30wkMgmtGuidelines1
advertisement
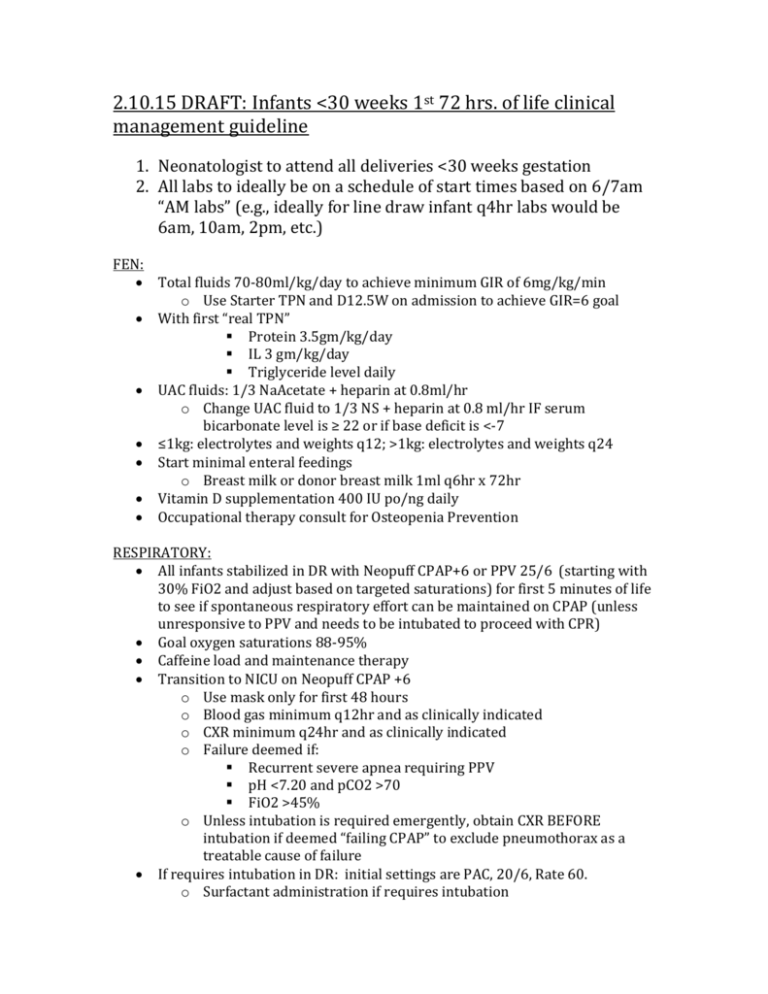
2.10.15 DRAFT: Infants <30 weeks 1st 72 hrs. of life clinical management guideline 1. Neonatologist to attend all deliveries <30 weeks gestation 2. All labs to ideally be on a schedule of start times based on 6/7am “AM labs” (e.g., ideally for line draw infant q4hr labs would be 6am, 10am, 2pm, etc.) FEN: Total fluids 70-80ml/kg/day to achieve minimum GIR of 6mg/kg/min o Use Starter TPN and D12.5W on admission to achieve GIR=6 goal With first “real TPN” Protein 3.5gm/kg/day IL 3 gm/kg/day Triglyceride level daily UAC fluids: 1/3 NaAcetate + heparin at 0.8ml/hr o Change UAC fluid to 1/3 NS + heparin at 0.8 ml/hr IF serum bicarbonate level is ≥ 22 or if base deficit is <-7 ≤1kg: electrolytes and weights q12; >1kg: electrolytes and weights q24 Start minimal enteral feedings o Breast milk or donor breast milk 1ml q6hr x 72hr Vitamin D supplementation 400 IU po/ng daily Occupational therapy consult for Osteopenia Prevention RESPIRATORY: All infants stabilized in DR with Neopuff CPAP+6 or PPV 25/6 (starting with 30% FiO2 and adjust based on targeted saturations) for first 5 minutes of life to see if spontaneous respiratory effort can be maintained on CPAP (unless unresponsive to PPV and needs to be intubated to proceed with CPR) Goal oxygen saturations 88-95% Caffeine load and maintenance therapy Transition to NICU on Neopuff CPAP +6 o Use mask only for first 48 hours o Blood gas minimum q12hr and as clinically indicated o CXR minimum q24hr and as clinically indicated o Failure deemed if: Recurrent severe apnea requiring PPV pH <7.20 and pCO2 >70 FiO2 >45% o Unless intubation is required emergently, obtain CXR BEFORE intubation if deemed “failing CPAP” to exclude pneumothorax as a treatable cause of failure If requires intubation in DR: initial settings are PAC, 20/6, Rate 60. o Surfactant administration if requires intubation o Adjustments made in DR vent settings based on blood gases and chest rise/oxygen saturations o Blood gas obtained in DR once central access obtained Goal ABG/VBG: pH 7.25-7.35, pCO2 45-60 o Once in NICU, will only use PAC as mode of ventilation on Avea Initial settings PAC 20/6, Rate 60 unless already adjusted based on blood gas from delivery room If spontaneously breathing above set rate and blood gas shows over-ventilation, decrease vent set (apnea) rate to 40 and decrease PIP to achieve ideal blood gas values Goal ABG/VBG: pH 7.25-7.35, pCO2 45-60 If not spontaneously breathing above set ventilator rate and blood gas shows over-ventilation, decrease vent rate incrementally down to minimum of 40 and then work to decrease PIP to achieve ideal blood gas values Failure of conventional ventilation with need to move to high frequency ventilation deemed if: Blood gases suboptimal with Rate= 60 and/or PIP>28 Oxygen needs >60% for >30 minutes o Blood gases minimum q4hr and as clinically indicated o CXR minimum q24hr and as clinically indicated If requires high frequency ventilation o Blood gases minimum q4hr and as clinically indicated o CXR minimum q12hr to assess MAP lung expansion and as clinically indicated EXTUBATION GUIDELINES: Consider extubation by 18 hours of life Extubation criteria: FiO2 <0.3 Spontaneously breathing above set ventilator rate PIP ≤ 20 PEEP ≤ 6 Caffeine being given pH >7.25 pCO2 <60 REDOSING SURFACTANT GUIDELINE: FiO2 >0.3 PIP >22 NONINVASIVE RESPIRATORY SUPPORT GUIDELINE: For CPAP support use either CPAP of 6 or SiPAP 10/6 o Leave on CPAP until FiO2 21% for minimum of 24 consecutive hours or 32 weeks CGA o If met criteria for FiO2 21% on CPAP, first attempt to wean off CPAP completely to room air. If unsuccessful and baby currently <32 weeks gestation, place back on CPAP and continue to try to wean completely off CPAP to room air as clinically indicated. o After a baby is 32 weeks CGA, if still requires non-invasive support and cannot wean to room air, may consider use of HFNC or LFNC. CARDIOVASCULAR: Double lumen UVC in all infants o Have a fluid always running through the second port – do not “heplock” as this increases risk of line becoming dysfunctional UAC to be placed in all infants born at <27 weeks or if infant requires intubation Hypotension deemed by 2 out of 3 parameters: o Prolonged capillary refill o Low urine output o Low blood pressure (i.e. Mean BP < gestational age in weeks) Treatment of hypotension o NS flush 10ml/kg or colloid 10ml/kg once o If no improvement, discuss with Neonatologist or fellow re: use of second fluid bolus vs. starting pressor support o If hypotension or on pressors, follow iCa q12hr and treat to keep normal INFECTIOUS DISEASE: Unless in room air with no risk factors for infection, all infants will have admission blood culture and IV Ampicillin and Gentamicin initiated NEUROLOGIC: Indomethacin prophylaxis on all infants <1kg (of note, non-nutritive feedings and Vitamin D acceptable when receiving indomethacin) Head ultrasound at 5-7 days of age Midline head positioning ordered per protocol HEMATOLOGY: Coags only obtained if active bleeding Infant blood type & DAT testing on admission Hemoglobin and platelet count daily o Treat per clinical transfusion guidelines GI: First bilirubin level to be obtained at 12-24 hours of life. o Checked daily o Increase in total daily fluid goal by 20ml/kg/day if initiating overhead phototherapy RENAL: If urine output <1ml/kg/day over previous 12 hours o Consider use of bladder scanner to evaluate for urine and possible need for Foley catheter o Give NS 10ml/kg bolus o If no improvement in urine output over next 4 hours, give Lasix 1mg/kg IV o If no improvement in urine output over next 4 hours, consider more volume versus low-dose Dopamine Confidential 2/9/2016