edema vs. lymphedema
Edema and Lymphedema
Articles
Edema and Lymphedema: Are They Different?
Implications for Bodyworkers
By Kalyani Premkumar
Originally published in Massage & Bodywork magazine, December/January 2005.
Copyright 2005. Associated Bodywork and Massage Professionals. All rights reserved.
"My legs get swollen at the end of the day."
"When I got caught in a hailstorm, I got hit on the head, and there was this huge swelling on my forehead."
"This swelling in front of my neck has been there for more than a month."
"After surgery for breast cancer, my right arm started swelling up."
Do these complaints sound familiar? Swelling is one of the complaints frequently encountered by bodyworkers when working with clients.
But are all four clients referring to the same thing? Can the term "edema" be used interchangeably with swelling? Which of them has edema? Who doesn't? Who has lymphedema?
According to the Stedman's Medical Dictionary for the Health Professions, swelling refers to enlargement (e.g., protuberance or tumor).
1
So the right term has been used by all four clients. This article will help you distinguish between edema and lymphedema, factors responsible for their formation, the treatment options available, and the implications for bodyworkers.
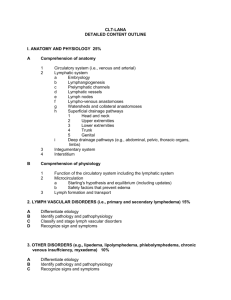
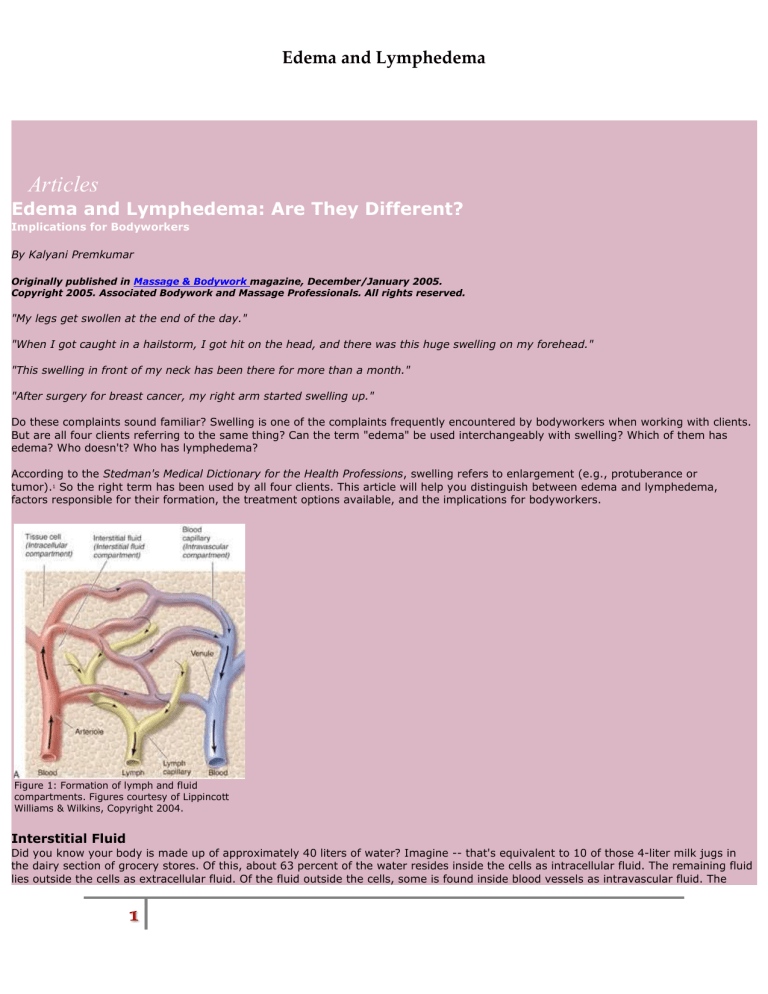
Figure 1: Formation of lymph and fluid compartments. Figures courtesy of Lippincott
Williams & Wilkins, Copyright 2004.
Interstitial Fluid
Did you know your body is made up of approximately 40 liters of water? Imagine -- that's equivalent to 10 of those 4-liter milk jugs in the dairy section of grocery stores. Of this, about 63 percent of the water resides inside the cells as intracellular fluid. The remaining fluid lies outside the cells as extracellular fluid. Of the fluid outside the cells, some is found inside blood vessels as intravascular fluid. The
1
Edema and Lymphedema remaining fluid (approximately 30 percent) is distributed between the cells as interstitial fluid (See Figure 1). When abnormal levels of interstitial fluid accumulate, it is called edema.
In order to understand edema, we need to consider the various factors responsible for moving fluids in and out of blood vessels into the interstitial fluid compartment.
Interstitial fluid is fluid that has leaked out of blood capillaries. Capillaries have thin walls (one cell thick) with variable gaps between endothelial cells. Structurally leaky, it is easy for fluid and other small particles to move out of them into the interstitium. But the gaps are too small for blood cells to exit. The interstitial fluid has a similar composition to that of blood -- except for cells and large proteins. In addition to the permeability of capillaries, other forces play an important part in fluid movement.
To help you understand these forces, the movement of water in a garden hose can be used as an analogy. Imagine a hose with holes punctured along its length. If you open the tap connected to the hose, the pressure of water would push it out through the holes. If you clamp one end of the hose without opening the tap further, it will result in the damming up of water before the clamp. More fluid would leak out of the holes in this case, too. If the hose is the capillary (the holes -- the gaps in the capillaries and the water), then pressure in the hose is the capillary hydrostatic pressure.
In our body, if arterioles dilate, more blood flows through capillaries and the hydrostatic pressure increases, forcing fluid into the interstitial compartment. This is what happens when you are stung by a bee and you see redness (increased blood flow) and swelling
(edema) at the site.
In situations where venous drainage is hampered -- as in varicose veins -- there is damming up of blood in the venules and capillaries.
This situation also increases hydrostatic pressure with resultant edema.
Hydrostatic pressure is not the only force that determines how much fluid moves into the interstitial compartment. The osmotic pressure, primarily exerted by the plasma proteins, plays an important part, too. If you consider the capillary wall as a semipermeable membrane that allows water to pass through but not large particles, then the number of particles inside and outside the capillaries will exert osmotic forces. As you may recall, osmosis is the movement of water from an area of lower concentration of particles to an area of higher. The particles inside the capillaries therefore draw water into the capillaries while the particles in the interstitium exert their forces outward.
The fluid in the interstitial region also exerts some hydrostatic force. This pressure would try to push fluid back into the capillaries. Thus, there are four forces determining the direction of fluid moving in or out of the capillaries:
- The capillary hydrostatic pressure -- pushes fluid out of the capillaries.
- The interstitial hydrostatic pressure -- pushes fluid into the capillaries. In the body, generally the interstitial hydrostatic pressure is negative (this is like having a suction pump around the capillary). This means that the negative interstitial hydrostatic pressure actually helps draw fluid out of the capillaries.
- The capillary osmotic pressure -- draws fluid into the capillaries.
- The interstitial osmotic pressure -- draws fluid out of the capillaries.
If the net outward force is greater than the inward force, more fluid moves out of the capillaries. Therefore any condition that results in increasing the outward force would result in edema. You may notice edema in your legs if you have been standing still for a long time.
Why? By gravity, blood pools in the leg veins. This increases the capillary hydrostatic pressure and the outward force is increased -- edema. Edema may be observed in protein deficiency malnutrition. Why? There is less plasma protein, resulting in a decrease in the capillary osmotic pressure. This reduces the inward force and the net outward force becomes greater, more fluid moves out -- edema.
Generally, at the arterial end of the capillary, fluid moves out. At the venous end of the capillary, the forces change and fluid moves into the capillary. But the fluid moving into the capillary at the venous end is less than that which moves out at the arterial end. This excess fluid in the interstitium has to be taken back into the circulatory system. The lymphatic system helps to do so.
2
Edema and Lymphedema
Figure 2: Structure of a lymph capillary.
The Role of the Lymphatic System
The lymphatic system consists of tiny capillaries that begin as blind-end tubes in the interstitial compartment. These vessels are found in almost all vascularized tissue. The walls of the capillaries are thin -- just one cell thick. Gaps in the walls allow excess interstitial fluid to enter the lymphatic capillaries (See Figure 2). Elastic fibers known as anchoring filaments connect the lymph capillary endothelial cells to the surrounding connective tissue fibers. The anchoring filaments help open and close the gaps in the wall.
The lymphatic capillaries join with others and flow into larger lymph vessels referred to as pre-collectors and collectors. These lymph vessels resemble those of the circulatory system and have smooth muscles in their walls. At regular intervals, they have one-way valves -
- folds of endothelium -- which prevent back flow of lymph. The pressure inside lymph vessels is very low and ranges between 0 to 1 millimeters of mercury during relaxation to 3 to 5 millimeters of mercury during contraction.
Lymphatic circulation may be considered to be made up of two parts -- the superficial circulation found in the junction of the dermis and epidermis and the deep circulation found in skeletal muscle beneath fascia and the viscera. Both circulations carry lymph toward the heart. The superficial circulation is divided into different drainage areas called lymphotomes, and the line between any two adjoining areas is called a watershed. Anastomotic connections exist between watersheds and if drainage is poor in one watershed, lymph flow can get diverted to adjacent ones.
2
At various points, the lymph vessels open into lymph nodes. The lymphocytes present in the lymph nodes screen the lymph and destroy foreign substances such as germs and toxins that may be present.
The lymph vessels ultimately open into large ducts -- the thoracic duct and right lymphatic duct which in turn open into neck veins. The right lymphatic duct drains lymph from the right side of the head, neck and chest, and right upper limb. The lymph from the rest of the body drains into the thoracic duct. This way, the excess fluid that tends to collect in the interstitial compartment is taken back to the circulation. If the lymph drainage is inadequate, fluid accumulates in the interstitial compartment and edema results. The type of edema that results from inadequate lymph drainage is referred to as lymphedema.
Composition of Lymph
As mentioned, lymph is primarily made up of the excess fluid from blood capillaries. It is typically clear, slightly more watery than blood.
Its composition varies depending on the tissues. For example, due to the high fat content, it appears whitish in the intestines soon after a meal. Some of the constituents of lymph include proteins (that have leaked from the blood capillaries), white blood cells (lymphocytes and macrophages), toxins, bacteria (if they have gained entry), bits of cell debris, enzymes, hormones, and gases, among others. It has been estimated that in one day about 75 to 100 grams of proteins and about 1.5 to 3.5 liters of fluid escapes into the interstitium. If the lymphatic system stopped moving the excess fluid and leaked proteins back into the circulatory system, the body would develop severe edema and death would result in 24 to 48 hours.
3
Factors that Assist with Lymph Flow
Many factors assist with lymph flow. Of these, the intrinsic ability of the smooth muscles in the walls of lymph vessels seems to play a primary role. Studies have shown that the smooth muscles in the vessel walls located between any two valves contract rhythmically -- as if they had pace makers -- at the rate of 5 to 8 contractions per minute at rest.
4
They may contract at 20 to 30 times this rate during exercise and/or when stimulated by autonomic nerves. These smooth muscles are also affected by hormones, stretch of vessel wall (as may happen when there is more interstitial fluid), and chemicals in the local environment.
Apart from the intrinsic ability of lymph vessels to contract, respiration is another factor that facilitates lymph flow. The negative pressure created in the thoracic cavity during inspiration draws lymph fluid upward. The pulsation of arteries flowing parallel to lymph vessels,
3
Edema and Lymphedema contraction of skeletal muscles, peristalsis of smooth muscles of the intestines, movement of limbs and external compression (clothes, etc.), presence of valves, and presence of anchoring filaments (that helps open gaps in lymph capillaries when there is more fluid in the interstitium) are other factors that affect flow of lymph. Lymphedema results when lymph flow does not match lymph production.
Figure 3: Filariasis of the left leg, also known as elephantiasis, is caused by threadlike filarial worms transmitted into the blood by mosquitoes. The worms and inflammatory reactions to the parasite block lymphatic flow in different areas causing lymphedema.
Causes of Lymphedema
Clinically, lymphedema is classified as primary and secondary. Primary lymphedema is due to congenital malformations in the lymphatic system such as defective valves or vessels. Secondary or acquired lymphedema, a more common condition, is due to problems with the lymphatic system that occur after birth. Some of the common causes are surgery involving removal of lymph nodes and vessels (e.g., cancer surgery), radiation therapy, spread of cancer to lymph vessels and nodes, scarring of lymph vessels and nodes following infections, and trauma. In developing countries, a common cause of secondary lymphedema is a type of parasitic infestation known as filariasis (See Figure 3).
Consequences of Lymphedema
As fluid accumulates in the interstitium, damage is caused to the surrounding tissue.
5
The swelling may compress the delicate lymphatic vessels and veins, promoting further damming up of fluid. The skin cells are pushed farther from the underlying blood capillaries that supply nutrients needed for metabolism. This in turn makes the skin more prone to infection and slows down healing after injury. With time, non-healing ulcers may form, and fibrous changes that may occur worsen the situation. Edema near joints may restrict movement and thereby decrease muscle strength and function. Postural abnormalities may follow. Sensory changes such as feelings of heaviness, aching, and paraesthesias due to compression of nerves may be present. Heaviness of limb may worsen joint ailments if present.
Functional impairments make it difficult for individuals to do normal day-to-day activities and psychological problems such as depression and anxiety are not uncommon. Such impairments have greater effects if the person is elderly.
How is Lymphedema Diagnosed?
Unfortunately, there is no objective tool that helps with accurate diagnosis of lymphedema. At present, it is diagnosed based on clinical observation and thorough history. Ultrasound, magnetic resonance imaging, and computed tomographic imaging may help identify structural changes. Lymph angioscintigraphy, or isotopic lymphoscintigraphy, is a test that may be used to visualize the lymphatic system. Here, a radiolabeled protein molecule is injected into the web space of the hand or foot, and the movement of the protein is monitored over time using special cameras. A newer technique, multiple frequency bioelectrical impedance analysis, may be used to diagnose lymphedema. In this technique, the resistance encountered by a small electric current as it passes through extracellular and intracellular fluid is measured and used to calculate fluid volume in each compartment. Sometimes, the difference in the circumference of
4
Edema and Lymphedema the two limbs (measured at specific points), or a comparison of the volume of water displaced when each of the limbs are immersed in water, may be used for diagnosis and monitoring the effect of interventions. Tonometry may also be used, it measures the pressure required to indent the skin to a specific depth.
How is Lymphedema Treated?
Lymphedema, caused by impaired transportation of lymph, is unfortunately a chronic condition that can only be managed, not cured. A number of interventions are used for managing lymphedema. They include patient education, skin care, compression bandaging, compression garments, compression pumps, exercises, and manual lymphatic drainage. The combination of treatment interventions is known as decongestive lymphatic therapy.
6
Patients are educated about the cause of lymphedema and precautions that could be taken to maintain the health of skin and prevent skin infections. The area may be compressed using a multilayer bandaging technique. First a cotton stockinette is used, over which a padding layer is applied, followed by a low stretch bandage. The bandage is applied so that there is a pressure gradient, with greater pressure distally. Initially, the bandage is worn 22 to 24 hours for two to three weeks.
Compression garments are usually used to maintain the girth reduction achieved by bandages. These are available off the shelf or may be custom fitted and are classified from class I (least) to class IV based on the pressure exerted. With the availability of newer techniques such as manual lymphatic drainage and compression bandaging, use of compression pumps has become a secondary option. Here, a sleeve with multiple cuffs is applied over the edematous limb and compressed air is sent into the sleeve. By systematically inflating and deflating the various cuffs, pressure is applied to the subcutaneous tissue in a wave-like pattern.
7
Elevation and other exercises using special equipment are recommended to promote lymph drainage. However, it is best for clients with lymphedema to follow individualized exercise programs developed by physical therapists.
Manual Lymphatic Drainage is a specialized massage technique originally developed by Emil Vodder, a Danish massage practitioner and doctor of philosophy.
8
The techniques help clear edema by facilitating lymph flow through collaterals across watersheds and collecting ducts. Since pressure is very low in lymph vessels, lymph drainage techniques resort to very gentle stretches of the skin, superficial fascia, and the lymphatic vessels in the direction of lymph flow, followed by gentle release of the stretch. Superficial effleurage and superficial lymph drainage techniques are used to remove fluid and assist further drainage, and kneading strokes may be used to soften the hardened tissue.
9
Newer developments by French physician Bruno Chikly, specifically lymph drainage therapy, have improved some of these techniques.
10
Here, practitioners are trained to manually identify with the various qualities of lymph flow such as rhythm and pressure and
"map" the superficial and deep lymphatic pathways (manual lymphatic mapping).
11
A thorough knowledge of the lymph drainage patterns is necessary for the technique to be effective. Initially, the proximal areas are massaged to facilitate drainage from distal areas. This is followed by draining the distal areas. The sequence of strokes is repeated many times. Following massage, the area is bandaged using low-stretch bandages to increase tissue pressure, support the connective tissue, and maintain the reduction in girth achieved.
Implications for Bodyworkers
The most important concept that bodyworkers need to understand is that edema is just a symptom or sign, and there are various causes of edema. When edema is caused by inadequate lymph drainage, it is referred to as lymphedema. While there are many studies that have proven the positive effects of manual therapies such as manual lymph drainage and massage on lymphedema, it should not be assumed that massage is indicated for all types of edema.
12,13
If the edema is generalized, it is usually due to chronic cardiac, kidney, or liver problems, and massage may be detrimental.
14
Consultation with an attending physician may be necessary. If the edema is due to causes other than this, massage may be beneficial.
It is important for bodyworkers to obtain a detailed history about the onset, duration, cause, previous treatments such as physiotherapy, radiotherapy, chemotherapy, surgery, and medications, skin infections, and loss of function, as all these factors can affect treatment protocol. Assessment of the hardness of the edema, condition of the skin and nails, and restriction to active and passive movement brought about by the condition are also important. In edema in a hemiplegic limb, sensations may be diminished or absent, and this should be taken into account. Based on these findings and later, according to improvements observed in the client, the therapist should be open to modifying the treatment plan.
During treatment, the client should be positioned with the edematous limb supported and elevated. Elevation for 10 to 15 minutes before treatment may reduce edema by capitalizing on the effect of gravity. Strokes should follow the direction of lymph in the area (e.g., in the
5
Edema and Lymphedema upper limbs -- toward the axilla, in the chest -- toward neck and axilla of respective side, in the legs -- toward the inguinal region).
Proximal areas are treated first, followed by distal areas. Passive and active movements may be used after the massage to assist both the venous and lymphatic flow. Often, in clients with chronic edema, organization of the proteins in the interstitial region results in fibrosis and thickening of the skin and connective tissue. Here, friction movements may be used to stretch and release adhesions. The therapist should understand that though visible reduction in the size of the treatment area may not be seen, massage helps relieve many of the symptoms. Initially, more frequent sessions may be required (e.g., three to five times/week). When girth reduction is stable, sessions may be tapered off. Clients may also be taught self-massage techniques. For greater effect, drainage therapies should be combined with other forms of interventions.
Lymphedema management is a time-consuming process that requires a lot of patience and flexibility on the part of the bodyworker.
However, the significant benefits provided by way of improved function and decreased disfigurement should be enough gratification for any wholistic practitioner.
Now go back to the beginning of the article. Which of the four clients has edema? Who doesn't? Who has lymphedema?
Kalyani Premkumar, a physician and certified massage therapist, is an adjunct assistant professor, Faculty of Medicine, University of
Calgary and an instructor at the Center for Complementary Health Education, Mount Royal College, Calgary, Canada. She is the author
of The Massage Connection -- Anatomy and Physiologyand Pathology A to Z -- A Handbook for Massage Therapists.
References
1 Stedman's Medical Dictionary for the Health Professions. 27th edition. Baltimore: Lippincott Williams & Wilkins, 2000.
2 Foldi, M. Anatomical and physiological basis for physical therapy of lymphedema. Experientia 1978,33(suppl):15-18.
3 Guyton, AC, Granger, HJ, and Taylor, AE. Interstitial fluid pressures. Physiol Rev 1971, 51:527-563.
4 Chikly, B. Silent Waves -- Theory and Practice of Lymph Drainage Therapy. Arizona: IHH Publishing, 2002.
5 Konecne, SM and Perdomo, M. Lymphedema in the elderly: A special needs population. Topics in Geriatric Rehabilitation
2004,20(2):98-113.
6 Ibid.
7 Premkumar, K. The Massage Connection -- Anatomy and Physiology. Baltimore: Lippincott Williams & Wilkins, 2004.
8 Chikly, B.
9 Andrade, CK and Clifford, P. Outcome-based massage. Baltimore: Lippincott Williams & Wilkins, 2001.
10 Chikly, B.
11 Ibid.
12 Haris, R and Piller, N. Three case studies indicating the effectiveness of manual lymph drainage on patients with primary and secondary lymphedema using objective measuring tools. Journal of Bodywork & Movement Therapies 2003,7(4):213-21.
13 Sitzia, J, Sobrido, L, and Harlow, W. Manual lymphatic drainage compared with simple lymphatic drainage in the treatment of postmastectomy lymphoedema: a pilot randomized trial. Journal of Traditional Chinese Medicine 2002,88(2):99-107.
14 Premkumar, K. Pathology A to Z -- A handbook for massage therapists. 2nd Ed. Calgary: VanPub Books, 1999.
6