Mental health promotion programmes
advertisement

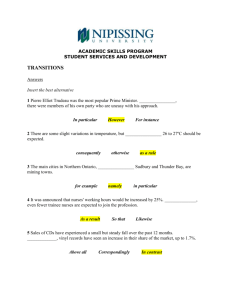
Mental Health Promotion What are the important concepts relating to mental health promotion? An initial search of the literature identified 4 main areas: 1. The interrelated concepts of wellness and positive psychology. 2. The importance of physical health to mental health and the nurses role within this. 3. Mental health promotion across the lifespan. 4. Learning derived from the development of mental health promotion education programmes. 1 1. Review of the concepts of ‘Wellness’ and ‘positive psychology’ in the context of mental health promotion. Louise Doyle (As there is some degree of overlap between this concept and those inherent in ‘recovery’ I have not included papers that refer to ‘recovery’ only as these will be covered by a different work group). ----------------------------------------------------------------------------------------------------------------Introduction Increasing evidence about the high social and economic costs of poor mental health has contributed to a growing recognition of the need to promote positive mental health and wellbeing and to prevent the onset of mental distress (Zechmeister et al., 2008). Although there is no agreed consensus on a universal definition of mental health promotion (Jane-Llopis 2007), most perspectives in some way concur that it involves promoting mental well-being among all age groups of the general population and addressing the needs of those at risk from, or experiencing, mental health difficulties (Department of Health and Children 2006). In recent years mental health promotion has been reconceptualised with a focus now on a positive view of mental health rather than an emphasis on mental illness and deficits (WHO 2004, Barry 2007, Reupert et al 2012). Mental health promotion involves not only minimising the occurrence of mental health problems but also focuses on enhancing positive aspects of daily functioning (Magyary 2002). It involves actions to create living conditions and environments that support mental health and allow people to adopt and maintain healthy lifestyles. These include a range of actions to increase the chances of more people experiencing better mental health. Focusing on factors which are protective of mental health is a critical element of national and international health promotion policies. Protective factors which have a positive influence on our mental health are important to help prevent mental health problems but also to improve the well-being of those experiencing mental distress and to prevent secondary problems (Magyary 2002). 2 Wellness as a paradigm and a mental health promotion approach has gained in popularity in the field of public mental health (Magyary 2002, Swarbrick 2006). This is part of a move away from a traditional medical perspective in which only ‘illness’ was emphasised, towards a more holistic health care model in which ‘wellness’ and ‘wellbeing’ are also highlighted. Wellness is defined as a deliberate process which requires a person to become aware of and make choices for a more satisfying lifestyle leading to improved health (Swarbrick et al 2009). Included within this lifestyle is a balance of healthy habits which focus on nutrition, sleep, exercise, supportive relationships, participation in meaningful activity and avoiding self-destructive behaviour (Swarbrick et al 2009, Swarbrick 2010). In the mental health literature, the concept of wellness is often closely tied to that of recovery for individuals with existing mental health difficulties and while both concepts are closely aligned the concept of wellness is one that has much to offer those who have never experienced a mental health problem. The central focus of wellness is on health, with an emphasis on individuals’ strengths and abilities and their personal responsibility to manage their mental (and physical) health (Swarbrick 2006). Within the wellness perspective, an individual is empowered to manage stressors and difficult situations proactively and is encouraged to self-monitor their own health behaviour. Wellness is not a popular trend, but rather a philosophy that embraces a way of living that helps all people enjoy a more satisfying, productive, and happy life (Swarbrick 2010). Also important to contemporary mental health promotion is the concept of positive psychology. Positive psychology is the science of what is needed for a good life (Slade, 2010) and moves away from the ‘negative bias’ which prevailed in traditional psychology to a focus on well-being and ‘flourishing’ (Boiler et al, 2013). Positive psychology is not only the absence of mental distress, but also the presence of positive psychological resources such as hedonic or subjective well-being (positive affect, life staisfaction, happiness) and eudaimonic well-being (Self-acceptance, positive relations, purpose in life) (Blakeman & Ford, 2012). Within the realm of positive psychology, it is possible to be moderately mentally healthy or even flourishing in the presence of ongoing mental illness (Slade, 2010). Positive psychological interventions are empirically sound and have been found to enhance well-being and ameroliate depressive symptoms (Sin & Lyubomirsky, 2009; Boiler et al, 2013). Included within the realm of postiive psychological interventions are goal-directed thinking, resilence training, positive future 3 thinking, life-coaching and individual and group positive psychotherapy (Boiler et al., 2013). Out comes - what will be realized? Mental health nurses have traditionally worked within the medical model of care focusing their attention on treatment and symptom/illness reduction (Blakeman and Ford, 2012: Slade, 2010; Magyary, 2002). Having wellness and positive psychology as a core component of mental health promotion requires a distinct paradigmatic shift. It requires a new way of thinking about preparation and education for mental health professionals including nurses and will require a change in how they practice if primacy is to be given to increasing well-being rather that to treating illness (Sade, 2010). Health services, and the workers within them, need to be reoriented with a shift on emphasis to health being a shared responsibility among individuals, community groups, health professionals, health service institutions and governments (Jane-Lopis et al., 2005). There is a need to create health-orientated rather than illness-orientated services. How will it be realized? Mental health professionals (nurses) need new approaches to assessment and treatment if the goal is to promote well-being rather than treat illness (Slade, 2010). Mental health professionals (nurses) need to support reasonable goal setting and goal striving (Slade, 2010). Mental health nurses need to become more involved in political activism, working meaningfully with service user and carer groups and engaging with public health campaigns (Blakeman and Ford, 2012). Mental health nurses need to become more involved in promoting social inclusion on a micro and macro scale. Mental health nurses need to take more consideration of the strengths and assets of a person when undertaking a clinical assessment. This is in contrast to traditional assessment which is very much focused on risk and personal deficiencies. 4 What do professionals have to reckon with? Although the literature suggests that service users are open to learning the skills required to promote well-being and positive psychology, there is a learning curve here. This is particularly so for those service users who have essentially been a passive recipient of care and treatment within the parameters of the medical model (through no fault of their own). Not only is a paradigm shift required for nurses and other mental health professionals, but also for some service users for whom these are new concepts. Political activism and critical analysis and discourse around government policies which affect mental health are part of the wellness model (Slade, 2010; Blakeman & Ford, 2012). However, nurses ‘on the ground’ often see these as being the sole domain of the academic community when a much stronger approach is to work in collaboration with academic colleagues to influence the direction of policy that reduces social exclusion for the people with whom they work. What are the challenges? The dominance of the medical model remains a difficulty when striving to develop and support a holistic care plan grounded in the tenets of wellness and positive psychology. Working from a wellness focused perspective requires a change in mind-set in addition to a change in practice. Despite the prominence of well-being in mental health promotion policies, there can be a difficulty in accessing services that promote well-being (Owens et al, 2010). Supporting service users to undertake activity, learning, social connections etc. can be expensive, anxiety-provoking and time-consuming for all concerned (Blakeman & Ford, 2012). Nurses cannot work within the well-being and positive psychology realm in isolation from other mental health professionals; instead, it requires a multidisciplinary team approach with buy-in from each discipline within that team. 5 Nurses are not traditionally educated to be political activists. This requires some consideration in terms of the development of mental health nurse education programmes both at undergraduate and postgraduate levels. Mental health professionals, including nurses, need to be more outward looking in their view of their role, and to construct their job as more than working with individuals (Slade, 2010). Greater interaction is required between mental health professionals who are medically orientated and treatment focused (and who focus more on primary, secondary and tertiary prevention of mental illness) and those workers who are community health-orientated who focus on mental health promotion for the entire population (Jane-Lopis, 2007). Competences Knowledge: Mental health nurses need to have information about the wellness and positive psychology interventions that work and the evidence behind them. MHNs need to know what enhances well-being and alleviates distress. Positive psychology and wellness promote the teaching of positive mental attitudes as an intervention which fosters resilience across the lifespan. Skills: MHNs need to know how to include positive psychology techniques into their clinical work. MHNs need to know how to promote social interaction and activities which have been identified by service users as helping to maintain their sense of well-being (Owens et al., 2010). MHNs need to be able to work with service users in helping them practice and keep a record of positive strategies; helping them incorporate these strategies into everyday life and helping turn these strategies into habits. MHNs need to become skilled at taking a strengths based clinical history with a greater emphasis on the individual’s goals and strengths. 6 Attitudes and Emotional intelligence: MHNs need to reflect and critically appraise how their current practice promotes well-being. MHNs need to be open about a change in thinking and practice to have more focus on well-being and positive psychology. Conclusion Positive mental health is a key asset and resource for population well-being and the long-term social and economic prosperity of society (Barry 2009). Historically, mental health nurses have focused on symptom reduction and as a result relatively little attention was paid to what makes people happy. However, every mental health practitioner needs to be familair with the concept of ‘well-being’ if they are to succeed in the mental health climate of the years to come. References Barry M.M. (2007) Generic principles of effective mental health promotion. International Journal of Mental Health Promotion 9(2), 4-16. Boiler, L., Haverman, M., Westerhof, G.J., Riper, H., Smit, F. & Bohlmeijer, E. (2013) Positive psychology interventions: a meta-analysis of randomized controlled studies. BMC Public Health, 13, 119 Blakeman, P. & Ford, L. (2012) Working in the real world: a review of sociological concepts of health and well-being and their relation to modern mental health nursing. Journal of Psychiatric and Mental Health Nursing, 19, 482-491. Department of Health and Children (2006) A Vision for Change: Report of the Expert Group on Mental Health Policy. The Stationery Office, Dublin. Jane-Lopis, E., Barry, M., Hosman, C. & Vikram, P. (2005) Mental health promotion works: a review. Promotion and Education, 12:9. Jane-Llopis E. (2007) Mental health promotion: Concepts and strategies for reaching the population. Health Promotion Journal of Australia 18(3), 191-197. 7 Magyary, D. (2002) Positive mental health: A turn of the century perspective. Issues in mental health nursing, 23:331-349 Millar, S.L. & Donnelly, M. (2013) Promoting mental wellbeing: developing a theoretically and empirically sound complex intervention. Journal of Public Health, 1-10. Owens, C., Crone, D., Kilgour, L. & El Ansari, W. (2010) The place and promotion of wellbeing in mental health services: a qualitative investigation. Journal of Psychiatric and Mental Health Nursing, 17, 1-8. Reupert A., McHugh C., Mayberry D. and Mitchell D. (2012) Training mental health promotion workers in programme evaluation. Journal of Psychiatric and Mental Health Nursing 19(1), 31-39. Sin, N.L., & Lyubomirsky, S. (2009) Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: A practice-friendly meta-analysis. Journal of Clinical Psychology, 65(5), 467-487. Slade, M. (2010) Mental illness and well-being: the central importance of positive psychology and the recovery approaches. BMC Health Services Research, 10:26 Swarbrick M. (2006) A wellness approach. Psychiatric Rehabilitation Journal 29(4), 311314. Swarbrick M. (2010) Wellness: A practice for our lives and work. Journal of Psychosocial Nursing and Mental Health Services 48(7), 1-3. Swarbrick M., Roe D., Yudof J. and Zisman Y. (2009) Participant perceptions of a peer wellness and recovery education program. Occupational Therapy in Mental Health 25(34), 312-324. World Health Organization (2004) Promoting Mental Health: Concepts, Emerging Evidence, Practice. WHO, Geneva. Zechmeister I., Reinhold K., McDaid D. and MHEEN Group (2008) Is it worth investigating in mental health promotion and prevention of mental illness? A systematic review of the evidence from economic evaluations. BMC Public Health 8(20). 8 2. The importance of physical health to mental health and the nurses role within this. Henrika Jormfeldt Introduction Individuals with serious mental illness have higher rates of physical illness and are more likely to experience premature death than the general population (Blyte & White, 2012). Literature describing healthcare programmes for mental health consumers demonstrates that such programmes regularly result in significant improvements in healthcare access and health outcomes. Nurse-led strategies to improve physical healthcare in mental healthcare services could potentially reduce these inequalities since mental health nurses, as the largest professional group working in mental health care, have a key role in supporting enhanced physical health and well-being of people with mental illness (Happell, Platania‐Phung, & Scott, 2014; Verhaeghe et al., 2013). Through health-promotion strategies, alongside recovery-focused support aimed at avoiding deteriorating physical health, mental health nurses can significantly contribute to improving the current rate of premature death experienced by people with long-term mental illness (Blythe1 & White, 2012; Hardy & Thomas, 2012). Mental health nurses are well placed to provide person-centred, transitional care, so commonly absent from the experience of many service users. The ambition of this paper has been to look at a range of contemporary literature on the topic of the mental health nurses role in physical health related to mental health at master level. Out comes - what will be realized? Physical health outcomes of health care programmes include improvements in health behaviours such as substance use, cardiometabolic health measures such as cholesterol, blood pressure and blood glucose. Health care programmes also have been shown to improve aspects of mental health including perceived mental functioning, social functioning and self-esteem (Happell, Platania‐Phung & Scott, 2014). Mental health nurses have a key role in supporting enhanced physical health and well-being of people with mental illness. However there is a question of role ambiguity for mental health nurses, many of whom feel that physical care is outside their remit and expertise. Patients in mental health service identify that their physical symptoms are often dismissed by mental health nurses as part of their mental health problem. Hence mental 9 health nurses in practice require further skills and training in the area of physical health care. How will it be realized? The literature is illustrative of a growing role of nurses within mental healthcare in lifestyle programme delivery and management or co-ordination roles related to the mental health nurses’ holistic approach to care of consumers with severe mental illness (Happell, Platania‐Phung & Scott, 2014). Mental health nurses reporting of physical healthcare could routinely use a suitable taxonomy to clearly delineate the role of mental health nurses. Mental health nurses need knowledge and training in physical health care in order to handle lack of readiness and motivation to change unhealthy lifestyle behaviour among mental health patients to be able to discuss lifestyle issues with their patients in a constructive and inspiring manner Mental health nurses need education to be able to take the responsibility to implement and carrying out lifestyle programmes and care co-ordination as well as management of educational sessions targeting and healthy eating and physical activity. Mental health nurses have the advantage of an existing skill set from working with this client group, having often already established effective therapeutic relationships. Additional training and knowledge in physical health care is likely to put them in a prime position to help reduce morbidity and death rates of people with severe mental illness. Where do professionals have to reckon with? Nurses may have to deal with patients with lack of motivation or energy to focus on healthy lifestyle behaviour as a result of the severity of the mental suffering. Admission to an inpatient mental healthcare facility could be identified by some patients as a barrier to focus on healthy lifestyle behaviour. Mental health nurses may lack of knowledge/training in physical health care. 10 The mental health care system may lack of useful measure to establish more precisely what physical care nurses are doing. Mental health nurses commonly report lack of time as an important issue. Views and attitudes of the society could be a barrier to integrate individuals with severe mental illness into sport clubs or leisure time organisations and activities in society. Mental health nurses may be confident in carrying out routine physical health checks but less confident in regards to screening and interpreting physical health results. Mental health nurses may hold the traditional view in the nurse/doctor power relationship, whereby nurses are viewed as being subordinate to doctors resulting in nurses don’t take full responsibility It can be questioned to what extent lifestyle choices is the responsibility of the patient or the mental health nurse. Mental health nurses could experience a conflict between follow the patients in their own process of defining their own needs and desires regarding health issues and the standards of treatment policies What are the challenges? Traditionally mental health nurses have not seen physical health as their main concern and physical health problems among patients with severe mental illness have often been mistaken for symptoms of mental illness. Mental health nurses need to make themselves more visible to carers as a resource for support and education regarding overall health issues. Mental health nurses need to acknowledge that health promotion from a holistic view is integral to their roles. There is a tradition of stigma and discrimination in society but all patients require access to health services that do not differentiate or discriminate. 11 Competences Knowledge: Mental health nurses need to have knowledge and awareness of how to promote physical health in order to handle lack of readiness and motivation among patients with severe mental illness. Mental health nurses have to be able to face taboos and prejudices in society. Otherwise as a consequence, patients with mental illness may fear or have no longer the motivation to integrate into society to practice sports or other activities to stimulate health. Skills: Mental health nurses in practice require further skills and training in the area of physical health care to comprehend a holistic approach to care of consumers with severe mental illness Mental health nurses have to be able to integrate health-care provision for people with mental illness by cooperation with health care providers, health agencies and the general public. Mental health nurses should have the necessary skills to motivate and support people to improve their wellbeing, and to offer advice on how to prevent further physical health deterioration. Mental health nurses must be able to follow the patients in their process of defining their own needs and desires, and at the same time communicate with regimen of treatments. 12 Attitudes and Emotional intelligence: Mental health nurses must see the importance of strengthen the patients’ ability to trust themselves through making their own decisions and taking the consequences of these decisions with support. Mental health nurses have to understand the importance of tackling stigma and discrimination and that all patients require access to health services that do not differentiate or discriminate. Mental health nurses have to value and appreciate a holistic approach to care of consumers with severe mental illness Conclusion A major public health issue that can be addressed through improved physical healthcare access and delivery is the gap between physical health of people with and without severe mental illness. The barriers to physical healthcare services, whether in inpatient settings or in the general community, are significant for people with severe mental illness and a healthcare reform is necessary if inequalities in health are to be reduced. It is a challenge for the contemporary world for further promoting population health and well-being, as strategies to improve health care have the potential to improve health and well-being that enable people to live life to the best of their abilities. Nurses, as a major professional group in mental healthcare, will be critical to re-organizing health services to better support people with severe mental illness in recovery and well-being. References Blythe, J. & White, J. (2013) Role of the mental health nurse towards physical health care in serious mental illness: An Integrative Review of 10 years of UK Literature. International Journal of Mental Health Nursing, 21(3), 193-201. Happell, B. Platania‐Phung, Chris. & Scott, D. (2014). Proposed nurse‐led initiatives in improving physical health of people with serious mental illness: a survey of nurses in mental health. Journal of Clinical Nursing, 23(7-8), 1018 – 1029. 13 Happell, B., Platania‐Phung, C., & Scott, D. (2014). A systematic review of nurse physical healthcare for consumers utilizing mental health services. Journal of Psychiatric and Mental Health Nursing, 21 (1), 11 – 22. Hardy, S., & Thomas, B. (2012). Mental and physical health comordibity: Political imperatives and practice implications. International Journal of Mental Health Nursing, 21(3), 289 – 298. Verhaeghe, N., De Maeseneer, J., Maes, L., Van Heeringen, C., & Annemans, L. (2013). Health promotion in mental health care: perceptions from patients and mental health nurses. Journal of clinical nursing, 22(11-12), 1569 – 1578. 14 3. Review of the MHP across the lifespan Päivi Vuokila-Oikkonen ----------------------------------------------------------------------------------------------------------------- Introduction In these studies, mental health promotion is about enhancing positive emotion and optimal functioning. Health is not only the absence of illness but rather means to harness resources of individuals and societies and the factors that make life good. Mental health promotion should aims to increase the ability of an individual to have a good self-esteem, autonomy, wellbeing and inclusion in social activities. The promotion of mental health also aims to strengthen a person’s capacity to deal with adversity and shift of focus should be from treatment of illnesses to prevention of anxiety, depression and behavioural problems and promotion of mental health. Mental health interventions and promotive actions are aimed at improving both mental and physical health. The asset-based paradigms of positive psychology may offer new approaches for bolstering psychological resilience and promoting mental health. A working approach is to include mental health promotion in the existing health promotion programs. Mental health promotion in schools includes information and training on self-harm, interactional skills, social skills, stress, coping skills, school bullying and understanding mental wellbeing and understanding of diversity. The nurses working in schools are the tools that put these actions into practice. Focusing mental health promote interventions on children’s’ and adolescents’ is important. Mental health promotion aims to increase the individual and communal capacity to understand and respond to mental health issues. It also aims to promote the mental health of the whole population. Let’s talk about Child Discussion and the Network meeting is one effective method when prevention mental health among children and adolescents. Out comes - what will be realized? Mental health promotion of lifespan should not be detached from the community but a function of the community. Nurses and nurse students are needed to counselling skills when moving from core of caring to core of mental health promotion work. Resiliency is the process of positive adaptation in the context of adversity or risk. Resiliency helps people to 15 cope with life’s challenges and confers a sense of mastery over one’s life. Promotion of resiliency can occur within persons (e.g., coping, optimism), among persons (social support), and across social levels (public health or educational systems). Education in mental health promotion frameworks for practice are required at undergraduate, postgraduate and current clinical practice levels to ensure knowledge and understanding of mental health promotion is disseminated across the profession. How will it be realized? There exist programs which are evidence-based and have proven to be effective. The good evidence-based promotion and prevention programs implemented with fidelity strengthen parenting and build child resilience. Mental health promotion interventions are delivered at three levels: universal, which is an intervention that affects the whole school or community, selective, which is an intervention focusing on a certain group of students, and indicated, which an individually focused intervention is. Parenting interventions and preschool interventions are effective in boosting resiliency in mothers and children. Interventions to prevent mental disorders and psychological symptoms in the offspring of parents with mental disorders appear to be effective. Let’s talk about Child Discussion and the Network meeting is one effective method for mental health prevention among children and adolescents. Researches show that by providing social activities and enhancing social networking, quality of life and life satisfaction increase and depressive symptoms decrease among older people. Where do professionals have to reckon with? Mental health promotion of children and adolescents should not be detached from the community but a function of the community. Social support and trust may be important factors to consider when developing interventions to promote mental health and prevent mental disorders among older adults. When adults or children have personally experienced traumatic events and have psychological and/or behavioural symptoms or explicit difficulties. Yet, it is known that children in families with parents serve illness, even have 2-4 times elevated risk for 16 psychiatric and behavioural problems. Furthermore, effective preventive interventions are available. One such intervention is the Let’s Talk about Children (LTC), What are the challenges? Traditionally mental health nurses have studied to be nursing and caring. However mental health promotion and prevention approaches allow mental health nurses to provide services to a significant number of people in communities including those involved with young people, such as teachers, other health professionals and families. Nurses can contribute to the mental health and wellbeing of whole populations of young people while providing vital linkages across settings such as health, education, employment, and welfare which young people transverse during their lives. Mental health promotion and consultation roles could also provide new areas of expanded nursing practice in mental health promotion. Mental health promotion work basis on counselling approach and methods. There are challenges in considering a move towards mental health promotion, coaching and consultation roles. Positive and resources based approaches offer new approaches for bolstering psychological resilience and promoting mental health. The challenge is how to translate this evidence of mental health promotion and prevention into nurses’ everyday practices in their professional working life. Nurse students are needed to counselling skills when moving from core of caring to core of mental health interventions like coaching. Competences Knowledge: Mental health is not only the absence of illness but rather means to harness resources of individuals and societies and the factors that make life good. Mental health promotion should aims to increase the ability of an individual to have a good self-esteem, autonomy, wellbeing and inclusion in social activities. Need to recognize that mental health promotion is about enhancing positive emotion and optimal functioning. To understand what is resilience. Mental health promotion work includes universal, selective, and individually focused interventions. 17 The Let’s Talk about Children (LTC) intervention and Network Meeting methods. Skills: To coach individuals according to positive way of thinking, how they interpret day-to-day events and their interactions with others. Coaching includes learning skills for more optimistic ways of thinking and reacting to improve their resiliency. Universal, selective and indicated interventions as follows: Universal intervention In action Whole school events “Mental health rally”- a whole school event for distribution of information on mental health, School environment is improved by educating school staff on mental health issues and providing skills to identify, intervene and cope with different emotional and behavioral need. Sharing of knowledge In “mental health kiosk”, information letters trough the school intra, parental meetings “Low threshold”-places nurses associate with student at free time ex. in the school lobby, walk-in times Education of school staff Staff meetings Selective interventions Classroom interventions Lessons on ex. taking care of mental health, substance abuse, stress, friendship, social skills, crisis, interactional skills, classroom environment Groups ART (aggression replacement treatment), mastery of life skills, social skills Indicated interventions 18 Support for students and families Supportive and solution focused dialogue with student or families Parent consultation Assessment with multiprofessional team Also it is needed to skill for group leader by using mental health promotion strategies and goals. To skills to use Let’s talk about Child Discussion and the Network. LTC is a low threshold discussion with parents to identify both strengths and vulnerabilities in the child’s life and to make a plan how to strengthen protective factors and to support the child in vulnerabilities. Furthermore to use, if it is needed, LTC Network Meeting, this gathers those people (e.g. family’s own social network, the teacher, different professionals as needed) who will be able to support the child and the family. In the meeting, the participants plan and make commitments to strengthen those protective factors and to give support in those vulnerabilities which were identified during LTC discussion. Among older adults it is needed to promote social interaction and social support that may confer greater psychological resiliency. Recognize and focus on peoples’ strengths and resources. Listen, hear and dialogue skills when working with groups and cooperation with people in lifespan and multiprofessional teams. Reflective skills is needed. Attitudes and Emotional intelligence: Need to have a positive attitude and flexibility to work in field of communities and school. Need to be open to recognize mental health promotion interventions and do use it. To shared knowledge among the parents when using LTC- methods. Need to display empathy and understanding. 19 Conclusion Mental health promotion work needs new developed and evaluated intervention methods. Mental health nurses need to learn to work in fields like school and community. Motivation to change nurses’ ways of thinking when moving from psychiatric nurse as caring people to mental health work as coaching people to use their own resources . Furthermore field of Internet interventions is growing. It is needed to take account. References Forsman,A.K.; Nyqvist,F.; Wahlbeck,K. 2011. Cognitive components of social capital and mental health status among older adults: a population-based cross-sectional study. Scandinavian Journal of Public Health. Niemelä M, Repo J, Wahlberg KE, Hakko H, Räsänen S. Pilot evaluation of the impact of structured child-centered interventions on psychiatric symptom profile of parents with serious somatic illness: struggle for life trial. J Psychosoc Oncol. 2012;30(3):316-30. Kobau, Rosemarie & Seligman, Martin E. P. & Peterson Christopher & Diener, Ed & Zack, Matthew M. & Chapman, Daniel & Thompson, William (2011) Mental Health Promotion in PublicHealth: Perspectives and Strategies From Positive Psychology. American Journal of Public Health.August 2011, Vol 101, No. 8 Power, A. 2010. Kathryn Transforming the Nation’s Health: Next Steps in MentalHealth Promotion. American Journal of Public Health. December 2010, Vol 100, No. 12 Onnela A, Vuokila-Oikkonen P, Ebeling Hanna, Hurtig M. 2014 Mental health promotion in a school environment. Journal of Psychiatric and Mental Health Nursing. 21 (7), 618-627. Solantaus T, Paavonen EJ,,1 Toikka S, Punamäki R-L Preventive interventions in families with parental depression: children’s psychosocial symptoms and prosocial behaviour Eur Child Adolesc Psychiatry. Dec 2010; 19(12): 883–892. 20 Woodhouse, Annette. Is there a future in mental health promotion and consultation for nurses? Contemporary Nurse (2010) 34(2): 177–189Volume 34, Issue 2, February/March 2010 21 4. Mental Health Promotion Programmes: Mari Lahti & Heikki Ellila Mental health promotion programmes Name, developer Lennox et al. 2007. Effects of a comprehensive health assessment programme for Australian adults with intellectual disability: a cluster randomised trial. Fitzpatrick et al. 2013. Enhancing the mental health promotion component of a health and personal development programme in Irish schools. Aim Aim was to increase beneficial patterns of general practice-driven activities. Content Health assessment programme (CHAP) is a 21page booklet about health assessment for cares and GP’s and adults with intellectual disability. Aim was to seek whether The social, personal and students participating in health education programme. SHPE had better outcomes Programe contains several in terms of help seeking, models that are relevant to emotional and behavioral mental health promotion difficulties and their view of including communication, school social environment. belonging and integrating, relationships and emotional health. To who? Intellectual disability people Where? Australia School aged children aged between 12-16 years Ireland Badri et al. 2013. Promoting Darfuri women’s psychosocial health: developing a war trauma counsellor training programme tailored to the person. Aim was to promote a new philosophy in the Sudanese mental health care by introducing an integrative approach for targeted prevention and tailored treatments to the Darfuri person in a costeffectively way. Aim was to promote positive mental health for War trauma counselor programme 13 themes, forexample, need assessment, recognizing the stress, mental health assessment and psychoeducation. Professionals, people who work in Darfuri was area as war trauma councelors Mind Out curriculum. It consist 13 classroom School aged children aged between 15-18 Byrne et al. 2004. Implementation of a school- 22 Outcomes Health promotion Disease prevention Case-finding activities Appropriate interventions The strengths and difficulties questionnaire (SDQ) The children’s coping strategies checklist (CCSC) Help seeking questionnaire “What is your school like” questionnaire Netherlands - Ireland. Questionnaires for students based mental health promotion programme in Ireland. young people. sessions over two years. Themes are for example, support, stress and coping, emotions and understanding of mental health. Tubach et al. 2012. A homevisiting intervention targeting determinats of infant mental health: the study protocol for the CAPEDP randomized controlled trial in France. Aim is to evaluate young mothers presenting vulnerability factors associated with greater likehood of child mental health disorders. Vancampfort et al. 2012. International organization of physical therapy in mental health consensus on physical activity within multidisciplinary rehabilitation programmes for minimizing cardio-metabolic risk in patients with schizophrenia. Conley et al. 2013. An evaluation review of outcome research on universal mental health promotion and prevention programs for higher education students. Aim was to improve physical activity within rehabilitation programmes for people with schizophrenia. Parental skills and Pregnant womes (12- France attachment in early childhood: 17 weeks). reduction of risks linked to mental healthproblems and promotion resilience (CAPEDP) has two specificities 1. address child mental health promotion 2. it was conducted by psychologist. Schizophrenia Australia patients Aim was to review and evaluate higher education promotion and prevention programs for students. Review identified 83 studies where focus was on promotion and prevention. 23 years Higher education students USA School ethos questionnaire activity-based evaluation workshop for students Process questionnaire for teachers Group reviewsession for teachers 18 outcome questionnaires were listed in the protocol (see the article) - Social and emotional skills Self-perception Emotional distress Aboud 2007. Evaluation of an Early Childhood Parenting Programme in Rural Bangladesh Sin et al. 2008 An evaluation of education and implementation of psychosocial interventions (PSI) within on UK mental health trust To promote physical and mental development of children by educating poor mothers in age-appropriate responsive stimulation and feeding. To examine on local level ( in one Trust) the factors which support and limit the education and practice of PSI programs Eaton & Agomoh (2007) The impact of community-based mental health awareness programme To encourage people with mental health problems to get contacted with prober mental health services and reduce stigma on these people. Millar & Donelly (2013) Promoting mental wellbeing: developing theoretically and empirically sound complex intervention. To promote mental health well-being and prevent the development of mental disorders of people showing early sign of mental difficulties 170 mothers in 1 year parent education and control group 159 with no education. 1) Test of childrearing and 2) Home observation Mothers and children in rural areas Bangladesh Mothers in test group scored higher point in both observations. Differences not significant 2 questionnaires to evaluate education and implementation of PSI program 1) Staff(n=17) 2) Managers (n=11) 50 voluntary mental health village workers were educated and they informed 2260 individuals about issues concerning mental health / services in three states (4 years Mental health awareness) program). development of a 12 week early Intervention mental wellbeing program for people showing signs of mental difficulties Professionals of particular Mental Health Trust UK There were several factors supporting and hindering the education and implementation the PSI program. General public Nigeria Significant increase in the number of patients attending the community psychiatric clinic Services user in voluntary sector and in primary care Belfast Northern Ireland Significant increase in mental health wellbeing among those participated in the program. 24