Emory Family Practice Residency Curriculum
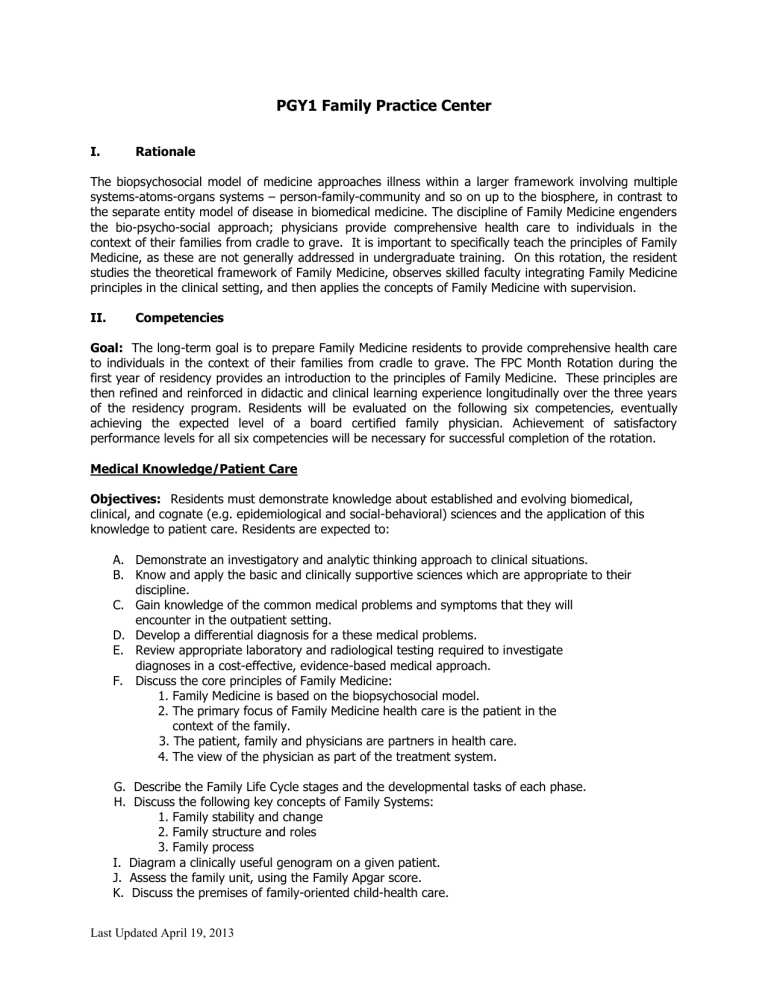
PGY1 Family Practice Center
I. Rationale
The biopsychosocial model of medicine approaches illness within a larger framework involving multiple systems-atoms-organs systems – person-family-community and so on up to the biosphere, in contrast to the separate entity model of disease in biomedical medicine. The discipline of Family Medicine engenders the bio-psycho-social approach; physicians provide comprehensive health care to individuals in the context of their families from cradle to grave. It is important to specifically teach the principles of Family
Medicine, as these are not generally addressed in undergraduate training. On this rotation, the resident studies the theoretical framework of Family Medicine, observes skilled faculty integrating Family Medicine principles in the clinical setting, and then applies the concepts of Family Medicine with supervision.
II. Competencies
Goal: The long-term goal is to prepare Family Medicine residents to provide comprehensive health care to individuals in the context of their families from cradle to grave. The FPC Month Rotation during the first year of residency provides an introduction to the principles of Family Medicine. These principles are then refined and reinforced in didactic and clinical learning experience longitudinally over the three years of the residency program. Residents will be evaluated on the following six competencies, eventually achieving the expected level of a board certified family physician. Achievement of satisfactory performance levels for all six competencies will be necessary for successful completion of the rotation.
Medical Knowledge/Patient Care
Objectives: Residents must demonstrate knowledge about established and evolving biomedical, clinical, and cognate (e.g. epidemiological and social-behavioral) sciences and the application of this knowledge to patient care. Residents are expected to:
A.
Demonstrate an investigatory and analytic thinking approach to clinical situations.
B.
Know and apply the basic and clinically supportive sciences which are appropriate to their discipline.
C.
Gain knowledge of the common medical problems and symptoms that they will encounter in the outpatient setting.
D.
E.
Develop a differential diagnosis for a these medical problems.
Review appropriate laboratory and radiological testing required to investigate diagnoses in a cost-effective, evidence-based medical approach.
F.
Discuss the core principles of Family Medicine:
1. Family Medicine is based on the biopsychosocial model.
2. The primary focus of Family Medicine health care is the patient in the
context of the family.
3. The patient, family and physicians are partners in health care.
4. The view of the physician as part of the treatment system.
G. Describe the Family Life Cycle stages and the developmental tasks of each phase.
H. Discuss the following key concepts of Family Systems:
1. Family stability and change
2. Family structure and roles
3. Family process
I. Diagram a clinically useful genogram on a given patient.
J. Assess the family unit, using the Family Apgar score.
K. Discuss the premises of family-oriented child-health care.
Last Updated April 19, 2013
Learning Activities
Attending Rounds
Multidisciplinary Rounds
Grand Rounds
Sub-Specialty
Conference
X
X
Evaluation Methods
X Attending Evaluation
X
X
L. Discuss the uses and indications for a home visit.
M. Discuss the signs and symptoms and management of clinical depression.
N. Discuss the signs and symptoms and management of anxiety.
O. Demonstrate the following skills in history taking:
1. Biopsychoscocial approach (assessment of pertinent psychosocial factors)
2. Screening for anxiety and depression
Morning Report
Didactics
Other
Program Director
Review
360 ᵒ evaluation
Other
X
Research Conference
Videotape Review
X Outpatient Clinics
Ethics/Comm Conference X Direct Patient care
Specialty Conference
Noon Conference
X Faculty Supervision
X Procedures
X Directly Supervised
Procedures
X In-Training Exam
X
X
X
Resident Seminar
Journal Club
Readings
Morning Report
Faculty Supervision and Feedback
X Quarterly Review
Professionalism
Objectives: Residents must demonstrate a commitment to carrying out professional responsibilities, adherence to ethical principles, and sensitivity to a diverse patient population. Residents are expected to:
A.
Demonstrate respect, compassion, and integrity; a responsiveness to the needs of patients and society that supersedes self-interest; accountability to patients, society, and the profession; and a commitment to excellence and on-going professional development.
B.
Demonstrate a commitment to ethical principles pertaining to provision or withholding of clinical care, confidentiality of patient information, informed consent, and business practices.
C.
Demonstrate sensitivity and responsiveness to patients' culture, age, gender, and disabilities.
D.
E.
Arrive at the clinic in a timely fashion.
Work effectively as a member of a team.
F.
Respect patient privacy by guarding medical records and discussion of personal information about patients.
G.
Assist patients and their families in planning for future care needs and care decisions based on prognosis for the disease.
H.
Support the patient in their healthcare decisions.
I.
Demonstrate professional, respectful demeanor when addressing team members,
J.
K.
patients, ancillary staff, and consultants.
Appear professionally dressed and well groomed.
Completes H&P’s, progress notes and discharge summaries in a timely fashion.
L.
Attends required daily conferences and grand rounds.
M.
M. Responds to pages and floor calls in a timely fashion.
Learning Activities
Attending Rounds Research Conference X Outpatient Clinics
Last Updated April 19, 2013
Multidisciplinary Rounds
Grand Rounds
Sub-Specialty
Conference
Morning Report
X Didactics
Other
Ethics/Comm Conference
Specialty Conference
Noon Conference
X Faculty Supervision
Procedures
X
X
Direct Patient care
Resident Seminar
Journal Club
Readings
Evaluation Methods
X Attending Evaluation
X
X
Program Director
Review
360 ᵒ evaluation
Other
X In-Training Exam
X
Directly Supervised
Procedures
Videotape Review
X
Morning Report
Faculty Supervision and Feedback
X Quarterly Review
Interpersonal and Communication Skills
Objectives: Residents must be able to demonstrate interpersonal and communication skills that result in effective information exchange and teaming with patients, their patients families, and professional associates. Residents are expected to:
A.
Develop patient sensitive skills for interviewing that allow accurate, and complete collection of information regarding symptoms, the family and the community that affect the patient's health and care.
B.
Develop skills in communicating results to patients, their families, other health care providers.
C.
Develop skills in educating patients and their families, in dealing with sensitive issues or patients and families, and in negotiating a plan of investigation and treatment with the patient
D.
and family.
Develop professional relationships with co-workers, consultants, ancillary staff and other professionals to enable assembling of health care teams and mobilization of community resources to optimize care of the patient.
E.
Develop an understanding of the role of the family medicine consultant, and is able to support the patient through the process of consultation, medical evaluation, treatment, rehabilitation and long-term care.
F.
Use professional language and demeanor when communicating with other residents, with Family
Medicine attending physicians, with physicians from other services, with non-physician clinical staff, with non-physician non-clinical staff, and with patients and their families.
G.
Create and sustain a therapeutic and ethically sound relationship with patients.
H.
Use effective listening skills and elicit and provide information using effective nonverbal, explanatory, questioning, and writing skills.
I.
Work effectively with others as a member or leader of a health care team or other professional group.
Learning Activities
Attending Rounds
Multidisciplinary Rounds
Grand Rounds
Sub-Specialty
Conference
Research Conference
Noon Conference
X
X
Outpatient Clinics
Ethics/Comm Conference X Direct Patient care
Specialty Conference Resident Seminar
Journal Club
Last Updated April 19, 2013
Morning Report
X Didactics
Other
Evaluation Methods
X Attending Evaluation
X Faculty Supervision
Procedures
X Readings
X Program Director
Review
X 360 ᵒ evaluation
Other
X Directly Supervised
Procedures
X In-Training Exam
Videotape Review
X
X
Morning Report
Faculty Supervision and Feedback
Quarterly Review
Systems-based Practice
Objectives: Residents must demonstrate an awareness of and responsiveness to the larger context and system of health care and the ability to effectively call on system resources to provide care that is of optimal value. Residents are expected to:
A.
Understand how their patient care and other professional practices affect other health care professionals, the health care organization, and the larger society and how these elements of the system affect their own practice.
B.
Know how types of medical practice and delivery systems differ from one another, including methods of controlling health care costs and allocating resources.
C.
Practice cost-effective health care and resource allocation that does not compromise quality of care.
D.
Advocate for quality patient care and assist patients in dealing with system complexities.
E.
Know how to partner with health care managers and health care providers to assess, coordinate, and improve health care and know how these activities can affect system performance.
Learning Activities
Attending Rounds
X Multidisciplinary Rounds
X
Grand Rounds
Sub-Specialty
Conference
Morning Report
X Didactics
Other
Evaluation Methods
X Attending Evaluation
X Program Dir
Review
360 ᵒ evaluation
X Faculty Supervision
Procedures
X Directly Supervised
Procedures
X In-Training Exam
X
Research Conference
Noon Conference
Videotape Review
X Outpatient Clinics
Ethics/Comm Conference X Direct Patient care
Specialty Conference Resident Seminar
X
X
Journal Club
Readings
Morning Report
Faculty Supervision and Feedback
X Quarterly Review
Last Updated April 19, 2013
Practice-based Learning and Improvement
Objectives: Residents must be able to investigate and evaluate their patient care practices, appraise and assimilate scientific evidence, and improve their patient care practices. Residents are expected to:
A.
Analyze practice experience and perform practice-based improvement activities using a systematic methodology.
B.
Locate, appraise, and assimilate evidence from scientific studies related to their patients' health problems.
C.
Obtain and use information about their own population of patients and the larger population from which their patients are drawn.
D.
Apply knowledge of study designs and statistical methods to the appraisal of clinical studies and other information on diagnostic and therapeutic effectiveness.
E.
Use information technology to manage information, access on-line medical information; and support their own education.
G. Learn to incorporate health promotion and disease prevention into patient care.
H. Use evidence-based medicine, evaluation of available evidence, and use of best-
available evidence at morning report meetings and during routine clinical care.
Learning Activities
Attending Rounds
Multidisciplinary Rounds
Grand Rounds
Sub-Specialty
Conference
X Morning Report
X Didactics
Other
Research Conference X Outpatient Clinics
Ethics/Comm Conference X Direct Patient care
Specialty Conference
Noon Conference
X Faculty Supervision
Procedures
X
X
Resident Seminar
Journal Club
Readings
Evaluation Methods
Attending Evaluation
X Program Director
Review
X 360 ᵒ evaluation
Directly Supervised
Procedures
X In-Training Exam
X Videotape Review
X
X
Morning Report
Faculty Supervision and Feedback
Quarterly Review
IV.
Other
Instructional Strategies and Assignments (see above)
A. Self-study: Read Chapters 1-23 in McDonald’s Family-Oriented Primary Care (check out book from Sandra Price during the week preceding the rotation, return it at least one week before the rotation completion).
B.
AFP Monographs: A minimum of 2 topics (see attached) are to be read, post-test taken and
score > 90% during the FPC rotation. Complete the post-tests and turn into Sandra Price at the end of the rotation.
C.
Attend Family Medicine Thursday morning didactics weekly.
Last Updated April 19, 2013
D.
The first week of the rotation, observe at least four patient encounters with faculty seeing their own continuity patients.
E.
See own continuity patients at FMC Dunwoody. Precept each patient in first week and discuss pertinent family/biosychosocial aspects of case. Thereafter, present according to residency guidelines.
F.
Videotaping assignment: videotape 3 or more patient encounters, focusing first on the general flow of the interview and your interviewing techniques, then on the biopsychosocial aspects of the patient’s concerns. In at least two encounters, screening for anxiety and depression should be demonstrated. Be sure and complete signed consent forms from patients.
G.
Home visits assignment: A minimum of 2 home visits on at least two different patients is required to satisfactorily complete this rotation. Write up one case study in the, psychosocial format provided (write-up per attached format 3-5 pages word-processed, doublespaced). Include a genogram and family APGAR. You may hand draw the genogram. The additional (focused) home visits should be written up similar to an office visit and a note put in the chart. Bring a copy of the case report and the shorter notes to your rotation check-out.
H.
End of rotation check out: Review your videotapes ahead of time. Bring your case study write up and videotape to the checkout meeting the final Wednesday afternoon of the rotation at
1:30 pm in the clinic counseling room with the Behavioral Scientist (Dr. Owen or Kara McDaniel) and the rotation coordinator (Dr. Beck at Dunwoody) to discuss them.
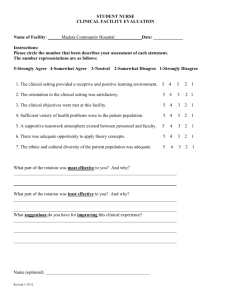
V. Evaluation Strategies (see above)
The resident will be evaluated on the basis of achievement of rotation objectives by preceptors in the
FPC clinic and by the rotation coordinator, with input from Dr. Ashley Owen and Dr. Kara McDaniel.
The written evaluation will be done on the FPC Rotation Evaluation Form.
VI. Attachments
Home Visit Guidelines
Psychosocial Case Study Format
PSYCHOSOCIAL CASE STUDY FORMAT
I. Patient Identification: For confidentiality, write the patient’s name and hospital or clinic #, address and phone number on a separate card. This will be kept separate from the case study.
Initials, first name or pseudonym which will be used to refer to patient in the report
Age
Race/Ethnicity
Gender
II. Medical History *
A. Chief Complaint (or major health problem at this time)
B. HPI (include current medications at end of HPI) **
C. Past Medical History
D. Family (Medical History)
E. Review of Systems
Last Updated April 19, 2013
* While the usual sequence of the medical history calls for the psychosocial history here, for this project it is emphasized more and is separated out from the usual history. It is written up under Part
III.
** If this is a hospital follow-up visit, a summary of the hospitalization is appropriate here.
III. Psychosocial History
A. Demographic data (do not need to repeat identifying data from above)
Marital status and history
Sexual history and preference
Education
Occupational history
Socioeconomic status/financial situation
(Is the current illness creating illness creating financial distress?)
Religious affiliation
Place of birth
Anything unexpected or unique?
B. Family Genogram and APGAR
Draw a genogram of the patient and closest relatives or significant others. Begin with family of procreation (spouse and children).
A suggested technique: Ask the patient to use three words to describe each person on the genogram including himself and 3 words to describe their relationships with the major people in their life.
Do the same for the family of orientation (unless the current nuclear family is greater than 7 people).
Do the family APGAR.
C. Current problems or concerns? This is purposely delayed until here because the genogram may help the patient to identify concerns.
What are they? Is this an excess or deficit in a certain area?
How distressing are these concerns?
How long has the problem(s) been occurring?
What strategies has the person used to cope with the problem?
What is the incentive for change?
Any previous experiences similar to current problem?
D. Background Information
How does the problem fit in the context of the genogram?
If not addressed in the genogram - How does this person relate to others and vice versa?
Non-normative experiences (e.g. usually enriched or impoverished experiences, traumatic events)
E. Current Life Situation
How does person occupy his/her time?
Current stressors, coping strategies, resources
Habits (e.g. eating, drinking, smoking, other drugs, caffeine)
Diet
Exercise
Last Updated April 19, 2013
Romantic / sexual attachments
Close friends / support group
Job situation
Strengths, weaknesses
F. Process Issues
How does this person react to you as a person?
How does he/she communicate his/her concerns (e.g. openly, honestly, avoids expressing feelings)?
What is it like to be in the room with this person? (Do you like / dislike him/her?)
G. Socioeconomic Environment
Past (Education, occupation, religion, economic status, discipline, and
housing while growing up.)
Current (Economic status, Housing, Transportation)
IV. Assessment
A. Problem List (from the Medical and Psychosocial History)
B.
CONCLUSIONS
Your conclusions should be a discussion of your assessment of the psychosocial functioning of this person, and how that psychosocial ffunctioning interfaces with their organic disease and their overall health. If this is not readily derived from the data you’ve collected, formulating answers to the following questions will complete this section.
1.
What is this person’s model of the world?
2.
What behaviors (excesses or deficits) or attitudes does this person have that contribute to or alleviate his major psychological and/or medical problem(s)?
3.
What background factors (genetic or environmental) may have contributed to this person’s current problems?
V. PLAN
Here, list some specific suggestions to improve the patient’s psychosocial situation, e.g. if he
smokes, don’t say “quit smoking” – say “enroll in a smoking cessation program.”
If you think marital or personal therapy/counseling would be beneficial, say so.
If nutrition, housing, or finances are significantly problematic, indicate possible resources.
Last Updated April 19, 2013
Revised 4/11/2020
Home Visit Guidelines
Roles/Indications for Home Visits
Home visits may be indicated for several reasons:
To follow-up after a recent hospitalization
A patient is home-bound
To assess the patient’s home and family environment (for safety, prevention, medically, psychosocially, or all of these)
To assess the patient and family’s readiness and response to changes, such as an addition to the family or a major change in health status of a family member
To provide palliative and supportive care to a terminally ill patient and family
Remember, to make best use of the home visit, concentrate on information and observations that couldn’t be gathered just as well in the clinic setting. Examples are assessing the patient’s system for handling (remembering) medications, the patient’s capability of performing ADL’s (activities of daily living), the risks of falls in the elderly or disabled, attitude, roles and involvement of family members.
Home Visit Practical Guidelines
1.
Exercise reasonable caution.
2.
Get good directions. Take a map. Go in daylight.
3.
Go as part of a team, taking a medical student or a fellow resident along, or contact
Social Services or one of the Home Health Agencies and arrange to make a visit with them.
4.
Limit the amount of personal belongings and valuables you carry.
5.
Confirm the visit ahead of time by telephone.
Home Visit Requirements
A minimum of 4 home visits are required to satisfactorily complete the Residency
Training program (and meet accreditation requirements). Try to complete at least 2 of
these during the Family Practice Center month rotation. One of the patients visited will be the subject of the biopsychosocial case study report. The remaining 3 (to make the total of 4) home visits are to be completed before the end of the second year of training.
You may visit one patient more than once, but must visit at least two different patients during your training. Be sure to report the total number of home visits done during the FPC month to the rotation liaison. A procedure card is to be completed and turned in for each home visit.
Supervision for Home Visits
The home visits made during this rotation emphasize the psychosocial aspects of health. If questions or problems which arise the hospital Attending Faculty is available.
Identification of Patients for Home Visits
1.
Identify patients in your continuity clinic who may benefit from a home visit for any of the reasons outline above. One home visit should be on a prenatal patient and then a second visit after the birth of the child should be done.
2.
You will be assigned to perform home visits on those patients being discharged from the inpatient service
who need a home visit
(during your FPC rotation). Check with the Family Medicine team to anticipate this. If the patient has an on-going need for home visits, you may be expected to pick them up and follow them, if they don’t have a primary provider
3.
Colleagues or the faculty may recommend patients whom are suitable for home visits.
Last Updated April 19, 2013
Revised 4/11/2020
4.
For those of you interested in visiting rural patients, contact the following people to make arrangements. If you choose the rural visit option, your clinic schedule should be arranged ahead of time to give you one entire day out of clinic on one or more days of the rotation.
Last Updated April 19, 2013