Billing, Coding & Insurance Study Guide
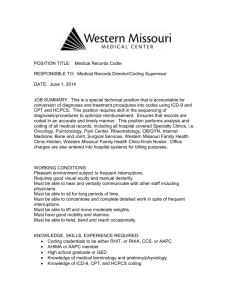
advertisement

Billing, Coding and Insurance (Content Area II: Administrative Knowledge) 1. Coding systems are: a. used to place verbal descriptions of medical conditions or procedures into alpha-numeric codes. b. a method of monitoring disease processes. c . used to allow for easier statistical tracking of medical conditions or procedural uses. d. All of the above. Explanation: Coding systems are a way for medical conditions and procedures to be listed as a number. This allows for easier tracking of statistics related to this information. It also allows for easier communication between physicians and health care insurance plans. 2. ICD-9 coding books: a. are organized into three volumes. b. used to code diagnostic procedures. c. are revised bi-annually. d. None of the above. Explanation: ICD-9 coding manuals are organized into three separate sections, each with its own function. These codes are used to code medical conditions that are treated by a health care provider. The newest version, ICD-10, is in the early implementation phase in the United States. 3. Volume II of the ICD-9 coding book: check a. is the three part alphabetical index. b. Contains procedural codes for specific diagnostic tests. c. contains three sections with Section 3 being the Index to Diseases. d. None of the above. Explanation: Volume II of the ICD-9 coding book is the three part alphabetical index, which should be used first when searching for the correct diagnostic code to be used for a disease state. Volume I is then used to confirm that the code chosen is correct. 4. The CPT Coding Book: a. provides a 5 digit code for all procedures or services that may be performed on a patient. b. provides numeric codes that allows for easier communication with insurance providers. check c. is divided into six sections. d. All of the above. Explanation: The CPT coding book is used to code procedures and diagnostic testing. The manual is divided into six sections and contains 5 digit codes for medical procedures. 5. The following symbol (*): a. is used in the ICD-9 book to designate additional diagnoses. b. is found in the CPT book to designate revised guidelines for code use. check c. designates variable pre and postoperative services. d. None of the above. Explanation: Symbols used in the CPT coding manual are used to add additional information to procedural codes. The asterisk is used to note that services used with a particular code vary between pre- and postoperative services. 6. The modifier that notes, "Bilateral Procedure," is: a. 26 check b. 50 c. 53 d. 24 Explanation: Modifiers are used with CPT codes to add additional information to a procedural code. A common modifier is -50 which denotes that a procedure that was performed was done on both right and left sides, or bilaterally. 1 7. In the CPT manual, codes in the range of 99201-99600 are: a. Surgical Codes check b. Evaluation and Management Codes c. Radiology Codes d. All of the above. Explanation: E&M codes are CPT codes that are used when a patient is being evaluated and treated. These codes are assigned based on the type of appointment that is done. For example, a patient who is new to the practice would receive an E&M code that designates a new office visit that allows time for a thorough history and examination. 8. When coding using HCPCS, a code that is accompanied by a diamond symbol would indicate: a. Special instructions are provided that describe how this code should be used to be included for reimbursement. check b. This code is not covered or valid with Medicare. c. There is the potential for this code not to be covered by the insurance carrier. d. The code is new. Explanation: Codes that are accompanied by a diamond symbol indicate that the code is not recognized by Medicare and will not be reimbursed. 9. E&M codes: check a. define a new patient as being one that is new to the practice or who hasn't been seen by that practice in at least three years. b. are defined as Evaluation and Medication codes. c. are selected based on criteria set forth by the American Medical Association. d. None of the above. Explanation: New patients are patients that have not been to the practice for at least three years, or a patient that has not previously been seen at the practice. Specific E&M codes exist to properly code the primary office visit to reflect the new patient standing. 10. The first place to look for an ICD-9 code should be: a. in Volume III check b. in Volume II and then confirmed in Volume I. c. in Volume IV with confirmation made in Volume III. d. None of the above. Explanation: When coding for diagnosis, codes should first be found in Volume II, which is the alphabetic listing. When this code is found, it is then confirmed by finding it in Volume I. 11. There are two coding tables in Volume II of the ICD-9 book. What are they? check a. Hypertension and Neoplasm b. Radiology and Laboratory Codes c. Cancer and Accidents d. None of the above. Explanation: Coding tables are added to Volume II for disease states that have a number of different variables. Hypertension and Neoplasms can come in a variety of forms, so to assist the coder in locating the correct code for these conditions, tables were added for ease in finding the appropriate code. 12. A clause in an insurance policy that restricts overpayment of benefits due to more than one medical insurance policy is: a. not legal. check b. known as coordination of benefits. c. used frequently by patients with only one policy. d. None of the above. Explanation: Patients who have a primary and secondary insurance plan fall under the coordination of benefits clause. This wording discourages multiple payments for the same procedure. 2 13. An HMO is: a. a group model of managed care. b. a health model that emphasized preventative care. c. can be part of a group or a single organization. check d. All of the above. Explanation: HMOs are Health Maintenance Organizations. This type of managed care system is set up to emphasize well care to reduce the number of illnesses a patient suffers, which will lower the overall cost of the plan as a whole. 14. To qualify for Medicare, a person must meet which of the following criteria? check a. must be 65 or older unless disabled. b. must have contributed to FICA in the past. c. must have received Social Security Disability for more than 1 year. d. All of the above. Explanation: To qualify for Medicare, a patient must fall into one of several groups which could include, being age 65 or older, being a spouse of an employee currently contributing to FICA, or being person who has been receiving Social Security disability for more than two years. 15. A patient receives Medicaid, but is also covered under Tricare. Which plan would serve as primary payer? a. Medicaid check b. Tricare c. CHAMPVA d. None of the above. Explanation: When a patient is covered by Tricare and another health insurance policy, Tricare is the secondary payer. However, when the second policy is Medicaid, Tricare is the primary payer. 16. Workman's Compensation claims: a. are federally managed. check b. are kept separate from other insurance claims which are not Workman's Comp in nature. c. are to be shared with the patient's employer with full medical record review. d. None of the above. Explanation: Workman's Compensation files are to be kept separate from a patient's usual medical record. These forms are filed to the state for claims for payment. 17. Medicare Part A: check a. covers inpatient care. b. covers outpatient care. c. is voluntary and pays 80% by Medicare and 20% by the patient. d. Allows participants to choose managed care plans. Explanation: Medicare Part A covers inpatient hospital stays. Part B covers outpatient coverage. Part C, also known as Medicare Advantage, is another Medicare plan that covers Part A and B. Part D covers pharmaceuticals. 18. When reading the CPT manual, a triangle next to a code notes: a. a new procedure check b. revised code description c. add-on codes d. codes that are not to be used with modifier -51. Explanation: Symbols added to CPT codes give the codes additional information. A triangle will denote that a code has been recently revised. 3 19. When considering coding for hospital stays, a _____________ is used to provide physicians with guidelines for admission and length of hospital stays. check a. Diagnosis Related Group (DRG) b. Health Care Financing Administration Common Procedural Coding System (HCPCS) c. Relative Value Study (RVS) d. E and V Codes Explanation: Diagnosis Related Groups are used for inpatient hospital stays. These codes help physicians decide the length of stay for a patient with a particular type of illness or condition. Most medical assistants will not directly deal with DRGs as MAs are not usually found in hospital settings. 20. Where would your office obtain additional legal copies of Medicare forms? check a. From an agency listed in the Medicare fiscal agencies directory. b. Internal Revenue Service c. Centers for Disease Control d. A local CHAMPUS office Explanation: Medicare forms can be found by searching the internet for a Medicare fiscal agency in your geographic location. The IRS, CDC and CHAMPUS offices would not have this type of information. 21. A deductible: a. is paid by the insurance company in full. b. is deducted from the payment owed the physician. check c. is paid by the patient before insurance coverage pays for medical costs. d. is money owed the insurance company. Explanation: Deductibles are set amounts of fees that will be the responsibility of the patient and are not covered by insurance. These fees usually have a limit and once that limit is reached, the insurance will then cover the difference. 4