Appendix Methods Survey Tool and Process We used a Web
advertisement
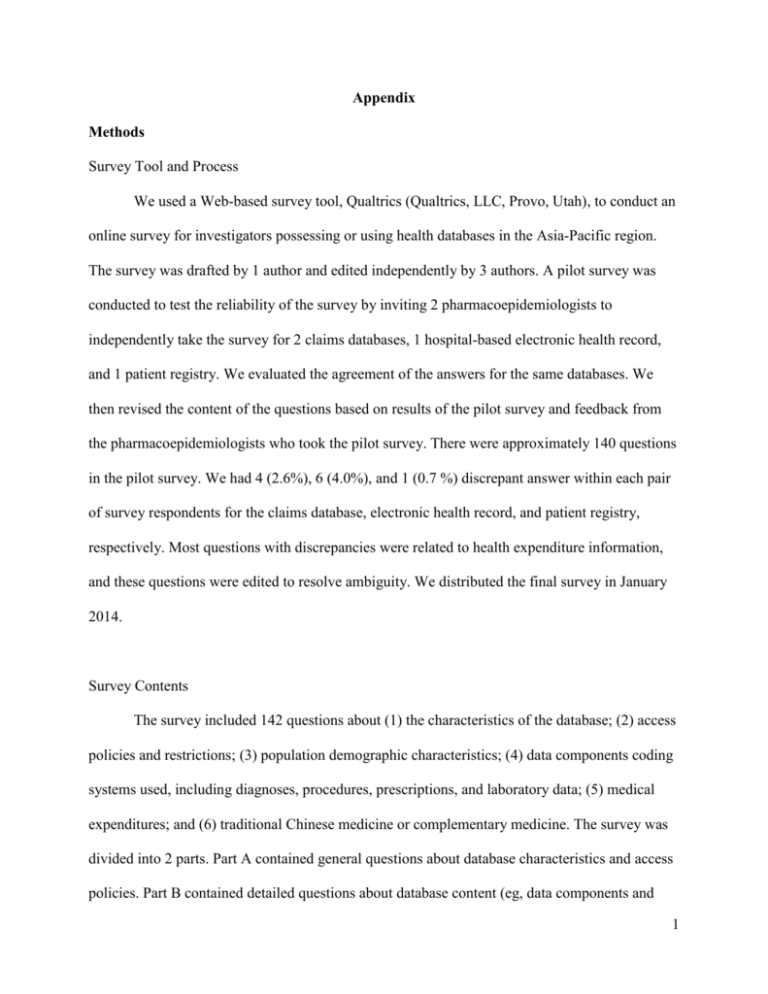
Appendix Methods Survey Tool and Process We used a Web-based survey tool, Qualtrics (Qualtrics, LLC, Provo, Utah), to conduct an online survey for investigators possessing or using health databases in the Asia-Pacific region. The survey was drafted by 1 author and edited independently by 3 authors. A pilot survey was conducted to test the reliability of the survey by inviting 2 pharmacoepidemiologists to independently take the survey for 2 claims databases, 1 hospital-based electronic health record, and 1 patient registry. We evaluated the agreement of the answers for the same databases. We then revised the content of the questions based on results of the pilot survey and feedback from the pharmacoepidemiologists who took the pilot survey. There were approximately 140 questions in the pilot survey. We had 4 (2.6%), 6 (4.0%), and 1 (0.7 %) discrepant answer within each pair of survey respondents for the claims database, electronic health record, and patient registry, respectively. Most questions with discrepancies were related to health expenditure information, and these questions were edited to resolve ambiguity. We distributed the final survey in January 2014. Survey Contents The survey included 142 questions about (1) the characteristics of the database; (2) access policies and restrictions; (3) population demographic characteristics; (4) data components coding systems used, including diagnoses, procedures, prescriptions, and laboratory data; (5) medical expenditures; and (6) traditional Chinese medicine or complementary medicine. The survey was divided into 2 parts. Part A contained general questions about database characteristics and access policies. Part B contained detailed questions about database content (eg, data components and 1 coding). To avoid ambiguity, we constructed most questions to have a “yes” or “no” response. The survey was designed to take approximately 30 minutes to complete. Targeted Health Databases and Survey Participants Targeted databases were identified through the AsPEN website and recommendations provided by AsPEN members.9 Identified databases included claims databases, hospital-based electronic health records, and patient registries. The coordinating center distributed the final survey to the pharmacoepidemiologist or relevant researchers for each identified database. A reminder letter was sent to nonresponders 1 month after the date of survey distribution. A followup letter was sent to participants to ensure the information was correct, complete, and up-to-date at the time of study completion. 2 Description of Participating Databases Among the 11 databases, 4 were nationwide claims databases from Japan (Japan Medical Data Center Database [JMDC] and the National Database [NDB]), South Korea (Health Insurance Review and Assessment Service [HIRA]), and Taiwan (National Health Insurance Research Database [NHIRD]); and 2 were nationwide hospital-based electronic health records from Hong Kong (Clinical Data Analysis and Reporting System [CDARS]) and Singapore (National Electronic Health Record [NEHR]). The 4 nationwide claims databases covered approximately 23 million to 128 million individuals, and the 2 electronic health record databases covered approximately 7 million and 5 million individuals, respectively, representing all age groups and mostly Asian ethnicities. An additional hospital-based electronic health record for approximately 5 million individuals was from the West China Hospital (Hospital Information System of West China Hospital [HIS-WCH]); and 2 electronic health record databases were from Thailand and covered approximately 350,000 individuals from Buddhachinaraj Hospital (Buddhachinaraj Hospital database [BHD]) and 1 million from 21 hospitals in the Ubon Ratchathani region (Hospital Information [HI]). We also included 2 registries of patients with cancer and stroke from Taiwan. Detailed descriptions of participating databases are presented below. Clinical Data Analysis and Reporting System (Hong Kong) The Hong Kong Hospital Authority is a statutory body that manages all public hospitals and their outpatient clinics in Hong Kong. The Hospital Authority not only provides acute hospital care, but also provides acute and chronic disease management to patients in the community via outpatient clinics (both specialists and general physicians) throughout Hong Kong. Health services are available to all Hong Kong residents (over 7 million people). 3 Data were extracted from the Clinical Data Analysis and Reporting System (CDARS), a database developed by the Hospital Authority. In 1995, the Hospital Authority developed the Clinical Management System (CMS), an electronic health record system that allows clinicians to order, document, and review care in their daily practice. CMS contains patients’ data, including demographic information, diagnosis, payment method, prescription information, laboratory tests, and hospital admission and discharge information. Drug information is stored in the system with prescribing details (eg, drug name, dose, drug frequency). Data from CMS are transferred to CDARS for research and audit purposes. CDARS also contains a multitude of data warehouses, including the Accident and Emergency Information System, Medical Record Abstract System, InPatient Administration System, and the Pharmacy Management System/Corporate Drug Dispensing History. Patient records in CDARS are anonymous (patient names, Hong Kong identification card numbers, addresses, and telephone numbers are not available) to protect patient confidentiality. A unique patient reference number is generated for each individual case to facilitate data retrieval and further analysis. CDARS has captured data since 1995. National Health Insurance Research Database (Taiwan) Taiwan’s National Health Insurance Research Database (NHIRD) is maintained by the National Health Research Institutes (NHRI) and is made accessible for research purposes. Taiwan launched a single-payer and mandatory national health insurance program on March 1, 1995, and by 2007, nearly 99% of the population was enrolled. The NHRI compiles information including the demographic characteristics of enrollees, health care professionals, and facilities and service claims from inpatient, ambulatory care, and contracted pharmacies for reimbursement purposes. Personal identifiers are encrypted for privacy protection, but all data sets can be linked to each other with the unique and anonymous identifiers created by the NHRI. 4 Taiwan Stroke Registry The Taiwan Stroke Registry is a government-funded project that identifies patients with acute stroke hospitalized within 10 days of symptom onset. (Definitions of acute stroke and its subtypes and registration criteria are available online at http://circ.ahajournals.org/content/122/11/1116/suppl/DC1). Formally launched on August 1, 2006, it engages 56 academic and community hospitals serving approximately 18% of stroke hospitalizations in the entire country, with 4 steps of quality control to ensure the reliability of entered data. All data were compiled prospectively by registry-trained neurologists and study nurses, and all enrolled patients were visited by physiatrists, who started rehabilitation within 72 hours after admission. More than 110 000 patients with stroke were registered when the present study was undertaken. Approval of the registry as a human study protocol was obtained from the institutional review board of each participating hospital, with stroke patients providing informed consent for follow-up. The data collection and quality-assurance processes and preliminary results of the population in the registry have been detailed elsewhere (Hsieh FI, Lien LM, Chen ST, Bai CH, Sun MC, Tseng HP, et al; Taiwan Stroke Registry Investigators. Get With the Guidelines-Stroke performance indicators: surveillance of stroke care in the Taiwan Stroke Registry: Get With the Guidelines-Stroke in Taiwan. Circulation. 2010;122:1116–1123.). In brief, preadmission medical and medication histories, stroke risk factors, clinical, laboratory and neuroradiological findings, interventions, and hospital course, including deterioration and outcome measures, were recorded in the registry. Stroke subtypes and locations were documented based on computed tomography and/or MRI findings. Ischemic stroke were further classified according to the Trial of ORG 5 10172 in Acute Stroke Treatment (TOAST) criteria: large-artery atherosclerosis, small-vessel occlusion, cardioembolism, specific causes, and undetermined causes. The National Institutes of Health Stroke Scale (NIHSS) score was recorded in all patients on admission and on discharge. Investigators who rated the NIHSS were certified by the Taiwan Stroke Society and trained for data entry through a Web-based TSR database system. In addition, the Barthel index score and modified Rankin Scale (mRS) were recorded at 1, 3, and 6 months after the stroke at the outpatient clinic or through structured telephonic interview. Taiwan Cancer Registry The Taiwan Cancer Registry started in 1996 and became nationwide in June 2003. According to the Cancer Prevention Act, enacted in 2002, hospitals with a capacity of more than 50 beds that provide outpatient and hospitalized cancer care are recruited to participate in reporting newly diagnosed malignant neoplasms to the registry. The registry has included cervical cancer patients since 2002, extending to breast cancer, oral cavity cancer, lung cancer, hepatocellular carcinoma and colon/rectal cancer patients in 2007. In 2008, the registry further expanded to include patients with prostate cancer, gastric cancer, esophageal cancer and bladder cancer. The registry has also recruited patients with nasopharynx cancer, salivary gland tumors, uterine sarcoma, ovarian cancer and hematopoietic and lymphoid neoplasms since 2009. The registry includes demographic information, primary cancer diagnoses, first cancer diagnosis data, histology, tumor stages, surgery, radiation therapy, and chemotherapy records. Recurrence and survival status are also available in the registry. 6 National Database of Japan The Japanese universal multipayer health care system was established in 1961, but Japan’s National Database of health insurance claims was created only recently. In April 2009, 85.8% of claims from hospitals, 40.7% of claims from clinics, and 98.6% of claims from community pharmacies were issued in electronic format. The database includes data from all claims issued in Japan in electronic format since April 2009. In August 2010, 89.5% of claims issued from clinics were in electronic format. In May 2011, 99.6% of claims from hospitals, 91.3% of claims from clinics, and 99.9% of claims from community pharmacies were issued in electronic format and incorporated into the database. Since 2011, the database has been available for secondary purposes, including scientific research, on a trial basis. As such, the number of researchers and other users of the database for secondary purposes is still limited as of May 2014. Claims data include diagnoses (given as domestic codes which can be linked to ICD-10 in a master table), prescription and dispensing of drugs, and medical procedures, including laboratory tests. The information on year and month of outpatient visits and date of admission and duration of hospital stay is also available. The information of year and month of death is also available provided that the death occurred in the health care under the health insurance system. Japan Medical Data Center Database Japan has a universal health care system, and all citizens are insured by one of thousands of insurers offering different types of coverage, such as health insurance for employees and their dependents. With a few exceptions, the cost is fixed by the government for individual drugs, laboratory tests, and medical procedures. The Japan Medical Data Center has obtained from corporate health insurance companies (1) claims data, (2) demographic and enrollment/disenrollment data, and (3) health screening data for a total of 4 million people (about 7 3% of the population) dating back to January 2005. People of working age and children are overrepresented, and elderly people are underrepresented. Claims data include outpatient visits, admission, diagnoses, prescription/dispensing of drugs, laboratory tests, and medical procedures. Health screening data, available for about one-fourth of the insured, includes body mass index, blood pressure, fasting blood glucose, HbA1c, cholesterol levels, and triglyceride levels. All patients are anonymized, and a unique patient number created by the Japan Medical Data Center is given for data analysis. Health Insurance Review and Assessment Service (Korea) In 1989, the South Korean government enacted universal health care insurance coverage, which currently covers 97% of the total population. The Health Insurance Review and Assessment Service evaluates the suitability of each expense and the National Health Insurance Service pays the provider by fee-for-service reimbursement. Accordingly, the database contains all medical information for approximately 50 million Koreans. The database includes each patient’s unique encrypted, age, sex, primary or secondary diagnosis (ICD-10 code), surgical or medical treatment administered, whether the individual was an inpatient or outpatient, type of insurance (National Health Insurance or Medical Aid), medical expenses, medical institution identification number, and prescriptions. National Electronic Health Record (Singapore) The Singaporean Ministry of Health created a national electronic health record system for the public health sector in 2011. The system is available to all public health care institutions (8 restructured hospitals, 8 specialist centers, and 18 polyclinics), 5 community hospitals, 2 nursing homes, a hospice, selected general practitioners, and users from the Agency for Integrated Care. 8 The system aims to help clinicians improve the quality of health care for more than 5 million Singapore residents by providing them with more timely, harmonized, and accurate patient health information from a central repository of aggregated data from source systems. The captured information includes medication histories, allergies, laboratory results, radiology results, and hospital inpatient discharge summaries. Buddhachinaraj Hospital Database (Thailand) The Buddhachinaraj Hospital database is a regional hospital database maintained and regularly updated by the Buddhachinaraj Hospital, a regional hospital in northern Thailand. The database from 2008 through 2012 contained data for about 350 000 outpatients with 2 388 000 visits and 165 000 inpatients with 258 000 admissions. The database includes inpatient, outpatient, pharmacy, and charge sub-databases. The inpatient and outpatient sub-databases contains information on age, sex, health insurance, date of birth, and diagnosis codes (ICD-10). The pharmacy sub-database contains drug name, regimen, and amount of medication per prescription. In addition, the charges sub-database contains drug, laboratory, medical service, and other service charges. Individual identifiers are encrypted for privacy protection, but all data sets can be linked to each other with the unique identifiers. Hospital Information Database (Thailand) The Hospital Information database was initiated by the medical director at Warinchamrab Hospital in the Ubon Ratchathani province of Thailand. It is widely used in community hospitals in Ubon Ratchathani, except 4 hospitals using other database systems. The database covers patients with different health care schemes and contains health care information used in providing medical care, such as medical diagnosis using ICD-10 codes, signs and symptoms, prescription 9 data using an individual coding system for routine practice and a national coding system for data pooling, the amount of drug supply and administration dose, and laboratory tests. Patient identifiers are encrypted for research and policy purposes. The database has been shown to have a high level of validity. 10