Department of Physiology Safety & Health
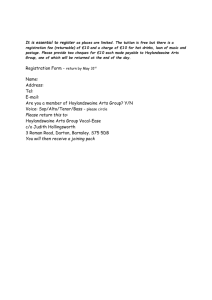
advertisement

Department of Physiology
Procedure No:
PHY/SOP/RE01
Revision No:
001
Title:
Effective Date :
16/6/2010
Safe handling of biological materials
(Adopted from OSHE/SOP/BS/10)
Page:
Page 1 of 9
Safety & Health
Laboratory (Location):
Cytokine biology Lab, MD9
Prepared/Review By
Approved By
Next Review Date
Oh Chu Yun
Dr. Leung Pui Lam Bernard
16/6/2013
* Review Date = Future date for the next revision (every 3yrs)
1.0 OBJECTIVE
This procedure provides guidance for personnel safety when handling or being exposed to
biological agents. Its purpose is to protect researchers, the University community and its assets,
and the environment by assuring the safe use and storage of potentially hazardous biological
material in Department of Physiology.
2.0 SCOPE
The procedure is applicable to all Department of Physiology laboratories where biological
materials are used or stored in the course of work. All staff and students are to adopt the
practices in the procedure.
3.0 RESPONSIBILITIES
3.1 Head of Department/ Principal Investigator
Principal Investigators (PI) and Head of Department (HOD) shall be responsible for ensuring
that this SOP is disseminated to all laboratory personnel and that they are aware of the
procedures to take for safe handling of biological hazards. The PI is responsible for providing or
arranging the appropriate training of personnel.
3.2 Laboratory personnel
All laboratory personnel (staff and students) working with infectious agents or potentially
infected materials must be aware of potential hazards, and must be trained and proficient in the
practices and techniques required to handle such material safely.
Department of Physiology
Procedure No:
PHY/SOP/RE01
Revision No:
001
Title:
Effective Date :
16/6/2010
Safe handling of biological materials
(Adopted from OSHE/SOP/BS/10)
Page:
Page 2 of 9
Safety & Health
Laboratory (Location):
Cytokine biology Lab, MD9
4.0 DEFINITION
Biological materials – any one type or combination of live, frozen or lyophilized material that
includes the following:
1. Human cell line (including non-human primates)
2. Non-human cell line
3. Human or other primate material (fluid, tissue, etc.)
4. Non-primate animal material (fluid, tissue, etc.)
5. Recombinant DNA
6. Bacteria
7. Virus
8. Fungus, parasite, or other live material
9. Rickettsia
10. Chlamydia
Biohazard - possessing the potential to produce an infection or genetic alteration in humans,
animals or plants.
Biohazard materials- may include but are not limited to: bacteria, fungi, viruses, rickettsiae,
chlamydiae, parasites, recombinant products, allergens, cultured human or animal cells and the
potentially infectious agents these cells may contain, viroids, prions and other infectious agents.
Biohazard materials do not include live animals that are healthy and presumed to be
noninfectious, but do include unhealthy animals that are known or suspected to be infectious.
Biological materials are not considered to be potentially hazardous when they have been
chemically, thermally, or otherwise treated to render them permanently non-viable/ permanently
inactivated/ permanently incapable of insertion or infection into living cells.
5.0 PROCEDURE
Safe handling of biological materials in the laboratory
Major biohazards associated with laboratory work are infections with pathogenic
microorganisms such as viruses, parasites or bacteria that are either being study in the
laboratory, or present as contaminants in blood, serum, body fluids, cell lines and tissue
samples under analysis.
Improper storage, handling or transport of biological materials in the laboratory poses a risk of
infection to the personnel involved.
5.1 Receipt
a. Personnel who receive and unpack biological materials should be aware of the potential
health hazards involved and the appropriate safety precautions to be taken, particularly
when handling materials derived from human or primates.
Department of Physiology
Procedure No:
PHY/SOP/RE01
Revision No:
001
Title:
Effective Date :
16/6/2010
Safe handling of biological materials
(Adopted from OSHE/SOP/BS/10)
Page:
Page 3 of 9
Safety & Health
Laboratory (Location):
Cytokine biology Lab, MD9
b. Before opening any package, read the safety information that usually accompany the
commercially available products e.g. MSDS/product information sheets of cell lines and
microbial cultures. If in doubt, only open the package in a biological safety cabinet.
c. Wear disposable gloves during receipt of biological materials.
d. Keep supplies of an appropriate disinfectant available on hand.
e. Check for any leakage, cracks or breaks in the containers.
f. Wash your hands thoroughly with disinfectant soap after handling.
5.2 Storage
a. All biological materials to be stored must be clearly labeled with the scientific name, and/
or descriptions, date of storage and name of person who stored them to facilitate
identification. Autoclave and discard all unlabelled and obsolete items.
b. Expired and other unwanted material must be decontaminated properly.
c. Hazard warning signs (as shown below), indicating the biosafety level of the biological
material being used, must be posted on laboratory doors, cold rooms,
refrigerator/freezer doors and cryogenic tanks. Refer to “Lab Sign Posting and Labeling”
SOP (CBL/SOP/GS/05) for NUS’s standard for signage and labels.
d. Keep and maintain an inventory of refrigerator, freezer and cryogenic tank contents.
e. Regularly clean and disinfect refrigerators etc. in which biological cultures are stored.
5.2.1 Storage containers
a. Storage containers may be of glass or preferably plastic. They must be robust and
leak proof.
a. Visually inspect to ensure that no material should remain on the outside of the
container.
b. Product specification forms that accompany the biological materials should not be
wrapped around the containers but removed and filed appropriately. If they are to
accompany the biological material for example, during transport, place them in
separate, preferably waterproof bags/envelopes.
c. If a biohazard material is stored in a refrigerator or cold room, place it in a secondary
container large enough to contain the contents should the container break.
d. All secondary containers (plastic bags, bottles, boxes, bins etc.) used to store
biological materials must also be labeled clearly with the universal biohazard symbol
as shown below. Biohazard labels for secondary containers can be obtained from
OSHE.
e. Decontaminate all containers used for storage before reuse.
5.2.2 Storage of ampoules containing infectious materials
a. Storage of ampoules/cryovials in liquid phase nitrogen allows the lowest possible
storage temperature to be maintained with absolute consistency but create potential
hazards. If they are cracked or imperfectly sealed, contamination may occur via the
Department of Physiology
Procedure No:
PHY/SOP/RE01
Revision No:
001
Title:
Effective Date :
16/6/2010
Safe handling of biological materials
(Adopted from OSHE/SOP/BS/10)
Page:
Page 4 of 9
Safety & Health
Laboratory (Location):
Cytokine biology Lab, MD9
liquid nitrogen medium. They may also break or explode on removal due to a buildup of excessive pressure during thawing. For these reasons, ampoules containing
highly infectious materials should never be immersed in liquid nitrogen and should
preferably be non-glass materials.
b. If very low temperatures are required, store the ampoules in the vapor phase
nitrogen or deep freezers.
c. Wear full personal protective equipment (lab coat, full covered shoes, insulated
gloves and full-face mask) when removing ampoules from cold storage. Disinfect the
outer surfaces of ampoules when they are removed from storage.
5.3 General Safety procedures for handling of infectious materials
Whenever works with infectious agents is performed, all appropriate measures must be taken to
protect lab personnel and the environment. Safety measures to take includes the use of
engineering and administrative controls, but the most important element of containment is
prudent laboratory practices, standard microbiological techniques and common sense as
detailed below.
5.3.1 Avoiding dispersal of infectious materials by aerosol production
a. Aerosols are dispersions of airborne liquid or solid particles created by most laboratory
manipulations. Exposures to airborne microbial agents by inhalation are a major route of
infection. Examples of aerosol-producing activities in the laboratory:
a. shaking or vortexing tubes, stirring
b. sonicating, homogenizing, blending, grinding, cell disruption with French press
c. opening lyophilized cultures, opening snap top tubes, opening ampoules
d. breakage of culture containers
e. flaming loops or slides
f. pouring liquids
g. centrifugation steps e.g. Opening/ filling centrifuge tubes, removing supernatant,
resuspending pellets, centrifugation itself and breakage of tubes during
centrifugation
h. blowing out pipettes
i. pulling needles out of septums, filling a syringe
j. intranasal inoculation of animals
k. cage cleaning, changing animal bedding
l. harvesting infected material from animals, eggs, and other virology procedures
b. Use measures that avoid the creation of an aerosol or reduce the extent of aerosol
formation routinely.
c. Conduct procedures that may produce infectious aerosols (eg. agitating, blending,
grinding) in a biological safety cabinet.
Department of Physiology
Procedure No:
PHY/SOP/RE01
Revision No:
001
Title:
Effective Date :
16/6/2010
Safe handling of biological materials
(Adopted from OSHE/SOP/BS/10)
Page:
Page 5 of 9
Safety & Health
Laboratory (Location):
Cytokine biology Lab, MD9
d. Vortexing/ Shaking/ Stirring - Keep containers properly sealed. Vigorous shaking will
create a heavy aerosol. To resuspend liquids e.g. cultures, use a swirling action to
create a homogeneous suspension with a minimum of aerosolization. Wait a few
minutes after the procedures before opening the container.
e. Blending - Use safety blenders, as although expensive, they are designed to prevent
leakage from the blender jar. Household blenders do not prevent the spread of aerosols.
See also OSHE SOP (OSHE/SOP/BS/11) on “Safe use of laboratory equipment”.
f. Opening culture tubes, plates, bottles and flasks - Immediately following shaking or
centrifugation, allow aerosols to settle for one to five minutes before opening the
containers. Manipulate slowly as films of liquid or dried infectious material may collect at
or near the rim/ neck of containers and may be dispersed into the air when disturbed.
Particular care is required when opening plates, tubes, or bottles containing fungi, as the
operation may release a large number of spores. Such cultures should be manipulated
in a biological safety cabinet.
g. Opening ampoules – Always open ampoules in a biological safety cabinet to control
any aerosol produced. To open a sealed-glass ampoule, nick the neck of the ampoule
with a file, hold the ampoule upright in a disinfectant-soaked paper towel to protect
hands, and snap it open at the nick. Reconstitute the contents of the ampoule by adding
liquid slowly to avoid aerosolization of the dried material. Exercise caution as sealed
glass ampoules stored in liquid nitrogen can explode on removal dispersing materials
into the atmosphere. Use alternatives e.g. polypropylene tubes / cryovials if possible to
eliminate this hazard.
h. Pouring of liquids- Never pour or decant liquids containing infectious agents e.g.
Bacteria cultures, virus suspensions. Aspirate off supernatants or use a mechanical
pipette.
i. Pipetting – Minimize the creation of bubbles in pipettes. Avoid vigorous pipetting and
mixing. Do not forcibly expel the last drop of liquid from a pipette. Discharge pipetted
material near the surface of fluid or down the wall of the container. See also OSHE SOP
(OSHE/SOP/BS/11) on “Safe use of laboratory equipment”.
j. Centrifuging- Use containment devices (e.g. BSCs, sealed canisters, safety cups or
buckets with covers, sealed tubes or sealed rotors, etc). Allow aerosols to settle for one
to five minutes before opening a centrifuge tube. See also CBL/SOP/03 on “Centrifuge
Safety”.
k. Lyophilizing - If possible, load samples in a biological safety cabinet. Use a vacuum line
trap or HEPA filter to protect the lyophilizer vacuum pump exhaust. Disinfect all surfaces
of the unit that have been exposed to the agent after lyophilization.
l. Sterilizing inoculating loops/needles - Use a hooded Bunsen burner, shielded micro
incinerator or glass bead sterilizer. If flaming the loop, avoid splattering by gradually
introducing the inoculating loop into the Bunsen burner; and allowing inoculating loops or
needles to cool before touching biological specimens. Alternatively, use disposable
sterile plastic loops and needles
Department of Physiology
Procedure No:
PHY/SOP/RE01
Revision No:
001
Title:
Effective Date :
16/6/2010
Safe handling of biological materials
(Adopted from OSHE/SOP/BS/10)
Page:
Page 6 of 9
Safety & Health
Laboratory (Location):
Cytokine biology Lab, MD9
m. Disinfecting spills- If a spill occurs that may generate aerosols, leave the area, close
the door, wait 30-60 minutes to allow dissipation of aerosols Do not spray disinfectant
onto liquid spills, as this will create aerosols. Instead swab the area with a paper towel
soaked with disinfectant over the work surface to kill any biohazard agents. Refer to
CBL/SOP/02 on “Biological Spill Response” for detailed procedures.
5.3.2 Avoiding contact of infectious materials with skin and eyes
Infectious agents can be introduced to the mucous membranes of eyes via splashes,
splatters or contact with contaminated fingers or other objects. These include viruses
and bacteria that can cause conjunctivitis (e.g., adenovirus, herpes simplex,
Staphylococcus aureus) and viruses that can cause systemic infections, including blood
borne viruses (e.g. hepatitis B and C viruses, human immunodeficiency virus), herpes
viruses, and rhinoviruses. Infectious agents can also be introduced via non-intact skin
(e.g. open wounds) from hands that have been in contact with a contaminated surface
(i.e. benches, phones, computers, equipment handles) or by failure to wash hands after
handling the agents.
a. Wear appropriate personal protective equipment (lab coats, gloves, eye protection
etc) at all times when handling infectious materials. Refer to SOP CBL/SOP/GS/07
for guidelines on selecting appropriate PPE.
b. Avoid touching any part of your body (skin, face, eyes, mouth etc) with your gloved
hands as infectious materials deposited on your hands can come into contact with
the area as a result.
c. Always remove personal protective equipment and wash your hands with
antibacterial soap and water before leaving the laboratory work area and other
restricted areas. Do not wear your lab coat or gloves outside of the laboratory into
public areas.
d. Wear proper covered footwear in the laboratory. Do not wear open-toed shoes or
sandals in the laboratory.
e. Cover up any open wounds with a plaster before starting work in the laboratory.
f. Do not use gloved hands to open doors or handle items (e.g. phones, computers)
that would be touched by someone not wearing gloves.
g. Replace disposable gloves as soon as possible if contaminated, torn, punctured or
damaged in any way.
h. Hands should be washed immediately with antiseptic soap after completion of any
procedure in which infectious material is used.
i. Do not handle contact lenses in the laboratory.
j. Wear suitable eye protection when performing procedures which may result in the
splashing of potentially infectious materials.
Department of Physiology
Procedure No:
PHY/SOP/RE01
Revision No:
001
Title:
Effective Date :
16/6/2010
Safe handling of biological materials
(Adopted from OSHE/SOP/BS/10)
Page:
Page 7 of 9
Safety & Health
Laboratory (Location):
Cytokine biology Lab, MD9
5.3.3 Avoiding injection of infectious materials
Infections can occur through intact skin via percutaneous/ sharps injuries causing accidental
inoculation of infectious materials.
a. As part 5.3.2a.
b. See SOP (CBL/SOP/07) on “Safe handling of sharps” for safety precautions.
5.3.4 Avoiding ingestion of infectious materials
a. As part 5.3.2a.
b. As part 5.3.2b.
c. As part 5.3.2c
d. Do not eat, drink or smoke in the laboratory or place any articles e.g. pen, pencil in your
mouth.
e. Do not store food or drinks in the laboratory premises, cold rooms, lab refrigerators, or
equipment. Similarly, do not bring biological materials into any premises where food and
drinks are consumed or stored.
f. Do not apply cosmetics in the laboratory.
g. Wear a face shield or surgical mask when performing procedures which may result in
the splashing of potentially infectious materials.
h. Do not pipette any materials by mouth. Use a mechanical pipetting device.
5.3.5 Safe handling of Human and Other Primate Cells and Tissues.
a. Laboratory-associated infections can occur from handling human or primate primary cell
cultures, human blood, body fluids or tissues. Examples of potential hazards include:
i.
HBV, HIV or other blood borne pathogens present in blood or body fluids,
ii.
Agents such as Mycobacterium tuberculosis that may be present in human lung
tissues
iii.
Cells transformed with viral agents, such as SV-40, EBV, or HBV
iv.
Cells carrying viral genomic material.
v.
Tumorigenic human cells that carry a risk of self-inoculation.
b. If your lab involves research using human blood, human cell lines (even vendorpurchased established human cell lines), or human tissue cultures you must employ
biosafety level 2 (BSL2) practices and procedures. This is consistent with the
recommended practices in CDC/ NIH booklet “Biosafety in Microbiological and
Biomedical Laboratories”.
c. Under the NUS Occupational Health program, laboratory personnel working with
materials of human origin are required to have immunization against Hepatitis B. See
section on “NUS Occupational health program requirements”.
d. Handle all human samples such as blood or tissues as if they are infectious, even if they
are thought not to be. Human samples include: human blood, blood products, and
certain body fluids (semen, vaginal, cerebrospinal, synovial, pleural, peritoneal,
pericardial, and amniotic), any body fluids in which visible blood is present, and any
Department of Physiology
Procedure No:
PHY/SOP/RE01
Revision No:
001
Title:
Effective Date :
16/6/2010
Safe handling of biological materials
(Adopted from OSHE/SOP/BS/10)
Page:
Page 8 of 9
Safety & Health
Laboratory (Location):
Cytokine biology Lab, MD9
unfixed human tissue or organ. Adopt the work practices as covered under sections
5.3.1 to 5.3.4
5.5 Safe handling of recombinant DNA
a. DNA only gains a biological function by being inserted into a living cell. Hence work with
most ‘naked’ DNA molecules is not generally thought to constitute a safety hazard.
Some degree of risk may still exist as such molecules can enter the cells of the operator
through breaks in the skin. A greater degree of risk is associated with:
i.
DNA encoding an oncogene or tumour suppressor gene product
ii.
DNA encoding growth factors, growth factor receptors or other substances that
might alter the growth patterns of human cells directly or indirectly.
iii.
Viral DNA or RNA representing complete viral genomes or fragments with the
potential to regenerate live virus.
b. Exercise good laboratory practice when handling isolated DNA molecules ('naked' DNA)
through recombinant DNA techniques such as polymerase chain reactions (PCRs), gel
electrophoresis, restriction enzymes digestion, sequencing etc. to prevent skin contact or
injection as detailed in the earlier sections.
c. Full length viral DNA/RNA are infectious in their own right and are regarded as
microorganisms even when they are not encapsulated or enveloped. This means that if
full length viral DNA were to be combined with DNA from other sources, a geneticallymodified organism would have been created. Refer to Appendix 5 of “Singapore
Biosafety guidelines for research on genetically modified organisms (GMOs)” by the
Genetic Modification Advisory Committee (GMAC) for guidance on working with viral
DNA/RNA.
d. Recombinant DNA also covers all biological entities (cells, organisms, prions, viroids or
viruses) that have been genetically modified through recombinant DNA technologies.
Evaluate the potential biohazard associated with a particular genetic modification to
select the appropriate biosafety level for such work. Refer to references 7.0f and 7.0g for
detailed guidelines for safe containment, handling and transport of genetically modified
organisms used in research.
5.6 Transport of specimens
This section is covered in detail under SOP on “Transportation & Transfer of Biological Agents”.
In summary:
a. For transport within the university: Spills or leakage should be prevented via the use
of appropriate sealed primary and secondary containers and items to be transported are
to be labeled with essential information.
b. For import or transfer within Singapore: procedures are governed by the Biological
c. Agents & Toxins Act (BATA) under the Ministry of Health for human pathogens.
Department of Physiology
Procedure No:
PHY/SOP/RE01
Revision No:
001
Title:
Effective Date :
16/6/2010
Safe handling of biological materials
(Adopted from OSHE/SOP/BS/10)
Page:
Page 9 of 9
Safety & Health
Laboratory (Location):
Cytokine biology Lab, MD9
d. For export: Export of high-risk BAs and toxins is controlled by the Strategic Goods
Control Act under the Singapore Customs.
e. For package and labeling: Biological agents to be exported must be packaged and
labeled according to International Air Transport Association (IATA) standards.
6.0 Records
Nil
7.0 References
a. Laboratory Biosafety manual 3rd edition, World Health organization (WHO).
b. OSHE Standard operating procedure (CBL/SOP/10): “Transport & Transfer of Biological
Agents”
c. OSHE Standard operating procedure (CBL/SOP/03): “Centrifuge Safety”
d. OSHE Standard operating procedure (CBL/SOP/07): “Safe handling of sharps”
e. OSHE Standard operating procedure (CBL/SOP/09): “Safe use of laboratory equipment”.
f. OSHE standard operating procedure (CBL/SOP/GS/05): “Lab Sign Posting and Labeling”
g. OSHE standard operating procedure (CBL/SOP/GS/07): “Selection of PPE”
h. CDC/ NIH booklet “Biosafety in Microbiological and Biomedical Laboratories” (5th edition,
2007, online) (http://www.cdc.gov/OD/ohs/biosfty/bmbl5/bmbl5toc.htm)
i. U.S. Department of Labor Occupational Safety and Health Administration (OSHA)
standards - 29 CFR Part 1910.1030: “Occupational Exposure to Bloodborne Pathogens
Standard” (Blood borne Pathogens Standard) (www.osha.gov )
j. Genetic Modification Advisory Committee (GMAC) guidelines: “The Singapore Biosafety
guidelines
for
research
on
Genetically
Modified
Organisms
(GMOs)”
(http://www.gmac.gov.sg )
k. NIH Guidelines: “Guidelines for Research Involving Recombinant DNA Molecules”
(http://www4.od.nih.gov/oba/rac/guidelines/guidelines.html )