Warrnambool Out of Hours Radiology
advertisement
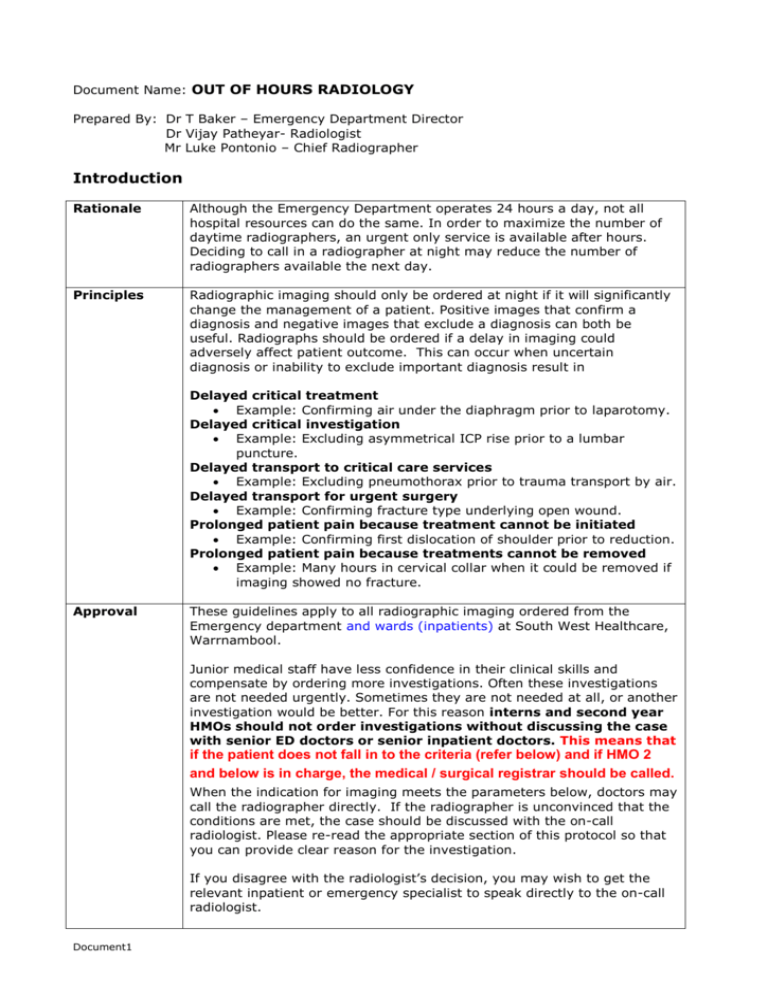
Document Name: OUT OF HOURS RADIOLOGY Prepared By: Dr T Baker – Emergency Department Director Dr Vijay Patheyar- Radiologist Mr Luke Pontonio – Chief Radiographer Introduction Rationale Although the Emergency Department operates 24 hours a day, not all hospital resources can do the same. In order to maximize the number of daytime radiographers, an urgent only service is available after hours. Deciding to call in a radiographer at night may reduce the number of radiographers available the next day. Principles Radiographic imaging should only be ordered at night if it will significantly change the management of a patient. Positive images that confirm a diagnosis and negative images that exclude a diagnosis can both be useful. Radiographs should be ordered if a delay in imaging could adversely affect patient outcome. This can occur when uncertain diagnosis or inability to exclude important diagnosis result in Delayed critical treatment Example: Confirming air under the diaphragm prior to laparotomy. Delayed critical investigation Example: Excluding asymmetrical ICP rise prior to a lumbar puncture. Delayed transport to critical care services Example: Excluding pneumothorax prior to trauma transport by air. Delayed transport for urgent surgery Example: Confirming fracture type underlying open wound. Prolonged patient pain because treatment cannot be initiated Example: Confirming first dislocation of shoulder prior to reduction. Prolonged patient pain because treatments cannot be removed Example: Many hours in cervical collar when it could be removed if imaging showed no fracture. Approval These guidelines apply to all radiographic imaging ordered from the Emergency department and wards (inpatients) at South West Healthcare, Warrnambool. Junior medical staff have less confidence in their clinical skills and compensate by ordering more investigations. Often these investigations are not needed urgently. Sometimes they are not needed at all, or another investigation would be better. For this reason interns and second year HMOs should not order investigations without discussing the case with senior ED doctors or senior inpatient doctors. This means that if the patient does not fall in to the criteria (refer below) and if HMO 2 and below is in charge, the medical / surgical registrar should be called. When the indication for imaging meets the parameters below, doctors may call the radiographer directly. If the radiographer is unconvinced that the conditions are met, the case should be discussed with the on-call radiologist. Please re-read the appropriate section of this protocol so that you can provide clear reason for the investigation. If you disagree with the radiologist’s decision, you may wish to get the relevant inpatient or emergency specialist to speak directly to the on-call radiologist. Document1 It should not be assumed that non urgent imaging should be performed out of hours purely because the Radiographer is already on the premises. If there is an x-ray examination (that is not the primary reason for the call in) that you feel should be performed, it should be discussed with the Radiographer. It will be performed if deemed suitable. Atypical cases You may feel that a patient with a situation not covered by this guideline also requires imaging. Discuss these patients with the radiographer, or, if necessary, the on-call radiologist. Business Hours Monday to Friday 8:30AM to 5:00PM – Ultrasound and MRI 8:30AM to 9:00PM – CT and X-rays Weekends and public holidays 9:00AM to 5:30PM – CT and X-rays There is no MRI service available outside these hours. CT, ultrasound and X-rays can be ordered out of hours as described in these guidelines. Three points are particularly important for our service at Warrnambool There are only two full-time sonographers. All requests for ultrasound must be considered very carefully so that the service remains viable. If a radiographer is called in after 1 AM, they will not be available to work the next morning. If at all possible, delay films needed in the early hours of the morning until 8:30 AM. Consider carefully your decision to have a CT scan performed, the patient dose for these scans are significantly higher than that of a plain film x-ray (CTPA is approximately equivalent to 300-400 chest x-rays). Also the IV contrast media is nephrotoxic in nature so should only be administered to patients with healthy renal function (eGFR > 60). Contact Number To speak to the radiologist-on call, ring switchboard and ask to be directed to the radiologist-on call. Clearly spell out that you are not looking for the radiographer or sonographer. Approved Indications by modality Urgent indications for ultrasound 1) 2) 3) 4) 5) Acute limb ischemia Paediatric trauma Ectopic pregnancy ( after +ve pregnancy test & bhcg ) Suspected ovarian torsion Suspected testicular torsion. Urgent indications for CT 1) CT brain for stroke, bleed or trauma. 2) Acute abdomen 3) Abdominal trauma Approved indications by system Respiratory It can be difficult to diagnose the underlying cause for a patient’s respiratory distress. As treatments can be quite different (diuretics, anticoagulants, bronchodilators), it is important to make the diagnosis as soon as possible. Certain diagnoses (such as pneumothorax or large pleural effusion) can be treated immediately if they can be confirmed. Discussion with senior ED staff or inpatient registrars before deciding to order a film is good practice. Urgent radiology is indicated for Shortness of breath of uncertain diagnosis with any of the following Increased work of breathing Tachypnoea New hypoxia (saturation <95%) Possible pneumothorax Possible thoracic dissection Possible large pleural effusion requiring urgent aspiration (and post aspiration film also) Urgent radiology is seldom indicated for Shortness of breath where the patient is not in respiratory distress. Example: Probable mild to moderate pneumonia Shortness of breath where the diagnosis is certain and the patient is improving Example: Acute asthma Possible pulmonary embolus where the patient is stable Unless the patient has a high risk of bleeding, the patient can be anticoagulated and imaged the next day. Trauma Warrnambool is designated as a Regional Trauma Service in Victoria’s Trauma system. It is tasked to provide resuscitation and stabilisation of major trauma patients prior to their transfer to a trauma centre, as well as definitive care of less severe injuries. Delayed diagnosis of head injury or acute bleeding increases the likelihood of an adverse outcome. Urgent radiology is indicated for: Any trauma meeting major trauma criteria http://docs.health.vic.gov.au/docs/doc/9382EC200E82017BCA25784000739B2 2/$FILE/Prehospital%20triage%20Victorian%20State%20Trauma%20Committe e%202010.pdf Head injury with any of the following Focal neurology Glasgow Coma Score <14 (even if possibly due to intoxication) Suspected skull fracture Anticoagulant use (will need rescan at 24 hours also) Neck injury with any of the following Focal neurology Severe neck pain Inability to maintain c-spine precautions due to poor patient compliance Significant patient discomfort due to hard collar when delay in imaging is likely to be many hours Chest trauma with any of the following Respiratory distress Hypoxia Significant pain Significant chest wall or sterna tenderness Abdominal trauma with any of the following Rebound or guarding Hypotension or tachycardia Macroscopic haematuria Pelvic Trauma with Pain on pelvic springing Abdominal Urgent radiology is seldom indicated for Mild symptoms in low impact injury Intoxicated patients (GCS14) tolerating a collar where intoxication precludes collar removal, even if CT clear. Unless the diagnosis under consideration is likely to require immediate surgery, imaging can be delayed. If the patient is unstable, immediate surgery may be more appropriate. Early discussion with the surgical unit is good practice. Urgent radiology is indicated for Acute abdomen Obtain surgical advice. Immediate transfer or operation may be a better option. Possible organ rupture Possible volvulus Possible leaking aortic aneurysm Possible ectopic pregnancy Please confirm pregnancy and discuss with gynaecology registrar first. Urgent radiology is seldom indicated for Abdominal pain with localized abdominal signs Orthopaedic Most patients with limb fractures can be made comfortable with splinting and analgesia. They can return the next day for x-ray. Even moderately displaced fractures are unlikely to be operated on after hours. They should also be splinted, but the patient may need to remain in hospital until x-ray is available the next morning. Urgent radiology is required for Open fractures Fractures with significant limb deformity or neurovascular compromise. Possible dislocation, if immediate relocation is possible It is preferable if a post-reduction film can also be done if the patient could then go home. Patient with recurrent shoulder dislocation may sometimes be relocated without x-ray. Possible cauda equine syndrome Urgent radiology is seldom indicated for Mild or moderately displaced fractures with little chance of neurovascular problems. Suspected fractures Neurological Urgent radiology is indicated for Cerebrovascular accident with any of the following Time since symptom free < 4.5 hours Possible intra-cerebral bleed Example: associated anticoagulant, hypertension headache GCS < 14 Deterioration Focal seizures Prior to lumbar puncture Discuss with ED consultant, paediatric, or medical registrar. CT is not always needed, especially for children. Urgent radiology is seldom indicated for Transient ischaemic attack, if symptoms resolved Post seizure, if patient is returning to normal GCS Syncope, without focal neurology or abnormal vital signs Other In general, intensive care patients should not have their imaging delayed. Urgent radiology is indicated for Patients being transferred to a critical care bed or for urgent surgery Example: Post central venous line placement Patients requiring anticoagulation, but require exclusion of bleeding Example: Possible pulmonary embolus and altered mental state – exclude intracerebral bleed. Urgent imaging is seldom required for Possible acute coronary syndrome, if chest is clear and the patient is not being transported Possible deep venous thrombosis if patient is safe to be anticoagulated. Patient can receive low molecular weight heparin until the next day. If that day is a weekend or public holiday, discuss the case with the medical unit. Peripheral foreign bodies