Massive Transfusion and Blood Products
advertisement
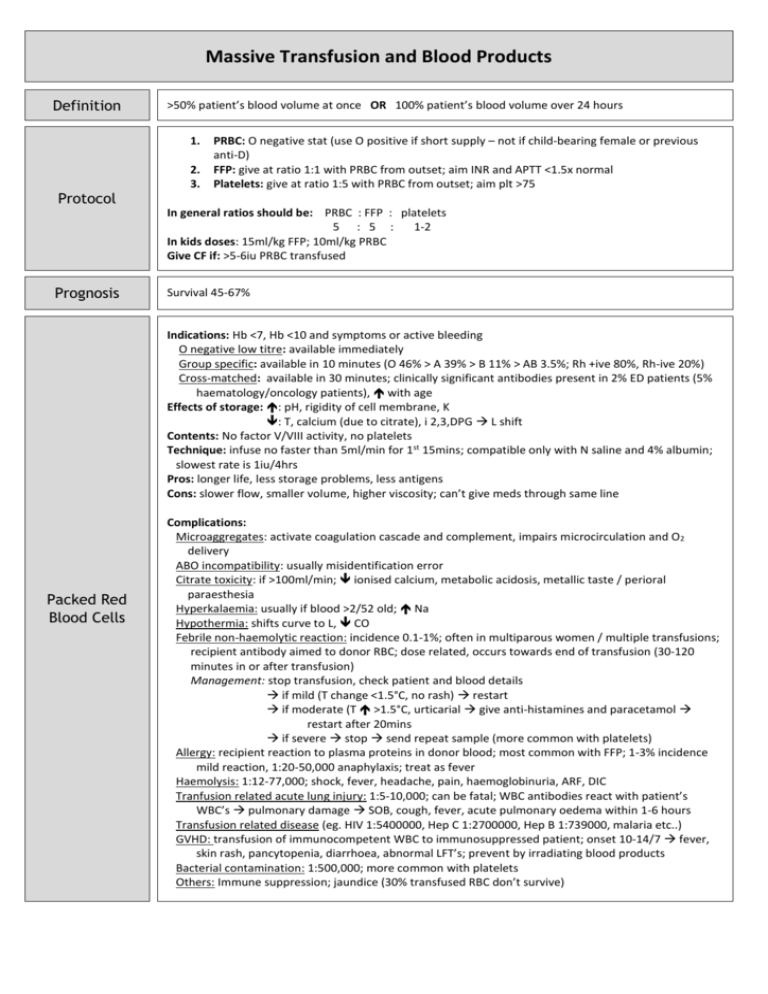
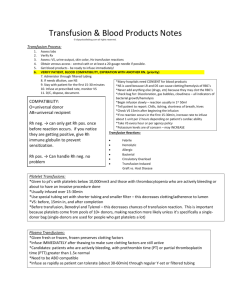
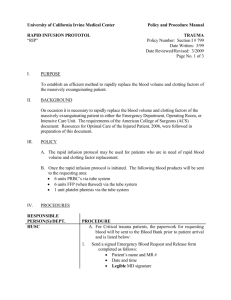
Massive Transfusion and Blood Products Definition >50% patient’s blood volume at once OR 100% patient’s blood volume over 24 hours 1. Protocol 2. 3. PRBC: O negative stat (use O positive if short supply – not if child-bearing female or previous anti-D) FFP: give at ratio 1:1 with PRBC from outset; aim INR and APTT <1.5x normal Platelets: give at ratio 1:5 with PRBC from outset; aim plt >75 In general ratios should be: PRBC : FFP : platelets 5 : 5 : 1-2 In kids doses: 15ml/kg FFP; 10ml/kg PRBC Give CF if: >5-6iu PRBC transfused Prognosis Survival 45-67% Indications: Hb <7, Hb <10 and symptoms or active bleeding O negative low titre: available immediately Group specific: available in 10 minutes (O 46% > A 39% > B 11% > AB 3.5%; Rh +ive 80%, Rh-ive 20%) Cross-matched: available in 30 minutes; clinically significant antibodies present in 2% ED patients (5% haematology/oncology patients), with age Effects of storage: : pH, rigidity of cell membrane, K : T, calcium (due to citrate), i 2,3,DPG L shift Contents: No factor V/VIII activity, no platelets Technique: infuse no faster than 5ml/min for 1st 15mins; compatible only with N saline and 4% albumin; slowest rate is 1iu/4hrs Pros: longer life, less storage problems, less antigens Cons: slower flow, smaller volume, higher viscosity; can’t give meds through same line Packed Red Blood Cells Complications: Microaggregates: activate coagulation cascade and complement, impairs microcirculation and O2 delivery ABO incompatibility: usually misidentification error Citrate toxicity: if >100ml/min; ionised calcium, metabolic acidosis, metallic taste / perioral paraesthesia Hyperkalaemia: usually if blood >2/52 old; Na Hypothermia: shifts curve to L, CO Febrile non-haemolytic reaction: incidence 0.1-1%; often in multiparous women / multiple transfusions; recipient antibody aimed to donor RBC; dose related, occurs towards end of transfusion (30-120 minutes in or after transfusion) Management: stop transfusion, check patient and blood details if mild (T change <1.5°C, no rash) restart if moderate (T >1.5°C, urticarial give anti-histamines and paracetamol restart after 20mins if severe stop send repeat sample (more common with platelets) Allergy: recipient reaction to plasma proteins in donor blood; most common with FFP; 1-3% incidence mild reaction, 1:20-50,000 anaphylaxis; treat as fever Haemolysis: 1:12-77,000; shock, fever, headache, pain, haemoglobinuria, ARF, DIC Tranfusion related acute lung injury: 1:5-10,000; can be fatal; WBC antibodies react with patient’s WBC’s pulmonary damage SOB, cough, fever, acute pulmonary oedema within 1-6 hours Transfusion related disease (eg. HIV 1:5400000, Hep C 1:2700000, Hep B 1:739000, malaria etc..) GVHD: transfusion of immunocompetent WBC to immunosuppressed patient; onset 10-14/7 fever, skin rash, pancytopenia, diarrhoea, abnormal LFT’s; prevent by irradiating blood products Bacterial contamination: 1:500,000; more common with platelets Others: Immune suppression; jaundice (30% transfused RBC don’t survive) Fresh Frozen Plasma Cryoprecipitate Platelets Prothrombinex Factor VIIa Available in 30 minutes Indications: haemorrhage and coagulopathy; reversal of warfarin overdose; factor deficiency; antithrombin III deficiency; TTP; can be used in Haemophilia A and B in emergency if no pure factor available (although risk of volume overload) Compatibility requirement: requires ABO compatibility Contents: all clotting factors and fibrinogen Technique: give at 10ml/min (ie. Over <1 hour); give 4-6iu per 5L blood Available in 30 minutes Indications: bleeding and fibrinogen <1 Compatibility requirement: better if ABO compatibility Contents: clotting factors VIII and XIII, fibrinogen, von-Willebrand factor; no factor IX (so can be used in Haemophilia A but not B in emergencies, although would be risk of fluid overload in amounts required) Technique: give at 10ml/min (ie. Over <1 hour); give 1iu / 10kg body weight Available in 15-30 minutes; 1iu platelets by 5 Indications: platelets <10 <20 and fever / antibiotics / evidence of systemic haemostatic failure <50 and bleeding (or skin bleeding time >2x normal) or surgery <100 and for eye / neurological surgery DIC / ITP with life-threatening haemorrhage Compatibility requirement: does not require ABO compatibility Technique: give 1-2iu per 5L blood Cons: can only be stored 3/7 Duration of action 12-24 hours Indications: congenital clotting factor deficiency, warfarin overdose and significant bleeding Compatibility requirement: ABO compatibility not required Contents: clotting factors II, V, VII, IX and X; anti-thrombin and heparin Technique: give 3ml/min; give 25-50iu/kg (50iu if INR >6, 35iu if INR 4-6, 25iu if INR 2-4) Pros: small volume, rapid administration, no time delay in thawing (unlike FFP), no ABO typing (unlike FFP), INR reversal within 15 minutes, no disease transmission Not demonstrated to improve any clinically significant outcomes in trials; mortality in blunt trauma in CONTROL trial, expensive, requires normal pH and T to be effective; 5% absolute risk of VTE; give 90120mcg/kg Indications: last resort in generalised bleeding only after control of bleeding obtained; inhibitors to clotting factors VIII/X; congenital clotting factor VII deficiency; Glanzmann’s thrombasthenia