen) -upon contact with allergen, Th2 cells secrete IL-4 and IL-13, and stimulate B cell specific for foreign antigens to switch to IgE-producing plasma cells; therefore large amounts of IgE is made in atopic people compared to normal people Activation of Mast Cells and Secretion of Mediators – IgE produced in response to allergen binds high-affinity Fc receptors, specific for ε-heavy chain expressed on mast cells -in atopic people, mast cells coated with IgE specific for antigen to which person is allergic; process of coating mast cells with IgE is called Sensitization, because coating with IgE specific for antigen makes mast cells more sensitive upon subsequent encounter with that antigen -receptor for IgE is called FcεRI, and is the same receptor found on basophils, which have similar functions as mast cells -when mast cells are sensitized by IgE are exposed to allergen, cells are activated to secrete mediators -mast cell activation occurs from binding of allergen to 2 or more IgE antibodies on cell -when this happens, FcεRI carrying IgE are cross-linked, and lead to 3 types of responses from mast cells: -rapid release of granule contents, synthesis and secretion of lipid mediators, and synthesis and secretion of cytokines -most important mediators produced by mast cells are vasoactive amines and proteases stored in and released from granules, newly generated and secreted products of arachidonic acid metabolism, and cytokines -the major amine, histamine, causes vasodilation and increases vascular permeability, and stimulates transient contraction of smooth muscle -proteases may cause damage to local tissues -arachidonic acid metabolites include prostaglandins (vasodilation), and leukotrienes (stimulate prolonged smooth muscle contraction) -cytokines induce local inflammation -cytokines produced by mast cells stimulate recruitment of leukocytes to cause late-phase reaction, and involve eosinophils, neutrophils, and Th2 cells -Mast cell derived TNF and IL-4 promote neutrophil and eosinophil inflammation -chemokines produced by mast cells contribute to leukocyte recruitment -eosinophils and neutrophils liberate proteases which cause tissue damage, exacerbated by action of Th2 cells (producing more cytokines) -eosinophils are prominent components of allergic reactions and cause tissue inury -eosinophils are activated by IL-5, produced by Th2 and mast cells Clinical Syndromes and Therapy – immediate hypersensitivity reactions are attributable to mediators produced by mast cells in different amounts and in different tissues 1. in allergic rhinitis and sinusitis, reactions are to inhaled allergens such as ragweed pollen. Mast cells in nasal mucosa produce histamine, and Th2 cells produce IL-13 to cause increased mucus production. -late phase reactions leads to prolonged inflammation 2. in food allergies, ingested allergens trigger mast cell degranulation and histamine release causes INCREASED peristalsis 3. bronchial asthma results from allergic response to inhaled allergens stimulating bronchial mast cells to release mediators such as leukotrienes to cause bronchoconstriction and airway obstruction -in chronic asthma, large numbers of eosinophils in bronchial mucosa and excessive mucus secretion causes smooth muscle to hypertrophy and hyperreact to various stimuli -some asthma not related to IgE, but all are related to mast cell activation -treated with corticosteroids (reduce inflammation), leukotriene antagonists (relax bronchial smooth muscle and reduce inflammation), and phosphodiesterase inhibitors (relax bronchial smooth muscle) 4. Anaphylaxis – systemic reaction characterized by edema in many tissues including larynx, accompanied by a fall in blood pressure caused by -bee stings, penicillin, and nuts or shellfish -massive mast cell degranulation in response to systemic distribution of antigen -therapy is epinephrine (vascular smooth muscle contraction and increases cardiac output) -therapy is aimed at inhibiting mast cell degranulation, antagonizing mast cell mediators, and reducing inflammation -various allergic reactions are treated with desensitization (repeated administration of small doses of allegen), Anti-IgE antibody (neutralize IgE), Antihistamines (block action of histamine on vessels and smooth muscle), and cromolyn (inhibit mast cell degradnulation) Diseases Caused by Antibodies and Antigen-Antibody Complexes – antibodies other than IgE can cause disease by binding to their target antigens in tissues or by forming immune complexes that deposit in blood vessels -basis of many chronic immune diseases -antibodies against cells or ECM may deposit in any tissue that expresses relevant antigen -immune complexes often deposit in blood vessels, especially where plasma is filtered at high pressure, such as renal glomeruli and joint synovium Etiology of Antibody-Mediated Diseases – these Ab are most often autoantibodies against selfantigen (failure of self-tolerance) and less common against microbial antigens -two diseases caused by Ab production against microbial antigens are rare, late sequelae of stretpcoccal infections; after infection, some antibodies cross-react with antigen in heart and deposit of them in heart to trigger inflammatory rheumatic feveracute heart failure -other people from strep infection have Ab deposits in kidney glomeruli to cause inflammatory process called post-streptococcal glomerulonephritis which can lead to renal failure Mechanisms of Tissue Injury and Disease – Ab specific for tissue antigens may deposit in tissues and cause injury by inducing local tissue inflammation, may bind and destroy cells, or interfere with normal cellular functions -Ab complexes deposited in vessels induce inflammation by attracting and activating leukocytes -IgG Ab of IgG1 and IgG3 subclasses bind ot neutrophils and macrophage Fc receptors to activate them and cause inflammation -IgG1, IgG3, and IgM activate complement system by classical pathway resulting in recruitment of leukocytes and inflammation -leukocytes recruited by antibody deposition release reactive oxygen species and lysosomal enzymes that damage adjacent tisseus -if antibodies bind to cells like erythrocytes and platelets, phagocytes can opsonize them -antibodies against hormone receptors may inhibit receptor functions (myasthenia gravis) -antibodies for Acetylcholine receptor inhibit neuromuscular junction transmissionparalysis -antibodies against TSH in hyperthyroidism (graves disease) stimulate thyroid without TSH Clinical Syndromes and Therapy – two models of immune complex diseases have given insight 1. Serum Thickness – administration of protein antigen (such as treatment for snake venom or rabies) elicits an Ab response and forms circulating Ab complexes in blood 2. Arthus Reaction – induced by subcutaneous administration of protein antigen to a previously immunized animal to result in immune complexes at site of antigen injection and localized vasculitis -therapy for these diseases is to limit inflammation and its consequences, such as with corticosteroids -plasmapheresis is sometimes used to reduce circulating antibodies -some diseases respond well to treatment with intravenous IgG pooled from healthy donors -treatment of patients with an Ab for CD20, surface protein for mature B cells, results in depletion of B cells and may be useful for treating these disorders Diseases Caused by T Lymphocytes – many autoimmune diseases focused on T cells Etiology of T cell-mediated diseases – major causes of T-cell hypersensitivity are autoimmunity and exaggerated or persistent responses to environmental antigens -autoimmune reactions usually directed against cellular antigens with restricted tissue areas, and tend to be limited to a few organs and not systemic -examples of type IV hypersensitivity to environmental antigens include contact sensitivity to chemicals (poison ivy) -tissue injury can accompany T cell responses to microbes, such as in tuberculosis, where response is chronic because infection is difficult to eradicate -resultant granulomatous inflammation causes injury to normal cells -in hepatisis virus, virus is not itself cytopathic, but cytotoxic T lymphocytes cause liver injury -excessive polyclonal T cell activation by certain microbial toxins can lead to production of many inflammatory cytokines to induce syndrome similar to shock (these toxins called superantigens) because they stimulate large numbers of T cells Mechanisms of Type IV tissue injury – caused by inflammation induced by cytokines produced mainly by CD4+ T cells or by killing host cells by CD8+ T cells -CD4 cells react against cell or tissue antigens and secrete cytokines to induce local inflammation and activate macrophages -diseases can be associated with activation of Th1 and Th17 cells -Th1 cells produce IFN-g, principal macrophage activator, and Th17 cells responsible for recruiting leukocytes like neutrophils -actual tissue injury caused by neutrophils and macrophages -typical reaction by T cell cytokines is delayed-type hypersensitivity (DTH), because it occurs 2448 hours after person is previously exposed to protein antigen, and it takes a long time because it takes several hours for circulating effector T cells to home to the site of antigen challenge and induce a response -DTH reactions are manifested by infiltrates of T cells and monocytes in tissues, edema and fibrin deposition caused by increased vascular permeability in response to cytokines from CD4 cells, and tissue damage caused by macrophages and activated T cells -DTH reaction to mycobacterial antigen, PPD, is an indicator of T cell response to mycobacteria -CD8+ T cells specific for antigens on host cells may directly kill cells, but may also produce cytokines that induce inflammation Clinical Syndromes and Therapy – many organ-specific autoimmune diseases believed to be caused by T cells, are typically chronic and progressive -tissue injury causes release and alteration of self-proteins, which may result in reactions against these newly encountered proteins, called epitope spreading -chronic inflammatory diseases that are initiated by immune reactions are called immunemediated inflammatory diseases -therapy for T cell-mediated hypersensitivity is designed to reduce inflammation and inhibit T cell responses -antiinflammatory steroids -antagonists to TNF are beneficial to patients with rheumatoid arthritis and IBD by reducing inflammation -drugs that block costimulation such as B7 and antagonists against receptors for cytokines IL-1, IL-6, and IL-17 are useful -B-cell depletion with anti-CD20 has proved effective in rheumatoid arthritis and multiple sclerosis