Title: Blood Administration Guidelines P&P #: 2.008 Page of 7
advertisement

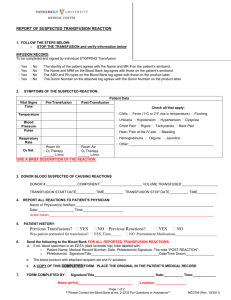
TITLE: Blood Administration Guidelines EFFECTIVE DATE: August 31, 2012 DATE REVISED: P&P #: 2.008 «DateRevised» PAGE 1 of 7 DISTRIBUTION: All Departments PURPOSE: TO POLICY: ALL NURSING STAFF WILL ADHERE TO ESTABLISHED POLICIES AND PROCEDURES RELATING TO BLOOD PRODUCTS AND THE GUIDELINES OF CARE FOR PATIENTS RECEIVING BLOOD COMPONENTS. ALL NURSES ARE REQUIRED TO BE THOROUGHLY FAMILIAR WITH INFORMED CONSENT, INITIATION OF INFUSION, MONITORING, TRANSFUSION REACTIONS, EMERGENCY RELEASE OF UNCROSSMATCHED BLOOD, OBTAINING BLOOD FROM BLOOD BANK, PATIENT REFUSAL AND RETURNING PRODUCTS TO BLOOD BANK. PROCEDURE: GUIDELINES OF CARE PROVIDE A GUIDELINE FOR THE SAFE ADMINISTRATION OF BLOOD AND BLOOD PRODUCTS. 1. Informed consent is to be obtained prior to administering blood components for non-emergency transfusions. 2. Collect all necessary supplies and have IV accessible and ready for use, prior to checking out products from Blood Bank. Only 0.9% Normal Saline may be used with blood products. 3. Transfusion must be initiated within 30 minutes of the product leaving Blood Bank. If there is a delay in starting the transfusion, the unit must be returned to the Blood Bank and stored at the proper temperature until ready for use. A unit of blood may not be transfused if it has been out a room temperature for more than 30 minutes. 4. Prior to initiation of transfusion 2 (two) licensed nurses (1 must be an RN) must verify unit and armband information against the transfusion record. A) Patient blood bank armband must identify patient first and last name, date of birth, medical record and admission number and blood bank number. B) Unit information must include: patient name, date of birth, medical record and admission number, patient’s ABO/RH, unit number, expiration date, unit ABO/RH, type of product and blood bank armband number. Specific Blood Component Administration Guidelines: TYPE OF PRODUCT SPECIAL CONSIDERATIONS INFUSION TIMELINE Packed Cells DO NOT use a blood pump if administering packed red cells unless NSS is added to the bag of packed red cells. 2-4 hours Platelets Single donor platelets will be used. Check for pre-medication order for antihistamine. Be sure to continue to agitate the platelets while they are not in use and while they are being administered to prevent their aggregation. Do not use micro aggregate filter. 30-60 min. Plasma Fresh frozen plasma cannot be re-frozen after thawing. If given for clotting factors, infuse within 24 hours of thawing. 1-4 hours Autologous PRBCs Observe for reactions like other components. 2-4 hours Directed Donor Reactions may occur as with any PRBC other blood product 2-4 hours DOCUMENTATION: Nursing will complete the Blood Administration Flow Sheet (see attached) for each unit of blood products administered. A copy must be returned to Blood Bank upon completion and original placed on the patients chart. Monitoring the Patient: Pre-Transfusion: The patient’s temperature, pulse, respiration and blood pressure must be determined and documented prior to initiating the blood transfusion so that baseline data is available in the event of a transfusion reaction. The patient will be monitored for the first 5-15 minutes of the transfusion to observe the patient for signs and symptoms of a transfusion reaction. Patient’s response during this period should be documented on the Blood Administration Flowsheet. During the transfusion: Vital signs (temperature, pulse, respiration and blood pressure) will be taken 15 minutes after initiation of transfusion, 30 minutes after initiation, then hourly until transfusion is complete. The patient should not be routinely transported off the nursing unit while blood or blood components are being administered. However, in the case of surgery, special procedures, or radiation therapy, the patient may be transported while blood is infusing with the following criteria being observed. The patient will not be transported during the first 15 minutes of the blood or blood product transfusion. Exception: A possible life-threatening situation. If this occurs a nurse will remain with the patient throughout the transport (i.e. to surgery). The nurse on the unit will call and give report to a nurse or physician in the receiving department who will assume responsibility for monitoring the transfusions when the patient is in that department unless the sending nurse remains with the patient. The nurse will accompany the patient to the receiving department. The nurse or physician from the receiving department will accompany the patient back to the unit. Patient’s response to and tolerance of the transfusion should be noted frequently. POST TRANSFUSION: Record vital signs at the end of the transfusion and observe patient closely until one hour post-transfusion. Discard blood syringe, tubing in Biohazard waste receptacle. Obtain post-transfusion Hematocrit as ordered by physician. Report results to physician. Blood Bank Transfusion Record must be completed with all required elements to include: 2 nurses signature, vital signs, transfusion reactions, transfusion start and stop times. TRANSFUSION REACTION: AT THE FIRST SIGN OF AN ADVERSE TRANSFUSION REACTION: A. STOP TRANSFUSION IMMEDIATELY! (If Urticaria (hives) or Rash only is noted, see Step #F.) B. Notify the Clinical Supervisor, Attending Physician and the blood bank at once and describe symptoms. (Described below) C. Keep IV open with slow saline drip, but use a new administration set to avoid infusing the blood remaining in the original set. D. Send the following to the Blood Bank STAT: 1. Red top tube (no gel) AND one lavender tube drawn atraumatically to avoid hemolysis. 2. Complete a Blood Transfusion Reaction Report Form Required. (Get Form from Lab) 3. Remainder of the unit with attached IV set tied off and needles removed. (Avoid contaminating the unit, as it may need to be cultured.) 4. Completed copy of the Blood Transfusion Reaction Report. 5. First voided urine marked “Post Transfusion”. E. Check for agreement of all identifying names and numbers on donor unit, transfusion record and patient armband. F. If the reaction symptoms are hives or skin rash ONLY with no other complications, a Blood Transfusion Reaction Report need not be filed. In this instance, Step D is not needed. Notification of the physician and blood bank/lab must take place for the following types of transfusion reactions: TYPE CAUSE SIGNS AND SYMPTOMS Hemolytic Antibodies in the recipient's plasma react with antigens in donor red blood cells. This leads to donor cell agglutination and capillary occlusion, blocking blood flow and oxygen to vital organs. Eventually, the red blood cells break down and release free hemoglobin into plasma and urine. This free hemoglobin may block the renal tubules, resulting in renal failure. Chills, Temperature 2 degrees above baseline, backache, restlessness, anxiety, nausea, vomiting, chest pain, tachycardia, dyspnea, hypotension, cyanosis, hemoglobinemia, hemoglobinuria, oliguria, anuria, jaundice, vascular collapse. Allergic Although its mechanism is unknown, it probably results from the reaction of allergens in donor blood with antibodies in recipient blood. Urticaria, pruritus, chills, nausea, vomiting, headache, nasal congestion, wheezing. In more severe reactions: bronchospasm, severe dyspnea, laryngeal edema, circulatory collapse. Febrile Recipient sensitivity to donor leukocytes or platelets. Temperature 2 degrees above baseline, chills, flushing, back pain, malaise, tachycardia, headache, confusion, nausea and vomiting Bacterial Circulatory Overload Air Emboli Bacterial contamination of donor blood, usually by gram-negative organisms. Temperature 2 degrees above baseline, chills, abdominal and extremity pain, vomiting, hypotension, bloody diarrhea. Rate or volume of transfusion exceeds the circulatory system's capacity. Cough, chest pain, dyspnea, distended neck veins, tachycardia, cyanosis, frothy sputum, pleural rales, and hemoptysis. Excessive air infused during transfusion, Sudden shortness of breath; sharp chest pain; anxiety; coughing; decreased blood pressure. Citrate Toxicity Hypersensitivity to product preservative Cardiac arrhythmias; nausea/vomiting; hypokalemia; alkalosis; decreased blood pressure. EMERGENCY TRANSFUSION OF UNCROSSMATCHED BLOOD: When an emergency situation arises and the physician determines that the patient’s life is in jeopardy without an emergency transfusion, uncrossmatched blood may be given. a. Nurse must fill out an Emergency Transfusion Request Form and it must be signed by the physician within 24 hours. b. Notify the Blood Bank that Emergency Release blood is needed, and who the patient is. c. Nurse must bring the patient’s sticker and obtain the number of specified emergency release O-negative uncrossmatched units of PRBC. d. Two licensed nurses shall verify blood identification labels and proceed with transfusion. e. A blood Transfusion Record form shall be completed for each unit transfused. All vitals and any reaction must be recorded. OBTAINING BLOOD PRODUCTS FROM BLOOD BANK: Blood will be signed out from the laboratory by one lab personnel and one RN. If blood is needed after hours, the House Supervisor and one other licensed nurse may sign out blood from the Blood Bank. If units are needed and not setup, lab must be notified to come in and complete the orders. 1. IV line must be in place and ready for use prior to picking up units from the Blood Bank. 2. Bring the patient’s sticker from the chart to the Blood Bank. 3. Verify name, visit number, patient’s ABO/RH, unit number, expiration date, unit ABO/RH, type of product and BB armband number. Verify any other pertinent information such as positive antibody screens and that the unit is negative for that patient’s antibodies. a. Information is to be read by Lab and verbal verification read back by RN. Any discrepancy found needs to be corrected prior to disposition of blood. 4. Sign out units in Blood Bank log book. Issued by, issued to and date/time. 5. Blood must be transported to the floor in a biohazard bag and the transfusion started within 30 minutes of checking out the unit. Only one unit of PRBC is to be released at once, except in the case of an emergency. REFUSAL OF BLOOD PRODUCTS: It is the policy of HERITAGE PARK SURGICAL HOSPITAL to verify, by means of the “Refusal To Permit Blood Transfusion” form, that the patient’s informed refusal has been obtained by the treating physician after the patient has been informed of the possible risks and complications that may occur as a result of the patient’s refusal to receive recommended transfusion of blood products or components of blood. 1. It is the exclusive duty and responsibility of the treating physician to provide information and to obtain informed consent. 2. In the event that the patient refuses to give consent for the proposed blood transfusion, the physician has a duty to give the patient all the information that is relevant to a meaningful decision sufficient for the patient to understand the potential consequences of declining a blood transfusion. 3. A valid consent can only be obtained under circumstances, which are free of any suggestion of duress or coercion. 4. It is the responsibility of the treating physician to document in the medical record the initial refusal and the outcome (i.e., consent or continued refusal). The documentation should specify that the physician gave the patient the relevant information, including that pertaining to the potential consequences of declining a blood transfusion. 5. The Clinical Supervisor should be notified of the patient’s informed refusal. 6. A notification form providing information on the patient’s informed refusal should be completed and forwarded as appropriate. End of Policy and Procedure B LO OD ADM INIST RAT IO N GU ID EL IN ES BLOOD COMPONENTS TYPE OF TUBING VITAL SIGNS USUAL LENGTH INFUSION NURSING IMPLICATIONS WHOLE BLOOD Y-type blood administration set. Microaggregate Filter if administering to a cardiothoracic surgery patient Prior to administration; 5 minute observation; 15 minutes; 30 minutes; every one hour during and upon completion. 3-4 hours (maximum four (4) hours.) Watch for s/s transfusion reaction. Change filter every two units. PACKED RED BLOOD CELLS Y-type blood administration set Prior to administration; 5 minute observation; 15 minutes; 30 minutes; every one hour during and upon completion. 2-3 hours (maximum four (4) hours.) Watch for s/s transfusion reaction. FRESH FROZEN PLASMA Blood component recipient set or can be given through a Y-type blood administration set Prior to administration; 5 minute observation; 15 minutes; 30 minutes; every one hour during and upon completion. Depends on patient's condition. Usually less than one (1) hour (maximum 4 hrs) Watch for s/s of fluid overload. ABO group specific or compatible Rh type is generally not required since not RBC's. PLATELETS Blood Component Recipient set Prior to administration; 5 minute observation; 15 minutes; 30 minutes; every one hour during and upon completion. Less than one hour ALBUMIN Tubing supplied with product Pre and post infusion baseline and hourly assessment until transfusion is completed. Depends on Patients Condition. Usually 1mL/min for 25% Albumin Comes from Pharmacy. Watch for s/s of fluid overload. Only one person must identify product and patient. CRYOPRECIPITATE Blood component recipient set Per blood administration flowsheet As quickly as possible or as ordered Only someone experienced in venipuncture should attempt IV on this patient. FACTOR VIII Prefilled syringe or IV tubing Can be taken PRN As quickly as possible or as ordered It should be hung promptly to ensure stability and can be used for 24 hour infusions. DO NOT REFRIGERATE. FACTOR IX Prefilled syringe or IV tubing Can be taken PRN As quickly as possible or as ordered MUST BE INFUSED WITHIN 1-3 HOURS FEIBA Prefilled syringe or IV tubing Can be taken PRN As quickly as possible or as ordered MUST BE INFUSED WITHIN 1-4 HOURS. DO NOT REFRIGERATE AFTER RECONSTITUTION. IBG Prefilled syringe or IV tubing or IM Can be taken PRN or as ordered Initial dose of 0.5- 1 mg x 30 min. subsequent doses at 125u/hr. Should be infused at room temperature. Stability is maintained for 8 hours at room temperature or 24 hours refrigerated. DO NOT SHAKE. DO NOT MIX WITH OTHER IV INFUSIONS. ****Only 0.9% Normal Saline may be used with any/all blood products.