Policy Number, REPEAT PRESCRIPTION, MEDICATION REVIEW
advertisement

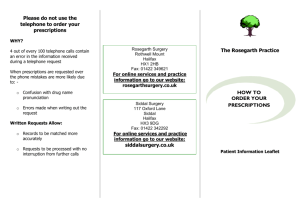
1 Policy Number, REPEAT PRESCRIPTION, MEDICATION REVIEW and MEDICINES RECONCILIATION POLICY June 2010 Date approved and name of approving body. Replaces [ref or date of previous policy] Review Date 1st June 2012 1 1.1 Summary The aim is to provide a safe and efficient repeat prescribing and medication review system, for use in general practice, which ensures effective appropriate treatment, provides monitoring for long term conditions and minimizes patient harm, inappropriate requests, drug wastage and prescribing errors. Systems should be in place to ensure that changes to a patient’s medication made by a practitioner outside the practice e.g. Community Nurse or hospital doctor, are updated on the patient’s medical record and reviewed appropriately. The policy should be implemented by practice managers with support from all practice staff. 2. The policy 2.1 Ordering repeat prescriptions Repeat prescriptions should ideally be requested by the patient. The patient should only order items that they need between now and when the next repeat request is due. Where a third party is responsible for the ordering of repeat prescriptions they should have the authority to do so from the patient and should obtain clear instructions, at the time the request is made as to which items are required. Repeat requests should be made on the tear off section of the previous prescription. Other arrangements may be in place. (See appendix 1 Information for Patients) 2.2 Who can issue a repeat prescription The practice manager should only allow competent staff to be responsible for issuing repeat medication. Staff authorized to print off a repeat 2 prescription should be members of practice staff that have been specifically trained and accredited in the repeat prescribing process or a doctor or a competent nurse or pharmacist working in the practice 2.3 The repeat prescription process The competent person should check the repeat prescription request to make sure the patient’s intention is clear and, if unsure, confirm the items required with the patient or their authorized representative directly. If a medication review is due or individual items appear to be over or under used or have reached the end of their repeat authorization period, the competent person should contact the prescriber. (See Appendix2 and Appendix 3) 2.4 The prescriber The prescriber is responsible for ensuring that medication reviews and repeat authorizations are completed in a timely fashion. They should check that the drugs are still required clinically and that monitoring is up to date. Wherever possible, the length of supply of each of the repeat medications should be aligned to the number of days specified in the practice repeat prescription policy and should also take account of patient’s current stockholding. Any changes to medication made by external prescribers should be reconciled. Repeat prescriptions should be signed in protected time with minimal interruptions. (See appendix 4) 2.5 Storage of signed prescriptions Signed repeat prescriptions should be stored in a way that prevents unauthorized access. They should be stored in a locked cupboard or draw when the surgery is closed. 2.6 Issuing signed prescriptions to patients and their authorized representatives To ensure that prescriptions are only collected by patients or their authorized representative, practice staff should request further details e.g. confirmation of address before issuing the prescription. If controlled drugs, or any drug liable to misuse, is included on the prescription then further identification should be sought. 3 Drivers or other pharmacy staff collecting prescriptions, as the patients authorized representative, should sign for each prescription form recording details of the patient name, number of items, and date collected. This serves as an audit trail if prescriptions are lost. Non-practice staff should not be allowed to retrieve signed prescriptions from where they are stored as this may breach the confidentiality of other patients. 2.7 Repeat Dispensing Arrangements Practices should consider taking part in the scheme in order to reduce the number of repeat prescriptions requiring signature, improve medicines compliance and the monitoring of repeat drug use via the feedback from community pharmacists. (See appendix 5) 3. Implementation 3.1 The policy should be implemented by practice managers with support from all practice staff. (See Appendix 6) 3.2 Practice staff, patients, patient’s authorized representatives and community pharmacists should be informed of any changes in the existing repeat prescribing system. Arrangements for Bank Holidays, any half days and weekends should be clearly stated. 4 This policy has was forwarded to the Healthcare Commission for the Medicines Management Post Discharge Pilot Survey November 2008 Appendices Appendix 1 Information for patients What is a Medication Review? It is a talk you can have with a doctor, nurse or pharmacist to ensure that you are comfortable taking your medication. 5 It is an opportunity to confirm that you are taking the right medicines in the right way, in the right amounts and that you are getting the right effects. It is also your opportunity to learn more about your medications and a chance to discuss any questions or concerns you might have What are repeat prescriptions? They are prescriptions for your medication that you can order from the GP practice without having to see a prescriber each time. Repeat prescriptions regularly need to be checked by a prescriber to make sure that your medication is working correctly. Thus, you might only be able to order a certain number of repeat prescriptions before you have to see the prescriber On occasions the prescriber may request that you attend a medication review. It is important that you do attend. How to order a repeat prescription Order you repeat prescription in plenty of time – allow at least [no of days stated in your repeat prescribing policy] working days. If you use the repeat prescription form counterfoil please tick the items carefully. You will only be able to order items that are on your repeat slip; for anything else you may need to make an appointment with a prescriber If you order by e-mail fax or telephone, please order the items carefully and give the practice full details of the prescribed medicines. Order only those items that you need If you do not need a particular medication this time, please do not order it. You will still be able to order it at a later date when you do need it. When you collect your prescription from the surgery, please check that it is only for the medications that you have ordered. Please inform the receptionist if there are any errors. Repeat prescriptions should only be ordered in writing; however you may be able to order by e-mail, telephone or fax depending on your circumstances or practice 6 If you agree that a community pharmacy can collect and/or deliver your prescriptions then you must make it clear to your doctor which pharmacy you have chosen If you agree that a carer or community pharmacist can order your prescriptions on your behalf, please make sure you only allow them to order the items you need. If you receive any medicines that you did not request please inform your doctor When you receive or collect your medicines from the pharmacy please check that you only receive items that you requested. Inform the practice if there are any unexpected items. Taking Care of Your Medication Know the names of all your medicines (these includes tablets, capsules, inhalers, liquid medicines, testing strips and so on) and what they are used for If you cannot remember what medicine is for then you can book a free medicines use review (MUR) with your regular dispensing pharmacist If you stop taking a prescribed medication for any reason, please make an appointment to discuss how you feel about the medicine with a with a doctor, nurse or practice pharmacist If you need to take more or less of a medication than the pharmacy label allows, please make an appointment to discuss how you feel about the medicine with a with a doctor, nurse or practice pharmacist Do not take non-prescribed medication (e.g. over the counter, health foods or herbal or Chinese medicines) without checking with your prescriber or pharmacist. It may interfere with your regular medication and may be harmful. Medicines and Wastage A large amount of medication is wasted every year. Some of this is due to people ordering medication that they do not need or do not take. If you have decided not to take a medicine (you should take advice from a doctor, nurse or pharmacist before stopping any medication) please do not re-order it. Make an appointment with a doctor, nurse of pharmacist to discuss why you have made this decision. 7 Medicines that have been ordered and returned to the pharmacy cannot be reused even if they are unopened and must be destroyed. You can help to reduce the amount of wastage by ordering only those items that you use and need. Safe Disposal of Unwanted Medicines Do not throw away unwanted medication and do not flush any down the toilet Always return expired, unused and unwanted medication to your local pharmacy. They will dispose of it safely. Repeat Dispensing Arrangements This is a system whereby your doctor or nurse can provide you with a series of repeat prescriptions which you can either keep or give to your dispensing pharmacist to keep for you. You can then have these dispensed at appropriate times without the need to see your doctor in between. You may be able to take part providing that you medication and health problems are unlikely to change in the near future. The system reduces the number of prescriptions your doctor or nurse needs to sign and involves your dispensing pharmacist more closely in your health care. The system can be arranged to allow you to control when you collect you repeat prescriptions, for example in advance of going on holiday. Each patient must give their consent before the arrangements can start. 8 Appendix 2 Authorized Members of Practice Staff Responsibilities Is the request for a patient at this surgery? It is important that the prescriptions request form is one that was generated by your practice. Those that were generated by a new patients’ previous surgery should be interpreted very carefully and reviewed by a doctor or competent nurse or pharmacist within your practice before being processed. Is this a patient that the practice has particular concerns about? There may be a handful of named patients who should not to have medications on repeat without direct contact with their prescriber. Is it clear which medicines the patient requires? If the patient has left the form blank and it is not obvious from their computer record which medication is needed then preferably the patient, or failing this, their authorized representative should be contacted. Are the requested medicines allowable on repeat? Confirm that items requested are allowed on repeat and are within their authorized period and that the prescriber specified that the item should be repeated and it was not a one-off supply. The practice’s repeat prescribing policy should list all of the items are not allowed on repeat prescription The following drugs or drug classes are generally less suitable for repeat prescribing although this will depend on individual practice policy (if you are unsure please contact the Medicines Management Team): Antibiotics-some exceptions The contraceptive pill 9 HRT Benzodiazepines Antidepressants Schedule 2 and 3 controlled drugs with the exception of phenobarbital Drugs that require regular monitoring. Any drug that has an abuse potential-may be appropriate for certain patients only. Any new drugs, until effectiveness and tolerability have been established Are there any repeats left for each requested item? Check the number of repeats left before the patient’s next review. If there are no repeats left for the item, the prescriber and patient should be notified and a review arranged. Is the medicine being used too frequently? Check the period since the last request. The computer should normally alert the user if the medication appears to be over used. If problems are suspected the prescriber should be alerted, preferably before the prescription is produced. Prescriptions should not be printed at less than the time intervals that have been authorized without agreeing the reason for this (e.g. holiday). The reason should be documented in the patient’s notes Is the medicine being used too infrequently? Are there repeat items on the patient’s computer record that have not been requested? Check the period since the last request. The computer should normally alert the user if the medication appears to be underused. If problems of non-compliance are suspected the prescriber should be alerted, preferably before the prescription is produced. Note some medicines may be seasonal e.g. antihistamines, or have a long shelf life but may be used infrequently e.g. GTN spray Does the request form contain any notes or alterations from the prescriber? The prescriber may have indicated on the previous occasion that the patient needs to be seen for a review, or may have requested a monitoring test/measurement (e.g. liver function test). The receptionist should confirm that the request has been fulfilled. 10 If the patient is overdue for review, this should be brought to the attention of the prescriber. A mechanism should be in place for dealing with patients who fail to make appointments when they are due for a review. This process should be explained in the practice repeat prescribing policy. If the presciber has amended the dosage instructions on the repeat prescription, the patient’s medical records should be amended accordingly once any change has been confirmed by the prescriber. Does the request form contain any manual alterations from the patient? Any manual alterations to the request form by the patient/or their authorized representative are to be brought to the attention of the prescriber (e.g. “I no longer take this medication”). Any manual additions by the patient should be referred to the prescriber before being added on to the list of repeatable medications. Any request to alter the strength or dosage of a repeat item (other than in writing from an official source e.g. hospital doctor) MUST be referred to the patient’s prescriber. Only when authorization has been give by the prescriber, can the prescriptions details be changed. Are full dosage instructions included? Check that full instructions are provided for each requested item, e.g. name of drug, form of drug (e.g. tablets capsules), strength of the drug, the dosage, the frequency of dosage and the quantity to be supplied. Less information may be appropriate in the case of prescriptions for dressings, appliances (e.g. catheters) and chemical reagents (e.g. blood glucose testing strips). If in doubt, refer to the prescriber. Is the quantity of each medicine being requested excessive? Verify that quantity of each item equates to the maximum prescription length (e.g. 28 days supply) allowed by the practice as stated in the practice policy Are there any discontinued therapies? If the patient has not requested a particular item for a specified amount of time (e.g. 3 months) then this may indicate poor compliance. The prescriber should be alerted and the patient called in for a medication review. The items 11 can be removed from the repeat request form if the prescriber agrees that they are no longer needed. Note some medicines may be seasonal e.g. antihistamines, or have a long shelf life but may be used infrequently e.g. GTN spray Are you in any way concerned or uncertain about the patient or the items being requested? Any prescription requests about which staff are uncertain or concerned should be referred to the prescriber Is the prescription legible? The printed or handwritten prescription should be legible and contain the name and address of the patient, the patents date of birth, the full names of all the drugs prescribed and the detail as above. Has a record of the prescription been made? All repeat prescriptions issued are automatically recorded in the patient’s computer medical records. There should be a process for adding the detail of handwritten prescriptions written by members of the practice, secondary care, Out of Hours or by community practitioners. Can the prescription be altered? Handwritten prescriptions should state the number of items on the prescriptions. Particular attention should be paid to certain drugs (e.g. where the quantity may be altered); if the prescriber has concerns then they can specify the quantity in words and figures. To prevent the addition of further items, the spare space on the prescription should be crossed through by the prescriber. Where the computer has failed to cancel out unused space t his should be done manually to prevent any unauthorized additions. Is the patient suitable for the Repeat Dispensing Arrangements? If the patient’s medication requirements and disease(s) are stable they may be suitable for the repeat dispensing arrangements. (See appendix 5) 12 See http://www.nhsbsa.nhs.uk/PrescriptionServices/1856.aspx on prescription writing. Appendix 3 Repeat Prescribing Process for more details 13 Patient/carer puts request in at practice for repeat medication Request collected by appropriate member of staff for processing Does prescription request require clarification or reauthorization; is there any medication that have not been collected for some time or that appears to be overused or has medication been recently changed by a practice member or external prescriber? Yes No Clarify medication with patient Obtain authority to re-authorize Book a medication review or medicines reconciliation with a doctor or a competent nurse or practice pharmacist Do the patient’s medication quantities need to be changed so that they all run out at the same time No Process prescription request Yes Consider booking patient for a review with the practice pharmacist. If necessary issue a “one off” prescription and align the patient’s medication to equalize quantities 14 Pass to doctor for signing Appendix 4 Safe storage Signing Repeat Prescriptions and Medication Review/Reconciliation Signing Repeat prescriptions Any medical and non-medical prescriber can sign a prescription provided that they are satisfied with the request, are competent to prescribe all the drugs on the prescription and are satisfied with the way the drugs have been prescribed. Repeat prescriptions should be checked and signed in protected time with minimal interruptions. Prescribers should be aware of their responsibilities regarding signing of repeat prescriptions for patients not familiar to them especially if there are queries or incomplete patient records If a prescriber is concerned about a patient’s compliance then they should arrange to see the patient as soon as possible; however if this would delay the patient’s access to medicines or otherwise affect patient care then the issue may be resolved on a temporary basis by speaking with the patient on the phone. Prescriptions that have the following instructions ‘As directed’ or ‘When required should be amended to include the normal dose, frequency, indication and maximum dose/over time e.g. “Two tablets to be taken four times a day as directed/required, for pain, up to a maximum of eight tablets in 24 hours” Reporting Adverse Drug Reactions 15 Prescribers are responsible for reporting all suspected adverse drug reactions involving new drugs, (so called black triangle drugs-annotated ) and any novel adverse drug reactions for all other drugs, to the MHRA using the yellow card scheme https://yellowcard.mhra.gov.uk/hcp/ Reviewing Medicines Patients may use medicines long term. The initial decision to prescribe medicines, the patient’s experience of using the medicines and the patient’s needs for support to adhere to the prescribed medicine regimen may change over time and should be reviewed regularly. Offer repeat information and review, especially when treating long-term conditions with multiple medicines. Review at agreed intervals patients’ knowledge, understanding and concerns about medicines and whether they think they still need the medicine. Ask about side effects and the patient’s tolerance to these. Ask about adherence to the prescribed regimen when reviewing medicines. Clarify possible causes of non-adherence and agree any action with the patient (including a date for follow-up). Bear in mind that patients sometimes evaluate prescribed medicines in their own way (for example, by stopping and starting them and monitoring symptoms). Ask the patient if they have their own way of weighing up their medicine. 16 Medicines Adherence-see NICE Clinical Guideline 76 http://www.nice.org.uk/nicemedia/pdf/CG%2076%20Medicines%20adherence%20Q RG%20FINAL.PDF Medication Review Types of Medication Review Review Access to patient notes Patient /carer involvement Description Assesses technical issues relating to the Does not need Type 1 Prescription prescription e.g. No* patient/carer to be (Medicines) review anomalies, changed present items and cost effective prescribing Concordance Usually requires Addresses issues Type 2 and Not patient and /or relating to patient’s (Medicines compliance necessarily* carer to be medicine taking use) review present behaviour Type 3 Addresses issues Clinical Requires patient (Medicines relating to patient’s use Medication Essential and /or carer to and of medicines in the Review be present condition) context of their condition * Any changes to medication will have to be communicated to the patient/carer 17 For more information see “A Guide to Medication Review.” National Prescribing Centre. 2008 http://www.npci.org.uk/medicines_management/review/medireview/resources/agtmr_web1.pdf A full review of a patient’s medical record is to be undertaken when the patient has had all the authorized repeats. Regular review should be included as part of the policy for patients with long term conditions e.g. asthma, COPD, diabetes, CVD, hypertension, heart failure etc. or high risk patients on key drugs e.g. older patients taking NSAIDs, patients on warfarin, controlled drugs, diuretics or two anti-platelets. The practice should take note and act on any issues raised by Medicines Use Reviews, carried out by community pharmacists, and feedback where appropriate. Regular medication review should be a priority for patients that are housebound, in sheltered accommodation or in care homes. A six monthly review will be appropriate for most of these patients. Practices should have a system in place to remind practitioners when reviews are due and should allocate the required time for GP, Community Matron, competent nurse or pharmacist to undertake the reviews, in the patients home/care home if necessary. Review of the notes to be undertaken by competent health care professionals ( please state categories of staff) Depending on the results of the review, the prescriber will then either: Authorize the prescription for further repeats and record in the patient’s notes that a review has taken place and the prescription has been re-authorized, or Request that the patient attend a consultation Frequency of Review 12 month review for all patients who are on repeat medication. 18 6 month review for all patients over 75 years who are on four or more medications. Patients should be notified when they are required to attend for a review of their medication. The following are examples of what a patient’s medication review may include: Review of the patients medical condition(s) Review of the effectiveness of the patients medication Any monitoring and subsequent test results Patient’s understanding of the repeat prescribing system Patient’s understanding of what their medication is for and its effectiveness Knowledge of dose, frequency and any other issues relating to administration Any side effects or problems with taking the drug which might require review A discussion around compliance and concordance Other non-prescription drugs being taken e.g. over the counter or herbal/alternative products Any general queries they may have about their medication What quantity of each drug does the patient currently hold Can they open the containers easily 19 Following the review, the action taken is to be recorded in the patient’s notes, preferably by read code. All changes to the prescription are to be recorded on the computer system by the reviewer. Sufficient time should be allocated for a face to face medication review. If patients are having difficulty remembering to take their medication they may find a medicines reminder chart useful. Alternatively they can be initially assessed for a monitored dosage system (MDS) using the form available at: http://pcttransition/pcttransition/Pharmacy/MDS/MDS%20Initial%20assessment%20f orm%20version%20final.pdf The patient should then be referred to their community pharmacist along with a completed copy of the form. More information regarding MDS can be found at: http://intranet.pct.xwalsall.nhs.uk/Medman/M_D_S.asp Competency Framework for Practitioners Undertaking Face –to-Face Medication Reviews Competency Area Competency Overarching Statement 20 Building a partnership Listening Communication Listen actively to the patient Helps the patient to interpret information in a way meaningful to them Context With the patient defines and agrees the purpose of the consultation Has up-to-date knowledge of area of practice and wider health services Managing a Shared Consultation Knowledge Sharing a Decision Understanding Exploring Deciding Monitoring Recognizes that the patient is an individual Discusses illness and treatment options, including no treatment Decides with the patient the best management strategy Agrees with the patient what happens next For more information see “A Guide to Medication Review.” National Prescribing Centre. 2008 http://www.npci.org.uk/medicines_management/review/medireview/resources/agtmr_web1.pdf A Template for Medication Review is available from the Medicines Management Team Medicines Reconciliation-The aim of medicines reconciliation when patients change care settings is to ensure that medicines prescribed in the new setting (e.g. on admission to hospital) correspond to those that the patient was taking in the previous care setting (e.g. medicines prescribed by the patient’s GP) Medicines Reconciliation on Discharge from Hospital Medicines reconciliation is an important task, those that undertake it should be competent to do so 21 The following members of the practice staff should be responsible for medicines reconciliation (including the implementation of any drug changes in the patients medical record)- a doctor or a competent nurse, pharmacist or pharmacy technician. There should be robust processes for the collecting and receiving information regarding patient discharge information from secondary care Any missing information on the discharge summary should be completed by contacting the ward, pharmacy department, the discharging practitioner or the patient Where missing information cannot be obtained the prescriber should undertake a full medication review with the patient. The discharge information should clearly state which medicines have been changed, those that have been stopped and those that have been started and the reason. The following data should be expected: o Complete and accurate patient details including full name, date of birth, weight if under 16 years, NHS/unit number, consultant, ward, date of admission, date of discharge o The diagnosis of the presenting condition plus co-morbidities o Procedures carried out o A list of all medicines prescribed for the patient on discharge form hospital (not just those dispensed at the time of discharge) o Dose, frequency, formulation and route of administration o Medicines stopped and started, with reasons and dates o Length of courses where appropriate (e.g. antibiotics) o Details of variable dosage regimens e.g oral steroids, warfarin etc. o Known allergies, intolerance and hypersensitivities and previous drug interactions o Any additional patient information provided such as corticosteroid record cards, anticoagulant books etc. o Details of any follow up appointments 22 Adapted from http://www.npci.org.uk/medicines_management/safety/reconcil/resources /reconciliation_guide-a5ordered.pdf Ongoing concerns about missing data should be fed back to the tPCT and provider. Practices should participate in local audits. Any future monitoring required after the patient has been discharged should be undertaken and facilitated by the use of screen messages and reminders in the patients medical record The process should be double checked by another person from the list above The The practice pharmacist should be involved in medicines reconciliation, especially where the patients are at high risk of harm from either their prescribed medication e.g. patients discharged on controlled drugs, NSAIDs or warfarin or diuretics or on two anti-platelets or when they are in a vulnerable patient group e.g. the elderly, those with complex comorbidities and/or patients receiving polypharmacy. Wherever possible assistive technologies should be used to reduce patient harm e.g. patient safety messages on ScriptSwitch. practice pharmacist should facilitate the above process Medicines reconciliation when patients are admitted to hospital Medicines reconciliation is equally important when patients are admitted to secondary care and practices should supply the following data as soon as possible after admission either by e-mail or to a secure fax o Complete patient details including full name, date of birth, weight if under 16 years, NHS/unit number, GP, date of admission o The presenting condition plus co-morbidities o A list of all medicines currently prescribed for the patient including those bought over-the-counter (where this is known) 23 o Dose, frequency, formulation and route of administration o An indication of those medicines that are not intended to be continued o Known allergies and previous drug interactions N.B. Medicines reconciliation for any patient that crosses any other care “Interface” e.g. from GP practice to a Care Home should adopt the same principles and data sets Competencies for Practitioners undertaking Medicines Reconciliation Many of the competencies for staff undertaking medication review apply to medicines reconciliation; however the NPC has indicated that the following skills are required for practitioners undertaking medicines reconciliation: Effective two way communication skills Technical Knowledge 1. 2. 3. 4. 5. 6. 7. Therapeutic Knowledge This level of therapeutic knowledge would normally be achieved by pharmacists, doctors, or suitably experienced pharmacy technicians or nurses. Verbal, Non verbal Written skills Active listening Questioning techniques Giving and receiving feedback Understanding of relevant policies and procedures e.g.: Local medicines documentation Discharge summaries NMP Fax form Patient own drugs policy Repeat prescribing policy GP practice system MDS availability Up to date knowledge of brand and generic names of drugs Forms in which drugs are available Licensed indications Common dosage directions 24 Ability to correctly interpret a prescription including dose and directions Knowledge of the legal requirements for the prescribing, recording, administration and storage of medicines (including controlled drugs) A basic understanding of what the medicine is intended to do and how it works Adapted from http://www.npci.org.uk/medicines_management/safety/reconcil/resources/reconcilia tion_guide-a5ordered.pdf Prescribing by Community Nurses Where a non-medical prescriber, based in the community, issues a prescription for a patient they should fill in the attached form and fax it to the patient’s practice as soon as possible. Form available from: http://pcttransition/pcttransition/Pharmacy/Non%20Medical%20Prescribing/n urse%20presc%20fax.pdf On receipt of the above form, the patient’s doctor should be informed; they will authorize appropriate changes to the patient medical record e.g. the drug added as a repeat and the form scanned into the patient’s computer record 25 Appendix 5 Repeat Dispensing Arrangements Patients in the scheme should be on stable medication regimens A medication review should be undertaken before patients are accepted into the scheme The patient should complete a patient consent form “As required” and “as directed” medicines are not suitable for inclusion in the scheme For maximum flexibility the prescriber should not specify a dispensing interval; however a set interval may be appropriate for some patients or in certain situations Schedule 1, 2 and 3 controlled drugs are not suitable for inclusion in the scheme Care should be taken with inhalers, topical preparations and liquids oral medicines to ensure that the patient does not receive excessive amounts under the arrangements 26 The practice staff involved in the repeat dispensing arrangements should be competent to issue the prescriptions Relevant repeat authorizations (RA) and repeat dispensing (RD) prescriptions should be banded together in a “set”, once produced. Once the RA is signed the RA and RD prescriptions should be kept in “sets” stored in such a way to prevent unauthorized access. All the security considerations for ordinary repeats should apply to RA and RD “sets” (See 2.6 in the policy) It is essential to communicate any changes in medication to the patients chosen dispensing pharmacist Practices should have a system in place to act on any communications from dispensing pharmacists regarding medicines on repeat dispensing RA and RD prescriptions. Community pharmacists have to be accredited before they can take part in the repeat dispensing arrangements-those pharmacies taking part are listed here: http://intranet.pct.xwalsall.nhs.uk/Medman/Repeat_Dispensing.asp For more information go to: http://www.dh.gov.uk/en/Healthcare/Medicinespharmacyandindustry/Prescriptions/ DH_4000157 Appendix 6 Practice Manager’s Responsibilities Practice managers need to ensure that repeat prescribing process is practical, efficient and clearly understood by all involved including patients and community pharmacists. There should be an individual practice Repeat Prescribing and Medication Review Policy based on this document. 1 Patient Education 27 GP practices should have a patient leaflet explaining the Repeat prescribing system specific to the surgery It is important to clearly explain the Practice’s repeat prescribing process to patients. This will help patients to understand how the process works, which will aid in reducing the number of inappropriate request, drug wastage, and errors Patients should be informed of the repeat dispensing arrangements if or when the practice offers the service Display posters to highlight and remind patients about the repeat prescribing process Provide leaflets that explain the various aspects of the process in clear and simple terms Ensure that the information is specific to your practice’s repeat prescribing process 2 Policy for uncollected prescriptions There should be a standard time limit for the collection for signed prescriptions after which those not collected should be investigated, e.g. a medication review with the practice pharmacist. 3 Staff Training Practice staff involved in the repeat prescription process should be appropriately trained on, the practice protocols for repeat prescribing, the practice protocols for the repeat dispensing arrangements, what their responsibilities are and the need for accuracy. This training should be ongoing and is particularly important for new staff members. Practice pharmacists can provide the medicines management aspects of this training. Ensure that sufficient, adequately trained staff are available to cover sickness, holiday, sudden departures, etc 28 4 Community pharmacists Community pharmacists should have telephone access to doctors. There should be a set procedure for community pharmacists to contact the doctors to discuss urgent and non-urgent matters (e.g. telephone at a certain time or leave a message at reception). 5 Monitoring The repeat prescribing process should be monitored regularly, providing guidance when needed and regulated for signs of fraud. There should also be a system of checking a patient’s compliance with the prescribed treatment. 6 Security A robust system for the secure storage of prescriptions pads should be in place. Signed repeat prescriptions should be stored in a way that prevents unauthorized access. See Security of Prescription Form Guidance from The NHS Business Services Authority-Security Management Service available at: http://www.nhsbsa.nhs.uk/PrescriptionServices/Documents/PPDPrescripti onFormProductArea/security_prescriptions.pdf 7 Recall system There should be a recall system within the overall repeat prescribing policy that is clear to staff, doctors and patents alike and sufficiently flexible to meet the clinical needs. 8 Auditing Review and audits of the repeat prescribing process should be undertaken regularly. A built-in quality assurance mechanism should be incorporated into the repeat prescribing system to monitor: overprescribing, under prescribing and review of prescribing. Auditing the Repeat Prescribing System The repeat prescribing system should be audited on a regular basis Examples of how the repeat prescribing process can be audited are: 29 The number of new repeat items that are linked to a diagnosis The number of patients who have had an annual medication review as a percentage of the total requiring review over the last 12 months (using a sample size of 100) The number of patients over 75 who are on four or more medications reviewed in the last 6 months as a percentage of those patients over 75 years who are on four of more medications The percentage of repeat prescriptions without specific dosage instructions Auditing the number of repeat prescriptions that have been synchronized Auditing how accurately patient’s medical records are updated Surveying patients to ascertain how well they understand the repeat prescribing process e.g. A questionnaire given to patients when they collect their repeats. Additionally, specific therapeutic areas can be audited. For example: Monitoring patients taking drugs that have a narrow therapeutic index e.g. lithium, amiodarone, methotrexate or theophylline Auditing statin usage or the prescribing of two anti-platelets according to current clinical evidence 30