North Trent Neonatal Network Clinical Guideline Template
advertisement

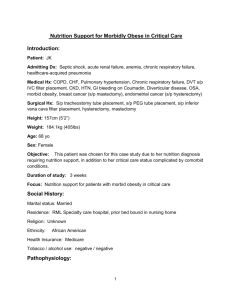
North Trent Neonatal Network Clinical Guideline Title: Parentral Nutrition Guideline Index Number/other identifier: Author: Dr Chris Vas (ST5 Paediatrics), Christine Nye (Senior Pharmacist) Date written: October 2013 Review date: October 2016 This clinical guideline has been developed to ensure appropriate evidence based standards of care throughout the North Trent Neonatal Network. The appropriate use and interpretation of this guideline in providing clinical care remains the responsibility of the individual clinician. If there is any doubt discuss with a senior colleague. Best practice recommendations represent widely used evidence-based practice and high quality standards that all Neonatal Units across the Network should implement. Subsequent suggested recommendations may be put into practice in local units. However, alternative appropriate local guidelines may also exist. A. Guideline Summary 6) Summary Who gets TPN? Infant <1Kg infant < 1.5 Kg with absent EDF Infant < 1.5 Kg and less than 50% of expected enteral feed All Infant <1.5 Kg with central acess TPN day 1 TPN day 1 TPN day 3 TPN day 1 TPN Regimen: Amino Acids (g/kg) 1 2 DAY 2 3 3 3 4 3.5 5 3.5 6 3.5 7 4 Carbohydrates (mg/kg/min) 6 8 8 8 9 9 10 8.64 1 0.5 11.52 2 0.5 11.52 3 Potassium (mmol/kg) 0 0 Phosphate (mmol/kg) 0.5 0.5 1.5 1.5 1.5 1.5 1.5 Calcium (mmol/kg) 1.5 1.5 1.5 1.5 1.5 1.5 1.5 Magnesium (mmol/kg) 0.3 0.3 0.3 0.3 0.3 0.3 0.3 Heparin 0.5 units/mL of aqueous soln 0.5 0.5 0.5 0.5 0.5 0.5 0.5 Acetate (mmol/kg) Start as soon as able Solivito N (mL/kg) 1 1 1 1 1 1 1 Vitlipid Infant (mL/kg) Peditrace (mL/kg) 4 1 4 1 4 1 4 1 4 1 4 1 4 1 Carbohydates (g/kg/day) Fat (g/kg) Sodium (mmol/kg) 11.52 12.96 12.96 3.5 4 4 According to U & E’s According to U & E’s Day 1 is used for infants less than 24 hours of age for the purpose of this guideline. B. 14.4 4 Full guideline 1) Background Total Parenteral Nutrition (TPN) is an effective way of maintaining nutrition in infants who cannot be fed or who will be slow establishing enteral feeds in the first days of life. Preterm infants have low calorific reserves (<4 days in infants <1000g) and maintaining nutrition is an essential part of intensive care. The risks of TPN include line infections, metabolic disturbances and cholestatic jaundice and these risks need to be balanced against the benefits. As the benefits require TPN to be used for at least 7 days, TPN should not be used unless the infant is unlikely to be on full enteral feeds by day 7. TPN is also important in maintaining nutrition in infants with necrotising enterocolitis and infants with short bowel syndrome, where enteral feeding is harmful or not tolerated. 2) Aim The aim of this guideline is to provide a standardised approach to the use of TPN in neonates across the region. 4) Guideline and Evidence – ref to grading system Early randomized trials (1) showed that parenteral nutrition improved survival by 40% in neonates of 28-30 weeks gestation with respiratory distress syndrome (RDS). TPN is also associated with shorter hospital stay (1). Full nutrition requirements can be safely started on the first day of life (2). Clinical Practice issues: 4.1 Who is eligible for TPN? All neonates < 1 Kg or <1.5 Kg with absent end diastolic flow (EDF) should start on first day of life. Neonates less than 1.5 Kg who are on less than 50% enteral feeds by day 3. Neonates less than 1.5 Kg with central access should start on first day of life. Neonates who cannot have enteral feeds for a prolonged period of time e.g. NEC and surgical patients. 4.2 Venous access for TPN: Umbilical vessels can be used for TPN (3). UVC compared to peripheral venous long line catheter reduces insertion attempts with no increase in risk of infection or necrotising enterocolitis (4). The risk of complication may increase if umbilical venous catheters are being left in place for more than 14 days (5, 6). Peripherally inserted long lines should be used to provide central venous access in neonates receiving prolonged PN, as long line use results in improved nutrient intake and fewer insertion attempts (3) . Peripheral veins can be used for short term but a peripheral PN solution is required. There is increased risk of extravasation injuries and nutrition is suboptimal. Central lines are therefore the preferred route for TPN however peripheral TPN may be of benefit for some neonates such as those awaiting central access. For neonates requiring long term TPN, vascular access can become difficult and the need for more permanent access such as broviac lines may need discussing with the surgical team. Recommendation: TPN should be administered via central venous access 4.3 TPN regimen The volume of TPN administrated depends on the daily volume required for individual neonates. 4.3.1 Protein/amino acids Amino acid solution (e.g. Vaminolact®, Primene®) is used to meet protein requirements of neonates. Start at 2g/kg/d and increase to 3g/kg/day on day 2, 3.5g/kg/d on day 4 and can be increased further to 4g/kg/d from day 7. A study by Ibrahim et al (2) showed very low birth rate infants could tolerate 3.5g/kg/day with no adverse effects. Tsang et al (7) showed nitrogen retention can be obtained with a nitrogen intake equivalent to about 3.8g/kg/day thus promoting growth. Recommendation: Amino Acids should be quickly increased to 3.5g/kg/day to promote growth and increased further to 4g/kg/day in extremely premature infants. (A) 4.3.2 Carbohydrates Glucose is the carbohydrate used in TPN. It should be used to provide 6075% of non-protein calories (8). 1g of glucose = 4 calories. Prescribed in mg/kg/min. (10mg/kg/min = approx 15g/kg/day) Start at 6mg/kg/min and increase to 10mg/kg/min (11). Can be increased to a maximum of 12mg/kg/min if tolerated and required. In the presence of hyperglycaemia there is no evidence suggesting reducing carbohydrate content is favorable to starting insulin therapy. 2 small studies have shown insulin therapy can improve calorie intake and weight gain with no adverse effects (12). Recommendation: Start carbohydrates at 6mg/kg/min and increase to 10mg/kg/min.(D) Recommendation; No evidence suggesting best management of hyperglycemia for neonates on TPN. Clinical decision based on individual basis. (B) 4.3.3 Lipids Lipids are a concentrated source of energy and essential fatty acids. The triglyceride portion is hydrolysed to free fatty acids. Lipids provide high energy needs without carbohydrate overload. If the rate of lipids exceeds hydrolysis then the triglyceride level will rise. Start at 1g/kg/d and increase daily by 1g/kg/day to 3g/kg/d. It is increased gradually as there are concerns about neonate’s toleration of lipids. If tolerated, it can then be increased to a maximum of 4g/kg/d. 1g of lipids = 10kCal The amount of fat tolerated by infants is difficult to determine. Triglycerides levels are used as a marker of tolerance. A triglyceride level greater than 2.8 mmol/l is a sign of intolerance. Tolerance is improved by running lipid infusions over 24 hours. There is no evidence to suggest reducing lipids in neonates who are septic. It is worth monitoring tolerance by testing triglyceride levels more frequently and adjusting lipids depending on the levels. Recommendation: Start lipids at 1g/kg/day and increase daily up to maximum of 4g/kg/day.(B) Recommendation: If Triglycerides level are >2.8 mmol/L then lipids should be reduced and Triglycerides levels monitored closely. (D) Recommendation: No need to stop lipids in septic neonates. (C) 4.3.4 Vitamins 1ml/kg/day of solivito added to the amino acid/carbohydrate solution and 4mls/kg day of vitlipid added to the lipid solution provides a full range of water and fat soluble vitamins. Solivito N (FK): 1/10th vial per kg provides per kg/day: Thiamine (B1) 0.32 mg Riboflavin (B2) 0.36 mg Nicotinic acid 4.0 mg Vitamin B6 0.4 mg Pantothenic acid 1.5 mg Biotin 6.0 micrograms Folic acid 0.04 mg Vitamin B12 0.5 micrograms Vitamin C 10.0 mg Vitlipid N Infant (FK): 4 ml/kg (to a maximum daily dose of 10 ml) is added to the lipid solution Infants <2.5 kg will receive 4 ml/kg, providing per kg per day: Vitamin A 276 micrograms (920 iu) Vitamin D 4.0 micrograms (160 iu) Vitamin E 2.56 mg (2.8 iu) Vitamin K 80 micrograms Infants >2.5 kg will receive 10 ml daily, providing a total daily intake of: Vitamin A 690 micrograms (2300 iu) Vitamin D 10 micrograms (400 iu) Vitamin E 6.4 mg (7 iu) Vitamin K 200 micrograms Recommendation: Optimal doses of vitamins have not been established and they are based on expert opinions. (D) 4.3.5 Electrolytes Sodium- Minimal amounts in first 48 hours as need to allow for contraction of extra vascular space without affecting intravascular volume, whilst allowing phosphate to be provided as a salt. Sodium then added depending on blood results and clinical status. Potassium- None in first 48 hours. Potassium then added depending on blood results and clinical status. Usually once neonate has entered the diuresis phase. If a neonate is on insulin then they may require potassium earlier than normal. Phosphate- Commence at 0.5 mmol/kg/d in prepared TPN bags to avoid early hypophosphatemia. Then increase to 1.5-2 mmol/kg/d. Dose may be altered depending on serum phosphate. Be aware that insulin infusions are likely to decrease phosphate levels. Calcium-Start at 1.3-3mmol/kg/d. Dose should be altered depending on serum levels and also the amount of phosphate that is being administrated. Acetate: acetate may used in exchange for chloride e.g. sodium acetate. Its role is to prevent a hyperchloraemia and metabolic acidosis. Acetate requires sodium and potassium in TPN to be added. Acetate has been shown to decrease metabolic acidosis in premature infants (9) and this guideline recommends the addition of acetate in TPN when possible in neonates at risk of metabolic acidosis. The maximum amount of acetate we go up to is 6 mmols/kg- but this depends on the stability of the TPN. Recommendation; Add acetate when possible. 4.3.6 Trace Minerals Peditrace 1ml/kg/day provides a full range of trace minerals and electrolytes Peditrace- Zinc, Copper, Manganese, Selenium, Fluoride, Iodine, Chloride Magnesium sulphate is added routinely at 0.3mmol/kg/d. If serum calcium level is low, need to ensure magnesium levels are adequate. 4.3.7 Heparin A study by Birch et al (10) compared the infection rates of neonates receiving TPN as normal to those with TPN and added heparin. This randomized, controlled double blinded study showed a significant reduction in line infections in neonates receiving TPN with added heparin. Recommendation; 0.5units of heparin/ml of solution should be added. (A) 4.4 TPN monitoring Week 1: Daily U+E/LFT/Bone Profile Subsequent weeks: U+E 2-3/week, Weekly LFT/Bone/Triglycerides/Magnesium Monthly: Selenium/Copper/Zinc/Manganese/Carnitine Selenium- A trace element which patients on long term TPN can become deficient of. Selenium deficiency can cause cardiomyopathy. Selenium can be supplemented orally or intravenously. Copper-Copper deficiency has been found in patients on TPN for longer than a month and can cause neutropenia and anaemia. These can improve with copper supplementation. Zinc-Zinc deficiency has been reported in patients on long term TPN causing a wide range of symptoms which respond to supplementation. Manganese-Long term TPN can cause elevated manganese levels leading to toxicity. Carnitine-This is required for fatty acid oxidation. Whilst on TPN, carnitine levels are known to decrease and supplementation may be warranted although there is no evidence to show this improves growth. 5) Complications 5.1 Infection Full aseptic precautions when inserting and accessing central lines. 5.2 Cholestasis There is an increased risk on cholestasis the longer the duration of parenteral nutrition, the degree of prematurity and the absence of enteral feeding. Even minimal enteral feeding is known to decrease the chance of cholestatic jaundice. IV lipids are a risk factor for PN-associated cholestasis. If cholestasis is present a decrease in lipids should be considered. There is evidence that the use of SMOF decrease PN associated cholestasis and hepatic dysfunction. The ideal timing for starting SMOF needs more research but SMOF should be considered for any neonate expected to be on TPN for longer than 1 month (13). Recommendation; Consider SMOF lipid for neonates requiring TPN longer than 4 weeks or with cholestatic jaundice >40 umol/L. (B). 5.3 Thrombocytopenia This is not a contraindication for TPN, but can be a sign of line infection. 5.4 Acidosis Chloride load is a major factor for metabolic acidosis. Sodium and potassium can be given with acetate and calcium with gluconate to prevent this. 5.5 Hyperbilirubinaemia Lipid emulsions have not been demonstrated to have a significant effect on hyperbilirubinaemia in populations of premature infants. 6) Peripheral venous TPN TPN can be given via peripheral veins but the solution has to be altered for peripheral use. Peripheral TPN provides less nutrition than central TPN. There are increased risks in using TPN peripherally, especially extravasation injuries. Peripheral TPN may be used if central access is awaited and the benefits are felt to outweigh the risks. The Regimen for peripheral TPN is not discussed in this guideline and should be discussed with pharmacy. 7) References 1. Mayer-Mileur L, Chan G: Nutritional support of very-low-birth-weight infants requiring prolonged assisted ventilation. Am J Dis Child 1986; 140: 929–932. 2. Ibrahim HM, Jeroudi MA, Baier RJ, Dhanireddy R, Krouskop RW: Aggressive early total parental nutrition in low-birth-weight infants. J Perinatol 2004; 24: 482–486. 3. Koletzko B, Goulet O, Hunt J, Krohn K, Shamir R. 1. Guidelines on Paediatric Parenteral Nutrition of the European Society of Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) and the European Society for Clinical Nutrition and Metabolism (ESPEN), Supported by the European Society of Paediatric Research (ESPR). Journal of pediatric gastroenterology and nutrition. 2005;41 Suppl 2:S1-87. 4. Loisel DB, Smith MM, MacDonald MG, Martin GR. Intravenous access in newborn infants: impact of extended umbilical venous catheter use on requirement for peripheral venous lines. J Perinatol. 1996;16:461-6. 5. Butler-O'Hara M, Buzzard CJ, Reubens L, McDermott MP, DiGrazio W, D'Angio CT. A randomized trial comparing long-term and shortterm use of umbilical venous catheters in premature infants with birth weights of less than 1251 grams. Pediatrics. 2006;118:e25-35. 6. Seguin J, Fletcher MA, Landers S, Brown D, Macpherson T. Umbilical venous catheterizations: audit by the Study Group for Complications of Perinatal Care. American journal of perinatology. 1994;11:67-70. 7. Tsang, R., Uauy, R., Koletzko, B., Zlotkin, S. (Eds) (2005). Nutrition nd of the Preterm Infant: Scientific Basis and Practical Guidelines (2 ed) Digital Educational Publishing Inc. Cincinnati. 8. ESPEN/ESPGHAN Guidelines on paediatric parenteral nutrition. 9. Olufunmi Peters, Steven Ryan, Linda Matthew, Katherine Cheng, Jenny Lunn . Randomised controlled trial of acetate in preterm neonates receiving parenteral nutrition. Archives of Disease in Childhood 1997;77:F12–F15. 10. Birch P, Ogden S, Hewson M. A randomised, controlled trial of heparin in total parenteral nutrition to prevent sepsis associated with neonatal long lines: the Heparin in Long Line Total Parenteral Nutrition (HILLTOP) trial. Arch Dis Child Fetal Neonatal Ed. 2010 Jul;95(4):F252-7. Epub 2010 Jun 7. 11. Parish A, Bhatia J: Early aggressive nutrition for the premature infant. Neonatology 2008; 94: 211–214. 12. Collins JW, Hoppe M, Brwon K. A Controlled trial of insulin infusion and parenteral nutrition in extremely low birth weigh infants with glucose Mintolerance. J Pediatrics 1991 Jun;118(6):921-7. 13. Mi Attard, N Patel, J Simpson. Change from intralipid to SMOF lipid is associated with improved liver function in infants with PN associated liver disease. Arch Dis Child 2012;97:A54-A55 doi:10. 1136 / archdischild-2012-301885.132