Tubulo-Interstitial Disease
advertisement
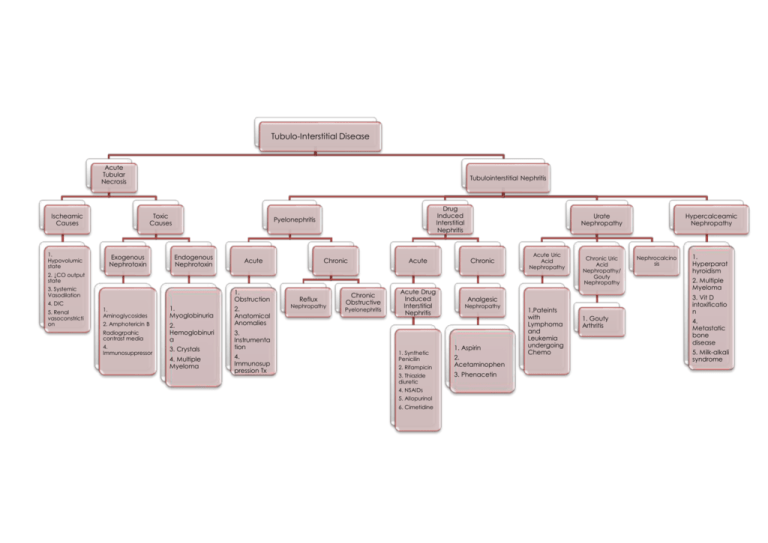
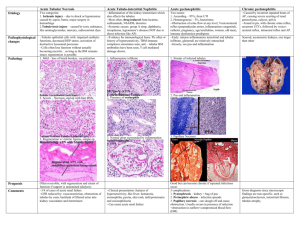
Tubulo-Interstitial Disease Acute Tubular Necrosis Ischeamic Causes 1. Hypovolumic state Tubulointerstitial Nephritis Toxic Causes Exogenous Nephrotoxin Drug Induced Interstitial Nephritis Pyelonephritis Endogenous Nephrotoxin Acute Chronic Acute Urate Nephropathy Chronic Acute Uric Acid Nephropathy 2. ↓CO output state 3. Systemic Vasodilation 4. DIC 5. Renal vasoconstricti on 1. Obstruction 1. Aminoglycosides 1. Myoglobinuria 2. Amphotericin B 2. Hemoglobinuri a Radiogrpahic contrast media 4. Immunosuppressor 3. Crystals 4. Multiple Myeloma 2. Anatomical Anomalies 3. Instrumenta tion 4. Immunosup pression Tx Reflux Nephropathy Chronic Obstructive Pyelonephritis Acute Drug Induced Interstitial Nephritis 1. Synthetic Penicilin 2. Rifampicin 3. Thiazide diuretic 4. NSAIDs 5. Allopurinol 6. Cimetidine Chronic Uric Acid Nephropathy/ Gouty Nephropathy Analgesic Nephropathy 1. Aspirin 2. Acetaminophen 3. Phenacetin 1.Pateints with Lymphoma and Leukemia undergoing Chemo 1. Gouty Arthritis Hypercalceamic Nephropathy Nephrocalcino sis 1. Hyperparat hyroidism 2. Multiple Myeloma 3. Vit D intoxificatio n 4. Metastatic bone disease 5. Milk-alkali syndrome Clinical Features Acute Tubular Necrosis Chracterized by Rapid destruction of tubular epithelium Rapid reduction in urine output o <400ml per day The most common cause of Acute Renal Failure in renal category The Initiation Phase Acute decrease in GFR to a very low level Sudden increase in o Serum creatinine o Blood Urea Nitrogen (BUN) The Maintenance Phase Sustained severe reduction in GFR Sustained increase in o Serum creatinine o BUN Continues for a period of time, usually 1-2 weeks The Recovery Phase Increase in urine ouput o Happens when Oliguria present during Maintenance Phase Gradual decrease in o Serum crearinine o BUN Restoration of tubular function Pathogenesis o o o o o o Prognosis o o o o o Motality rate 50% 60% mortality rate in pts with Shock due to sepsis Severe burn Multiorgan failure 30% mortality rate in pts due to Nephrotoxic agents Patient can recover if doesn’t develop organs failure during the course 50% may have some renal impairment 5% have decline in renal function 5% never recover kidney function and require dialysis o o o Tubular epithelium is highly sensitive towards Hypoxia Chemical irritants Ischeamia can cause Depletion in ATP due to lack of O2 Increased in cytosolic level of Calcium Free radical formation Metabolism in membrane phospholipid metabolism Abnormalities in cell volume regulation Consequently will lead to Disruption in Cell volume regulation Electrolyte regulation Ineffective membrane transport Cell swollen Intracellular accumulation of Calcium Sodium Nephrotoxic agents can cause Intrarenal vasoconstriction Direct toxicity to tubular cells Intratubular obstruction Gross o o Morphology Microscopy Kidney appears Pale Swollen Congested medullary parenchyma o o o o o o o o o o General feature Ragged tubular epithelium (necrosis) Interstitial edema Tubular cast present in urine Ischeamic ATN Patchy tubular necrosis Straight Proximal Tubule is the most susceptible Rupture of basement membrane (Tubulorrhexis) Tubular casts Nephrotoxic ATN Uniform involvement of tubular segment Sparing of distal tubule Preservation of basement membrane Laboratory Investigation Blood Urea and Serum Electrolyte (BUSE) Complete Blood Count (CBC) Full Blood Count (FBC) Urine Full Examination Microscopy Elements (UFEME) Urine Sample (US) Renal Biopsy (rarely needed) Complication o o o o o o o o o o Electrolytes Abnormalities Hypekaleamia Hyponatreamia Hypermagneseamia Hypocalceamia Hyperphosphateamia Intravascular Volume Overload May lead to Pulmonary Edema Hypertension Due to salt and water retention Ureamic Syndrome Precardial disease GIT upsets Neurological symptoms Metabolic Acidosis Epidemiology Acute Pyelonephritis Chronic Risk Factors Female Pregnancy Urinary tract obstruction o Benign Prostatic Hypertrophy o Tumor o Calculi o Neurogenic bladder o Pre-existing renal lesion with intrarenal scarring Anatomical anomalies o Vesicoureteral Reflux Instrumentation o Catetherization Immunosuppression Tx Chronic tubulointerstitial inflammation Renal scarring with pathologic involvement of o Calyces o Pelvis Can be categorized in 2 o Reflux Nephropathy Common Can be either Unilateral Bilateral o Chronic Obstructive Nephropathy Obstruction leads to Parenchymal atrophy Can be either Unilateral o Calculi Bilateral o Obstructive anomalies of UT Pathogenesis Acending infections o Due to reflux of pathogens against the flow of the urine o ‘can be due to Vesicoure teral reflux Intrarenal reflux Heamatogeno us spread of bacteria secondary to bactereamia Morphology Gross Microscopic Cortical Acute inflammatory surface can exudate within have o Tubule o Grayish o Intrarenal white area interstitium of Intratubular inflammati aggregates of on Neutrophils o Abscess o Leukocyte cast formation in the urine Patchy interstitial suppurative inflammation Surface is irregular Cut surface o Dilated calyces o Blunted calyces Focal/ extensive chronic inflammation with interstitial fibrosis Tubules are o Atrophic o Dilated Thyroidization happens due to dilated tubules containing Eosinophilic Proteinaceous Material Clinical Features Loin/back/ flank pain Systemic evidence of infection o Fever o Malaise Bladder and Urethral irritation o Urgency o Frequency o Dysuria Urinalysis o Pyuria Urine with many leukocytes o Leukocytes casts Idicator of renal involvement Complications (ACUTE) Endotoxic shock/ Septiceamia Papillary necrosis Perinephric abscess o Invasion of inflammation from the renal capsule to perinephric tissue Pyonephrosis o Suppurative exudate in Pelvis Calyx Ureter o Due to total/ partial obstruction Fibrosis o Distortion of shape and function Epidemiology Acute DrugInduced Interstitial Nephritis Adverse effects of certain Nephrotoxic drugs such as o Methicillin Trigger interstitial immunologica l response o Gentamicin Directly cause ATN o Analgesic abused Subtle but cumulative tubular injuries Pathogenesis Drugs bind covalently with cytoplasmic and extracellular components of tubular cells These complex then become Immunogenic The injury happens due to IgE/ cellular immune mediated response to o Tubular cells o Basement membrane Gross Morphology Microscopic Hardly seen any gross changes on the kidneys o o o o o o Interstitial edema and inflammation Infiltration of Lymphocytes Macrophages Large number of Eosinophils Neutrophils Small number of Basohils Tubulitis Intratubular epithelial Lymphocytes Tubular Necrosis Regeneration Clinical Features o o o o o o o Drug-Induced Interstitial Nephritis o o o o Analgesic Neuropathy (Chronic) Women>men Prevalent in pts with Recurrent headache Muscle pain Psychoneurotic Factory workers These subjects often abuse analgesics o o o o o o Analgesic mixture can cause damage to kidney through Renal papillary necrosis Chronic tubulointerstitial nephritis Phenacetin metabolite and Acetaminohen Injures the cells through Covalent binding that elicits immune response Oxidative stress Aspirin Inhibits vasodilatory effects of Prostaglandin Leads to Papillary ischeamia End up with Coagulative Necrosis Children Cause the Minimal Change Disease Maybe due to injury to Podocytes by cytokine during inflammation Adults Cause Membranous Glomerulonephritis Causes remain unknown o o o o o o Kidney appears smaller or normal in size Renal papilae Various stages of necrosis Calcification Fragmentation Sloughing Renal cortex Depressed/ atrophic Raised areas o o o o o o Renal cortex Loss and atrophy of tubules Interstitial fibrosis and inflammation Due to obstruction by damaged tubular cells in the papillae Renal papillae Early Patchy papillary necrosis Advanced Entire papillary necrosis Ghosts of tubules – coagulative necrosis Foci of calcification o o o o Begins about 15 days after exposure to drugs Characterized Fever Transient Eosinophilia Rash Renal abnormalities Heamaturia Mild proteinuria Leukocyturia In older patients Acute renal failure Increased serum creatinine Withdrawal of the offending drugs is followed by recovery May take several months Irreversable damage often happens in elderly Findings Early Inabality of kidney to concentrate urine Late Distal tubular acidocis Renal stone Clinical Features Early Headache Aneamia GIT symptoms Hypertension UTI (50%) Later Heamaturia Renal colic Due to obstruction of tubule by necrotic papillae