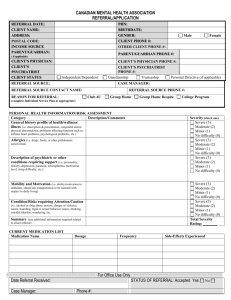
Appendix 2 : Referral Criteria These referral criteria are designed to
advertisement

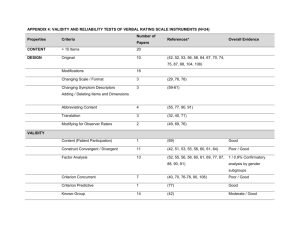
Appendix 2 : Referral Criteria These referral criteria are designed to advise referrers and support practitioners in developing a service for children / young people and their families. They are not intended to be exhaustive and the clinical judgment and professional accountability of practitioners is recognised and supported by the service. The service does not work with CYP with a primary diagnosis of Eating Disorder; these services are provided by the countywide Eating Disorder Service. Children and Young People with a learning disability may receive a service within any of the teams, those requiring a specialist service will be supported by specialist staff within the Level 3 team. Universal (Level 1) services 2gether’s Children & Young People Service works in partnership with all statutory services working with children and young people within Gloucestershire. These universal services form part of a pathway providing C/YP with emotional support as the need arises in response to life changes and events. These services are generally able to support C/YP experiencing : • Behaviour problems consistent with their stage of development • Mild to moderate anxiety • Mild to moderate depression • Emotional issues arising from life events The service will offer advice, consultation, support and supervision via Primary Mental Health Workers and the practitioner advice line with the aim of enabling the support to continue to be led by universal services. The service also offers a range of training to practitioners working within universal services. Service Referral Criteria Team Service Element Criteria Will be present Core PMH Primary Mental Health (PMH) Hospital Education / Paediatric Liaison Infant Mental Health Parents of children with behavioural difficulties who are willing to participate in a group programme to increase their skills and confidence. As Core PMH Must be in receipt of Hospital Education Services or in the care of Gloucestershire Hospitals Trust Paediatric Services Age 0-2 years Infant’s long term mental health is identified as being at serious risk of harm Must be in receipt of Statutory Youth Offending Service and score 2 or above on ASSET and have a SQIFA completed Child Protection procedures should be in place Vulnerable Children Service Youth Offending Service Understanding Sexual behaviour Moderate mental health issues which have either not been successfully managed within universal services or which are significantly affecting a C/YP’s functioning. An identified need for an assessment of mental health, with a view to developing a programme of short term interventions Parenting Programme May be present Presence of serious mental illness within parents Infants at risk of entering care system Complex Engagement Looked After Children Family Court Assessment ‘Keep Safe’ work should have been completed C/YP must have an allocated social worker Sexually harmful behaviour which is beyond the capability of universal services to safely manage History of non-engagement or needs more intensive support than can be provided by level 3 Must be Looked After, on the edge of care, in kinship care or in special guardianship arrangements. Requires clinical advice and support of pre-adoption / fostering arrangements Or Requires clinical advice and support to improve placement stability Referrals will only be received in writing from GCC legal services department for family court assessment. Client/siblings should not have current contact with any service element within 2 gether CYPS Requires routine domiciliary/community visits Requires support by more than one agency Non-intensive approach is likely to lead to non-engagement and poor long term mental health outcomes. Learning Disability Level 3.5 Level 3 / 3.5 Core Level 3 Reduced ability to understand new / complex information with impaired social / adaptive functioning. In receipt of special education in any of the county special schools Sleep / Behavioural/ Mental health / concurrent epilepsy difficulties which are significantly affecting functioning Moderate to severe mental health need with concurrent high level of complexity and/or clinical risk. Level of need exceeds the resources of L3 care coordinator / MDT Mental Health problems significantly affecting functioning Problem has not been resolved within universal / L2 services or is moderate to high risk / complexity Or Problem is complex and requires multidisciplinary assessment / intervention. Mental Health hospital admission may be being considered. May have recent history of DSH and have been admitted to hospital via the Emergency department