Value Based Purchasing & Readmission Program
advertisement
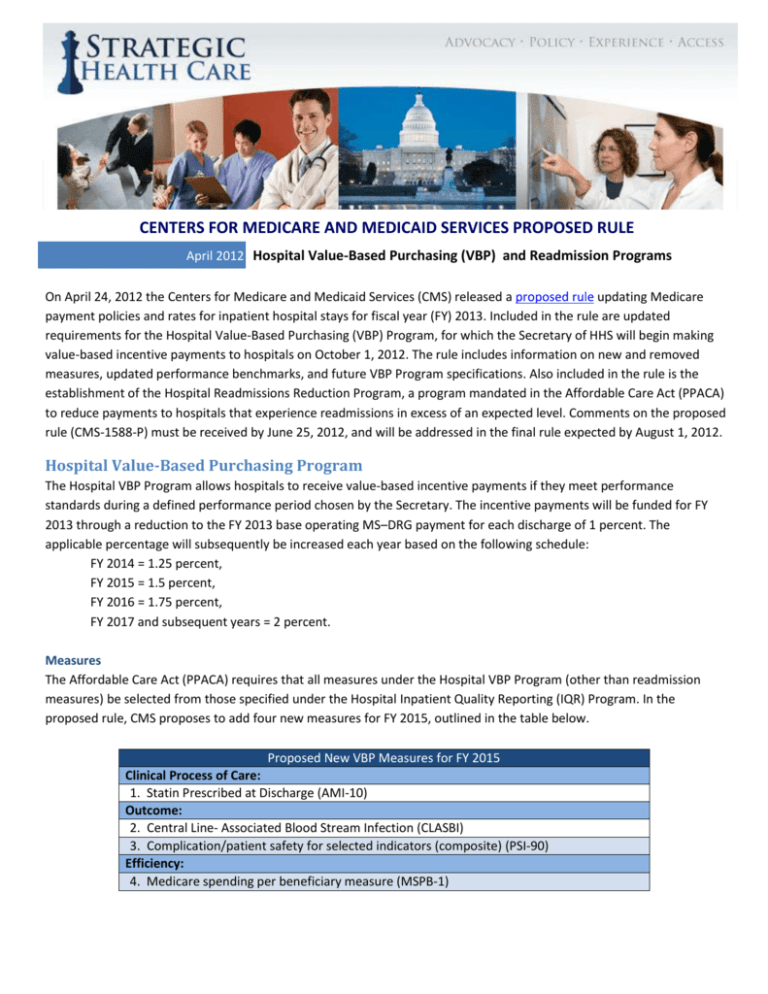
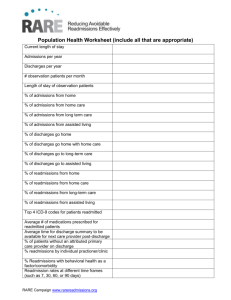
CENTERS FOR MEDICARE AND MEDICAID SERVICES PROPOSED RULE April 2012 Hospital Value-Based Purchasing (VBP) and Readmission Programs On April 24, 2012 the Centers for Medicare and Medicaid Services (CMS) released a proposed rule updating Medicare payment policies and rates for inpatient hospital stays for fiscal year (FY) 2013. Included in the rule are updated requirements for the Hospital Value-Based Purchasing (VBP) Program, for which the Secretary of HHS will begin making value-based incentive payments to hospitals on October 1, 2012. The rule includes information on new and removed measures, updated performance benchmarks, and future VBP Program specifications. Also included in the rule is the establishment of the Hospital Readmissions Reduction Program, a program mandated in the Affordable Care Act (PPACA) to reduce payments to hospitals that experience readmissions in excess of an expected level. Comments on the proposed rule (CMS-1588-P) must be received by June 25, 2012, and will be addressed in the final rule expected by August 1, 2012. Hospital Value-Based Purchasing Program The Hospital VBP Program allows hospitals to receive value-based incentive payments if they meet performance standards during a defined performance period chosen by the Secretary. The incentive payments will be funded for FY 2013 through a reduction to the FY 2013 base operating MS–DRG payment for each discharge of 1 percent. The applicable percentage will subsequently be increased each year based on the following schedule: FY 2014 = 1.25 percent, FY 2015 = 1.5 percent, FY 2016 = 1.75 percent, FY 2017 and subsequent years = 2 percent. Measures The Affordable Care Act (PPACA) requires that all measures under the Hospital VBP Program (other than readmission measures) be selected from those specified under the Hospital Inpatient Quality Reporting (IQR) Program. In the proposed rule, CMS proposes to add four new measures for FY 2015, outlined in the table below. Proposed New VBP Measures for FY 2015 Clinical Process of Care: 1. Statin Prescribed at Discharge (AMI-10) Outcome: 2. Central Line- Associated Blood Stream Infection (CLASBI) 3. Complication/patient safety for selected indicators (composite) (PSI-90) Efficiency: 4. Medicare spending per beneficiary measure (MSPB-1) Also in FY 2015, CMS proposes to remove the previously endorsed SCIP-VTE-1 measure from both the VBP Program and the Hospital IQR Program, citing its similarity to another measure (SCIP-VTE-2), and the fact that it is no longer endorsed by the NQF. The “Medicare spending per-beneficiary measure” will include Part A and Part B payments from 3 days prior to an admission through 30 days post discharge with certain exclusions. The measure will also be risk-adjusted for age and severity of illness, and will be standardized to remove differences in geographic payment adjustments and other payment factors. CMS anticipates submitting the proposed measure to the NQF for endorsement in the near future. The performance period for the FY 2015 Hospital VBP Program will begin May 1, 2013, which CMS notes is more than one year after the performance data has been publicly posted. The “Statin Prescribed at Discharge" measure was included as part of the Hospital IQR Program in FY 2013. CMS notes that data concerning the measure were posted on the Hospital Compare Web site on January 26, 2012, and is thus proposing a 9-month performance period for this measure for FY 2015. The measure is NQF-endorsed (#0639) and has also received strong support of the American College of Cardiology (ACC)/American Heart Association (AHA). CMS states in the proposed rule that the "PSI-90" and the "CLABSI” measures are consistent “with the intention captured in the Hospital VBP Program’s statutory requirement that we consider measures of HAIs for the FY 2013 Hospital VBP Program’s measure set.” Fiscal Year 2016 CMS also proposes reclassifying the VBP measures into six new domains in FY 2016: (1) Clinical Care, (2) Person- and Caregiver-Centered Experience and Outcomes, (3) Safety, (4) Efficiency and Cost Reduction, (5) Care Coordination, and (6) Community/Population Health. CMS solicits comments on changes to the domains as well as on how to properly weight the domains in FY 2016. Specifically, the agency requests comment on whether it should continue to group all outcome measures in a single domain, and on the implications of and alternatives to the proposed approach of including both clinical process of care measures and outcome measures in one Clinical Care domain. Other Proposals Definition of “Base Operating DRG Payment Amount” CMS proposes to define the term “base operating DRG payment amount” for purposes of the Hospital VBP Program as “the wage-adjusted DRG operating payment plus any applicable new technology add-on payment.” As stated in the rule, CMS believes the provision of a new technology to a Medicare beneficiary “is a treatment decision, unlike the other addon payments which are excluded by statute (for example, IME and DSH add-ons) that represents a cost to the Medicare program that should be subject to the applicable percent reduction to the base operating DRG payment amount.” Proposed Review and Corrections Process for Claims-Based Measure Rates CMS currently provides hospitals with confidential reports containing the measure rate calculations and accompanying confidential detailed discharge-level information prior to making the rates available to the public. The rule proposes to give hospitals 30 days to review and submit corrections for the claims-based measure rates contained in their confidential reports, beginning the day a hospitals’ information is posted to QualityNet, and that CMS will no longer accept any additional corrections once the 30-day period has ended. 2 Hospital Readmissions Reduction Program Establishment of the Hospital Readmissions Reduction Program was mandated in the Affordable Care Act (PPACA) to reduce payments to certain eligible hospitals to account for excess readmissions. The Hospital Readmission Reduction Program will be effective for discharges beginning on or after October 1, 2012. Key aspects of the program are described below. Payments Payments for discharges from applicable hospitals will be determined from an equation multiplying the base operating DRG payment amount (the payment that would have been made for a discharge in the absence of the Program) by an “adjustment factor” that accounts for excess readmissions. For each hospital, the adjustment factor will be the greater of (a) 1 minus the ratio of the aggregate payments for excess readmissions to aggregate payments for all discharges, or (b) A defined floor adjustment factor: 0.99 for FY 2013; 0.98 for FY 2014; and 0.97 for FY 2015 and subsequent fiscal years. For example, a hospital experiencing high rates of readmissions would have their adjustment factor limited to a 1 percent reduction in FY 2013, but if their readmissions remained high, the adjustment would increase to a 2 percent cut in 2014. On the other hand, a hospital with relatively few readmissions would experience either no adjustment, or an adjustment less than 1 percent. Excess Readmission Ratio calculation For the final rule, the excess readmission ratios will be calculated based on discharges occurring between July 1, 2008 and June 30, 2011. The ratio adjusts for variation across hospitals in patient severity and in the number of patients that a hospital treats. The calculation produces an adjusted actual (or “predicted”) number in the numerator and an “expected” number in the denominator. In other words, the numerator represents aggregate payments for excess readmissions and the denominator represents aggregate payments for all discharges. Applicable conditions As mandated in PPACA, applicable conditions must be “high volume or high expenditure” and have been endorsed by the National Quality Forum (NQF). Conditions for the FY 2013 Program are heart failure (HF), acute myocardial infarction (AMI), and pneumonia (PN). The Secretary is permitted to expand the conditions for the Hospital Readmissions Reduction Program starting in FY 2015. Opportunity to Review and Submit Corrections By June 20, 2012, CMS proposes to deliver via QualityNet confidential reports and accompanying confidential dischargelevel information to applicable hospitals, containing their excess readmission ratios for the three applicable conditions. The information in the reports would be calculated using the claims information available approximately 90 days after the last discharge date in the applicable period. Readmission A “readmission” is defined as when a patient is discharged from an applicable hospital and then admitted to the same or another applicable hospital within 30 days from the date of discharge. Only one readmission during the 30-day period will count as a readmission. Index hospitalizations included in the measure calculation 3 An index hospitalization is defined as a hospitalization evaluated for a possible readmission within 30 days after discharge. The measures exclude any hospitalization for patients with an in-hospital death, without at least 30 days postdischarge enrollment in Medicare fee-for-service (FFS), discharged against medical advice, and under the age of 65. Data sources The finalized measures use Medicare inpatient claims data for Medicare FFS patients 65 years and older. For risk adjustment, the measures use Part A and Part B claims for the 12 months prior to the index hospitalization as well as index hospitalization claims. Exclusion of certain readmissions Certain readmissions that are unrelated to the prior discharge, such as transfers to other acute care facilities and planned readmissions, are excluded. Minimum number of discharges for applicable conditions The minimum number of discharges for applicable conditions is 25 for each condition. Applicable period Claims data over a three-year period (from July 1, 2008, to June 30, 2011) will be used to calculate the excess readmission ratios and to calculate the FY 2013 payment adjustment. 4